
The Uninsured and the ACA: A Primer
Key Facts about Health Insurance and the Uninsured amidst Changes to the
Affordable Care Act
Prepared by:
Rachel Gareld
Kendal Orgera
Kaiser Family Foundation
and
Anthony Damico
Consultant
January 2019
Table of Contents
Executive Summary ................................................................................................................................. 1
Introduction .............................................................................................................................................. 2
How have health insurance coverage options and availability changed under the ACA? ........................... 3
ACA Coverage Provisions .................................................................................................................... 3
Changes to the ACA under the Trump Administration ........................................................................... 5
How many people are uninsured? ............................................................................................................ 7
Who remains uninsured after the ACA and why do they lack coverage? ................................................. 10
How does lack of insurance affect access to care? ................................................................................. 13
What are the financial implications of lacking insurance?........................................................................ 16
Conclusion ............................................................................................................................................. 18
Endnotes ............................................................................................................................................... 20
The Uninsured and the ACA: A Primer 1
Executive Summary
In the past, gaps in the public insurance system and lack of access to affordable private coverage left
millions without health insurance, and the number of uninsured Americans grew over time, particularly
during economic downturns. By 2013, the year before the major coverage provisions of the Affordable
Care Act (ACA) went into effect, more than 44 million nonelderly individuals lacked coverage.
1
Under the ACA, as of 2014, Medicaid coverage expanded to nearly all adults with incomes at or below
138% of poverty in states that have adopted the expansion, and tax credits are available for people with
incomes up to 400% of poverty who purchase coverage through a health insurance marketplace. Millions
of people enrolled in ACA coverage, and the uninsured rate dropped to a historic low by 2016. Coverage
gains were particularly large among low-income adults in states that expanded Medicaid.
Despite large gains in health coverage, some people continued to lack coverage, and the ACA remained
the subject of political debate. Attempts to repeal and replace the ACA stalled in summer 2017, but there
have been several changes to implementation of the ACA under the Trump Administration that affect
coverage. In 2017, the number of uninsured rose for the first time since implementation of the ACA to
27.4 million.
2
Those most at risk of being uninsured include low-income individuals, adults, and people of
color. The cost of coverage continues to be the most commonly cited barrier to coverage.
3
Health insurance makes a difference in whether and when people get necessary medical care, where
they get their care, and ultimately, how healthy they are. Uninsured people are far more likely than those
with insurance to postpone health care or forgo it altogether. The consequences can be severe,
particularly when preventable conditions or chronic diseases go undetected. While the safety net of public
hospitals, community clinics and health centers, and local providers provides a crucial health care source
for uninsured people, it does not close the access gap for the uninsured.
For many uninsured people, the costs of health insurance and medical care are weighed against equally
essential needs, like housing, food, and transportation to work, and many uninsured adults report
financial stress beyond health care.
4
When uninsured people use health care, they may be charged for
the full cost of that care (versus insurers, who negotiate discounts) and often face difficulty paying
medical bills. Providers absorb some of the cost of care for the uninsured, and while uncompensated care
funds cover some of those costs, these funds do not fully offset the cost of care for the uninsured.
Under current law, nearly half (45%) of the remaining uninsured are outside the reach of the ACA either
because their state did not expand Medicaid, they are subject to immigrant eligibility restrictions, or their
income makes them ineligible for financial assistance.
5
The remainder are eligible for assistance under
the law but may still struggle with affordability and knowledge of options. Ongoing efforts to further alter
the ACA or to make receipt of Medicaid more restrictive may further erode coverage gains seen under the
ACA. On the other hand, state action to take up the ACA Medicaid expansion could make more people
eligible for affordable coverage. The outcome of current debate over health coverage policy in the nation
and the states has substantial implications for people’s coverage, access, and overall health and well-
being.
The Uninsured and the ACA: A Primer 2
Introduction
The Affordable Care Act (ACA) led to historic gains in health insurance coverage. The ACA builds on the
foundation of employer-based coverage and fills gaps in insurance availability and affordability by
expanding Medicaid for adults with incomes at or below 138% of the federal poverty level ($16,753 per
year for an individual in 2018)
6
and providing premium tax credits to make private insurance in the
individual market more affordable for many with incomes between 100-400% of poverty (between
$12,140 and $48,560 per year for an individual in 2018). Most of the ACA’s major coverage provisions
went into effect in 2014, and millions of people have gained coverage under the law. Despite historic
coverage gains, millions of people continue to lack coverage, and the ACA remained the subject of
political debate. Under the Trump Administration, several changes to ACA implementation have altered
the availability of coverage or likelihood that people will sign up for coverage. In 2017, after years of
decreasing uninsured rates, the US saw coverage gains stall or reverse for some groups. Lack of
coverage reflects the fact that Medicaid eligibility for adults remains limited in states that have not
adopted the expansion, some people remain ineligible for financial assistance for private coverage, and
some still find coverage unaffordable even with financial assistance. Furthermore, ongoing efforts to alter
the ACA or limit Medicaid coverage for some groups may have caused confusion or fear among some
people and led them to drop or forgo coverage. These changes pose a challenge to further reducing the
number of uninsured and may further threaten coverage gains seen in recent years.
The gaps in our health insurance system affect people of all ages, races and ethnicities; however, those
with lower incomes face the greatest risk of being uninsured. Being uninsured affects people’s ability to
access needed medical care and their financial security. As a result, uninsured people are less likely to
receive preventive care and are more likely to be hospitalized for conditions that could have been
prevented.
7
The financial impact can also be severe. Uninsured families struggle financially to meet basic
needs, and medical bills can quickly lead to medical debt.
The Uninsured and the ACA: A Primer provides information on how insurance has changed under the
ACA, how many people remain uninsured, who they are, and why they lack health coverage. It also
summarizes what we know about the impact that a lack of insurance can have on health outcomes and
personal finances and the difference health insurance can make in people’s lives.

The Uninsured and the ACA: A Primer 3
How have health insurance coverage options and
availability changed under the ACA?
In the past, gaps in the public insurance system and lack of access to affordable private coverage left
millions without health insurance. The ACA filled in many of these gaps and provided new coverage
options. Under the ACA, as of 2014, Medicaid coverage has been expanded to nearly all adults with
incomes at or below 138% of poverty in states that have adopted the expansion, and tax credits are
available for people with incomes up to 400% of poverty who purchase coverage through a health
insurance marketplace. These new coverage options have increased access to health insurance and
health care for millions, but recent actions may affect coverage options and people’s likelihood of signing
up for or retaining ACA coverage.
ACA Coverage Provisions
The ACA’s coverage provisions
built on and attempted to fill gaps
in a piecemeal insurance system
that historically left many without
affordable coverage. In the past,
many people did not have access to
affordable private coverage or were
ineligible for public coverage. Poor
and low-income adults were
particularly likely to lack coverage,
and the main reason that most people
said they lacked coverage was
inability to afford the cost.
8
The ACA
aimed to provide coverage options
across the income spectrum by filling
in gaps in eligibility for public coverage, access to employer coverage, and availability of affordable non-
group coverage (Figure 1).
9
The ACA expanded Medicaid eligibility to low-income adults, eliminating categorical restrictions
on coverage in states that have expanded their programs. Medicaid and CHIP have long been
important sources of coverage for low-income children and people with disabilities, but in the past,
coverage for parents was limited to those with very low incomes (often below 50% of the poverty level),
and adults without dependent children—regardless of how poor—were ineligible.
10
The ACA expanded
Medicaid eligibility to nearly all adults with income at or below 138% of poverty. The 2012 Supreme Court
ruling effectively made the expansion a state option. As of January 2019, 37 states,
including DC, had
adopted Medicaid expansion under the ACA,
11
and over 12 million people were covered through the ACA
Medicaid expansion.
12
Figure 1
Major Sources of Health Insurance Coverage for the
Nonelderly Population under the Affordable Care Act
Traditional
Medicaid/CHIP
ACA Medicaid
Expansion
Employer-Sponsored
Insurance
ACA Marketplaces
Non-group Market
ACA
Market
Reforms
Higher
Income
Lower
Income
The Uninsured and the ACA: A Primer 4
The ACA established health insurance marketplaces where individuals and small employers can
purchase non-group insurance, often with a subsidy. Very few people were covered by non-group
health insurance policies prior to the ACA, as such policies could be prohibitively expensive or
restrictive.
13
Under the ACA, health insurance marketplaces where individuals can shop for health
coverage operate in each state.
14
To make coverage purchased in these new marketplaces affordable,
the federal government provides tax credits for people with incomes between 100% and 400% of poverty.
Tax credits are available on a sliding scale based on income and limit premium costs to a share of
income. In addition, ACA allows for cost-sharing subsidies to reduce what people with incomes between
100% and 250% of poverty have to pay out-of-pocket to access health services. In 2018, more than 10
million people enrolled in marketplace plans, and the vast majority received financial assistance with their
coverage.
15
A small number of people still purchase non-group coverage outside the marketplace.
16
The ACA includes provisions to promote employer-based coverage. The availability and affordability
of employer-sponsored coverage has declined over time. From 2008 to 2013, the share of firms that
offered workers health benefits declined from 63% to 57%, and health insurance premium increases
outpaced growth in workers’ earnings and overall inflation.
17
Under the ACA, large and medium-size
employers (those with 50 or more full-time equivalent employees) are assessed a fee per full-time
employee (up to $2,320 in 2018) if they do not offer affordable coverage and have at least one employee
who receives a marketplace premium tax credit. To avoid penalties, employers must offer insurance that
pays for at least 60% of covered health care expenses, and the employee’s share of the individual
premium must not exceed a set share of family income (9.86% in 2019).
18
,
19
In addition, the ACA
established the Small Business Health Options Program (SHOP) marketplace to help small employers
and their workers access affordable health coverage.
20
Offer, eligibility, and take-up rates of employer-
sponsored insurance have largely stabilized since 2013,
21
and employer coverage remains the largest
source of health coverage for the nonelderly (covering 153 million people in 2017).
22
The ACA also extends dependent coverage in the private market. In the past, young adults (age 19-
26) were at particularly high risk of being uninsured, largely due to their low incomes and difficulty
affording coverage. As of 2010, young adults may remain on their parents’ private plans (including non-
group and employer-based plans) until age 26. This provision led to drastic decline in the young adult
uninsured rate from 32% in 2010 to 14% in 2017.
23
The ACA included nationwide insurance regulations to improve access to coverage for those who
may have been previously denied coverage and set new requirements for benefits and cost
sharing in ACA plans. Prior to the ACA, in many states, premiums in the non-group market could vary
by age or health status, and people with health problems or at risk for health problems could be charged
high rates, offered only limited coverage, or denied coverage altogether. The ACA included new rules for
insurers prevent them from denying coverage to people for any reason, including their health status, and
from charging people who are sick more (though insurers can, within limits, still charge older people more
for coverage). In addition, the ACA established a minimum “essential health benefits” package for
marketplace plans, Medicaid expansion enrollees, and some employer plans.
The Uninsured and the ACA: A Primer 5
Under the ACA, almost all people were required to have health insurance coverage or be subject
to a tax penalty. This requirement was intended to encourage healthier individuals to purchase coverage
through the marketplace. The requirement only applied to those with access to affordable coverage,
defined as costing no more than 8% of an individual’s or family’s income (certain other exemptions to the
mandate also were granted). The penalty from 2016 to 2018 was assessed as 2.5 percent of family
income, with both a minimum and maximum.
24
Coverage for immigrants remains limited under the ACA. Lawfully-present immigrants can receive
coverage through the ACA marketplaces, but they continue to face eligibility restrictions in Medicaid that
have been in place since prior to the ACA. Specifically, many lawfully present non-citizens who would
otherwise be eligible for Medicaid remain subject to a five-year waiting period before they may enroll.
25
Undocumented immigrants are ineligible for Medicaid and are prohibited from purchasing coverage
through a marketplace or receiving tax credits.
Changes to the ACA under the Trump Administration
With the change in Administration in January 2017, there was renewed debate over the future of the ACA.
Discussion of ACA repeal and public comments from President Trump declaring the law to be “dead” and
“finished,”
26
led some people to be confused about whether the law remained in effect.
27
In addition,
reduced funding for outreach and enrollment assistance programs led to reduction in these services.
28
While attempts to repeal and replace the ACA stalled out in summer 2017, there have been several
changes to implementation of the ACA that affect coverage options and people’s likelihood of signing up
for or retaining ACA coverage.
In October 2017, the Trump Administration announced it would no longer make payments to
insurers for cost-sharing reductions (CSRs). Regardless of whether the federal government
reimburses insurers for CSR subsidies, insurers are still legally required under the ACA to offer reduced
cost-sharing via silver-level plans to eligible consumers. Many built the loss of CSR payments into their
premiums for silver plans for 2018 and again in 2019.
29
,
30
Because premium tax credits on the
exchanges are tied to the cost of silver premiums, the effect of the loss of CSR payments was cushioned
for many enrollees purchasing insurance through the ACA marketplace.
The individual mandate is no longer in effect as of 2019. As part of tax reform legislation passed in
December 2017, Congress reduced the individual mandate penalty to $0 effective in 2019. Repeal of the
individual mandate is expected to deter healthier people from enrolling in coverage and thus lead to a
sicker—and more expensive—risk pool in the marketplace. Analysis of insurer rate filings shows that
plans increased marketplace premiums to account for the loss of the individual mandate.
31
Because
customers receiving marketplace subsidies will continue to pay sliding-scale premiums based largely on
their incomes, these premium increases primarily affect unsubsidized customers and those purchasing
individual coverage outside the ACA marketplace. In December 2018, a federal judge in Texas ruled that
the change to the law’s individual mandate made the entire law itself unconstitutional, though that
decision has no effect as the case works its way through the appeals process.
The Uninsured and the ACA: A Primer 6
New, more loosely-regulated plans may now compete with ACA marketplace plans. In 2018, the
Trump administration announced new rules that will allow more loosely regulated plans – both short-term
limited duration (STLD) plans and association health plans (AHPs) – to proliferate on the individual
market in competition with ACA-compliant coverage.
32
These more loosely regulated plans will serve as a
more affordable option for some people who are not eligible for the ACA’s premium tax credits. However,
particularly in the case of short-term plans, this lower-cost coverage is generally unavailable to people
with pre-existing conditions, and the plans often exclude coverage for certain services.
33
These plans will
attract disproportionately healthy individuals away from ACA-compliant coverage, thus having an upward
effect on premiums in the ACA-compliant individual market.
In 2018, the Centers for Medicare and Medicaid Services (CMS) issued new guidance regarding
Medicaid waivers and invited states to develop waivers, including some that restrict Medicaid
eligibility and enrollment.
34
Under the previous administration, CMS approved certain eligibility- and
enrollment-related waiver provisions as part of ACA Medicaid expansion waivers. Under the Trump
administration, states are seeking to apply these previously approved provisions as well as new
restrictions to both expansion and traditional Medicaid populations. The Trump administration also has
approved eligibility and enrollment restrictions that have never been approved before, such as
conditioning eligibility on meeting work requirements; coverage lock-outs for failure to report changes
affecting eligibility; and eliminating retroactive coverage for nearly all Medicaid enrollees, among others.
In some states, these provisions apply to both expansion adults and traditional Medicaid populations.
New public charge rules could have a chilling effect on coverage among immigrants. In October
2018, the Trump Administration published a proposed rule that would make changes to “public charge”
policies. Under longstanding policy, the federal government can deny an individual entry into the U.S. or
adjustment to legal permanent resident (LPR) status (i.e., a green card) if he or she is determined likely to
become a public charge. Under the proposed rule, officials would newly consider use of certain previously
excluded programs, including Medicaid, in public charge determinations. The changes would likely lead to
decreases in participation in Medicaid among legal immigrant families and their U.S.-born children
beyond those directly affected by the changes.
35
The effect of these policy changes on enrollment and coverage is currently playing out and will
continue to develop. After growing for the first few years of ACA implementation, marketplace
enrollment declined slightly in 2017 and 2018 then dropped substantially in 2019.
36
In the one state that
has implemented Medicaid work requirements to date, Arkansas, over 18,000 people lost Medicaid in
2018 for failing to meet work or reporting requirements;
37
it is unclear whether these people gained other
sources of coverage, but low offer rates of employer coverage among low-wage workers make it likely
that many did not.
38
In addition, recent research suggests that changes in immigration policy focused on
restricting immigration and enhancing immigration enforcement are causing some immigrant families to
turn away from public programs, including Medicaid and CHIP.
39
As additional data on health coverage
becomes available, it will be important to assess the effect of these changes, combined with other
economic trends, on health coverage.

The Uninsured and the ACA: A Primer 7
How many people are uninsured?
Before the ACA, the number of uninsured Americans grew over time, particularly during economic
downturns. By 2013, the year before the major coverage provisions of the ACA went into effect, more
than 44 million people lacked coverage.
40
Under the ACA, millions of people have gained health
coverage, and the uninsured rate dropped to a historic low in 2016. Coverage gains were particularly
large among low-income people living in states that expanded Medicaid. However, for the first time since
the implementation of the ACA, the number of people remaining without coverage increased by half a
million in 2017, reaching 27.4 million.
Under the ACA, the uninsured rate
and number of uninsured people
declined to a historic low by 2016.
The number of uninsured people and
the share of the nonelderly population
that was uninsured rose from 44.2
million (17.1%) to 46.5 million
(17.8%) between 2008 and 2010 as
the country faced an economic
recession (Figure 2). As early
provisions of the ACA went into effect
in 2010, and as the economy
improved, the number of uninsured
and uninsured rate began to drop,
hitting 44.4 million (16.8%) in 2013.
When the major ACA coverage provisions went into effect in 2014, the number of uninsured and
uninsured rate dropped dramatically and continued to fall through 2016 to 26.7 million (10.0%).
41
Overall,
nearly 20 million more people had coverage in 2016 than before the ACA was passed.
Coverage gains through 2016 were
largest among low-income people,
people of color, and adults—
groups that had high uninsured
rates prior to 2014—and were
particularly large in states that
expanded Medicaid. While
uninsured rates decreased across all
income groups from 2013 to 2016,
they declined most sharply for poor
and near-poor people, dropping by
9.7 percentage points and 11.4
percentage points, respectively
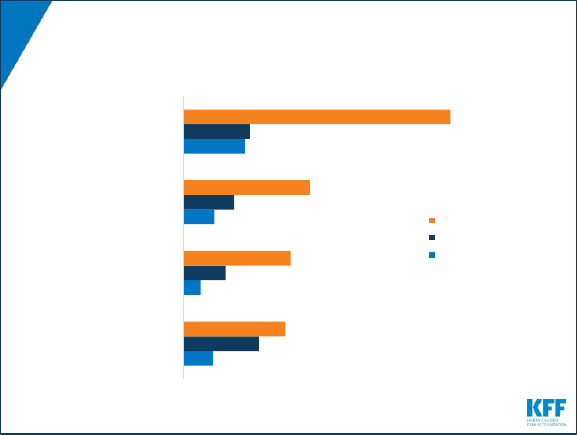
(Figure 3). Among racial and ethnic
Figure 3
-9.7%
-11.4%
-4.5%
-5.3%
-8.2%
-10.9%
-8.6%
-2.9%
-8.4%
-7.4%
-5.9%
Change in Uninsured Rate Among the Nonelderly
Population by Selected Characteristics, 2013-2016
NOTE: Includes nonelderly individuals ages 0 to 64. Asian includes Native Hawaiians and Other Pacific Islanders (NHOPIs).
SOURCE: Kaiser Family Foundation analysis of 2013 & 2016 American Community Survey (ACS), 1-Year Estimates.
Poverty Level
(% of FPL)
Race/Ethnicity Age Group
<100%
100-
199%
>200% White Black Hispanic Asian Children Adults Expanded
Did Not
Expand
State Medicaid
Expansion Status
Figure 2
44.2
45.0
46.5
45.7
44.8
44.4
35.9
29.1
26.7
27.4
17.1%
17.3%
17.8%
17.4%
17.0%
16.8%
13.5%
10.9%
10.0%
10.2%
-
5.0
10.0
15.0
20.0
25.0
30.0
35.0
40.0
45.0
50.0
2008 2009 2010 2011 2012 2013 2014 2015 2016 2017
0.0%
5.0%
10.0%
15.0%
20.0%
25.0%
Number of Uninsured and Uninsured Rate Among
the Nonelderly Population, 2008-2017
NOTE: Includes nonelderly individuals ages 0 to 64.
SOURCE: Kaiser Family Foundation analysis of 2008-2017 American Community Survey (ACS), 1-Year Estimates.

The Uninsured and the ACA: A Primer 8
groups, Hispanics, Blacks, and Asians had particularly large declines in uninsured rates, with each group
seeing a drop of over 8 percentage points from 2013 to 2016 (Figure 3).
42
Because the expansions are
largely targeted to adults, who have historically had higher uninsured rates than children, nearly the entire
decline in the number of uninsured people under the ACA has occurred among adults. Uninsured rates
dropped nearly immediately in expansion states following implementation of the ACA’s coverage
provisions, declining by 7.4 percentage points from 2013 to 2016, with even larger declines among adults
(a 9.2 percentage point drop) widely attributed to gains in Medicaid coverage. Uninsured rates among the
nonelderly population also dropped in non-expansion states following ACA implementation (down 5.9
percentage points), in part as a result of the availability of ACA subsidies for private insurance to those
with incomes above poverty, increased participation among those eligible but not enrolled in Medicaid,
and increased outreach and enrollment efforts surrounding the ACA in all states.
43
In 2017, the uninsured rate
reversed course and, for the first
time since the passage of the ACA,
rose significantly to 10.2%. Groups
that saw significant increases in their
uninsured rate from 2016 to 2017
include Black, non-Hispanics,
children, older adults (age 45-64),
and middle-income families (above
twice the poverty level) (Appendix
Table 1). From 2016 to 2017,
changes in the uninsured rate in the
set of states that expanded Medicaid
were essentially flat overall, declining
by less than 0.1 percentage points,
but patterns varied by states and by demographic group (Figure 4). In contrast, the uninsured rate in
states that did not expand Medicaid increased both overall (rising by 0.6 percentage points) and for most
groups. As with expansion states, changes in coverage from 2016-2017 varied within the set of states
that have not expanded Medicaid.
Figure 4
<0.01%
0.1%
-0.1%*
-0.5%
-0.2%*
0.1%
-0.1%
-0.2%
-0.2%*
0.1%
0.6%*
0.5%*
0.9%
0.1%
0.5%*
0.5%*
0.5%
0.4%*
0.7%*
0.7%*
Total
White
Black
Hispanic
Other race/ethnicity
Children (0-18)
Nonelderly Adults (19-64)
<100% FPL
100%-199% FPL
≥200% FPL
Expansion States
Non-Expansion
States
Change in Uninsured Rate Among the Nonelderly Population
by Selected Characteristics and Expansion Status, 2016-2017
NOTE: * Indicates a statically significant change between 2016 and 2017. Includes nonelderly individuals ages 0 to 64.
SOURCE: Kaiser Family Foundation analysis of 2016 & 2017 American Community Survey (ACS), 1-Year Estimates.
Race/
Ethnicity
Age
Poverty
Level

The Uninsured and the ACA: A Primer 9
Many remain uninsured are eligible
for ACA assistance, but about half
are outside the reach of the ACA.
Of the remaining uninsured in 2017,
more than half (15.0 million, or 55%)
are eligible for financial assistance
through either Medicaid or subsidized
marketplace coverage. However,
nearly half of uninsured people
remain outside the reach of the ACA.
Some (4.1 million, or 15%) are
ineligible due to their immigration
status or their state’s decision not to
expand Medicaid. The remainder of
the uninsured either has an offer of
coverage through an employer or has income above the limit for marketplace tax credits (Figure 5). These
patterns of eligibility vary by state.
44
In the fourteen states that had not expanded Medicaid as of January 2019, 2.5 million poor adults
fall into a “coverage gap.”
45
These adults have incomes above Medicaid eligibility limits in their state
but below the lower limit for marketplace premium tax credits, which begin at 100% of poverty. In non-
expansion states, the median income eligibility level for parents is 43% of poverty and 0% for childless
adults.
46
People in the coverage gap are concentrated in Southern states, with the largest number of
people in the coverage gap in Texas (759,000 people, or 31%) followed by Florida (445,000, or 18%),
Georgia (267,000, or 11%), and North Carolina (215,000, or 9%).
47
Figure 5
Medicaid/
Other Public
Eligible Adult
4.4 M
Medicaid/
Other Public
Eligible Child
2.4 M
Tax Credit
Eligible
8.2 M
In the
Coverage
Gap
2.5 M
Ineligible for
Coverage Due to
Immigration
Status
4.1 M
Ineligible for
Financial
Assistance Due
to ESI Offer
3.8 M
Ineligible for Financial
Assistance Due to Income
1.9 M
Eligibility for ACA Coverage Among Nonelderly
Uninsured, 2017
NOTES: Numbers may not sum to totals due to rounding. Tax Credit Eligible share includes adults in MN and NY who are eligible
for coverage through the Basic Health Plan. Medicaid/Other Public also includes CHIP and some state-funded programs for
immigrants otherwise ineligible for Medicaid.
SOURCE: Kaiser Family Foundation analysis of 2017 American Community Survey (ACS), 1-Year Estimates.
Eligible for
Financial
Assistance
55%
Total = 27.4 Million Nonelderly Uninsured

The Uninsured and the ACA: A Primer 10
Who remains uninsured after the ACA and why do they
lack coverage?
Despite coverage gains, groups with historically high uninsured rates continue to be at highest risk of
being uninsured, including low-income individuals, adults, and people of color. Although most remaining
uninsured people are in working families, cost continues to pose a major barrier to coverage with nearly
half (45%) of uninsured nonelderly adults in 2017 saying that they lacked coverage because it was too
expensive.
48
Though provisions in the ACA aim
to make coverage more affordable
for low and moderate-income
families, these income groups still
make up the vast majority of the
uninsured. Low-income individuals
are at the highest risk of being
uninsured.
49
Nearly half of the
remaining uninsured population
(47%) has family income below 200%
of poverty ($19,730 for a family with
two adults and one child in 2017)
50
and another 35% has family income
between 200 and 399% of poverty
(Figure 6).
A majority of the remaining uninsured population is in a family with at least one worker, and many
uninsured workers continue to lack access to coverage through their job. Not all workers have
access to health coverage through their jobs or can afford the coverage offered to them. In 2017, more
than three-quarters (77%) of the uninsured had at least one full-time worker in their family, and an
additional 10% had a part-time worker in their family (Figure 6).
51
As in the past, low-income workers and
those who work in agriculture, construction, and service jobs are more likely than other workers to be
uninsured.
52
Moreover, not all workers have access to health coverage through their job. In 2017, 71% of
nonelderly uninsured workers worked for an employer that did not offer health benefits to the worker.
53
People of color are at higher risk of being uninsured than Whites. While a plurality (41%) of the
uninsured are non-Hispanic Whites, people of color are disproportionately likely to be uninsured: they
make up 42% of the overall nonelderly U.S. population but account for over half of the total nonelderly
uninsured population (Figure 6). Hispanics and Blacks have significantly higher nonelderly uninsured
rates (18.9% and 11.1%, respectively) than Whites (7.3%).
54
Differences in coverage by race/ethnicity
likely reflect a combination of factors, including language and immigration barriers, income and work
status, and state of residence.
Figure 6
White
41%
Black
14%
Hispanic
37%
Asian/
NHOPI
4%
AIAN
2%
Other
2%
Race
Characteristics of the Nonelderly Uninsured, 2017
NOTE: Includes nonelderly individuals ages 0 to 64. The US Census Bureau’s poverty threshold for a family with two adults and
one child was $19,730 in 2017. Data may not sum to 100% due to rounding. NHOPI refers to Native Hawaiians and Other Pacific
Islanders. AIAN refers to American Indians and Alaska Natives. Persons of Hispanic origin may be of any race; all other
race/ethnicity groups are non-Hispanic.
SOURCE: Kaiser Family Foundation analysis of 2017 American Community Survey (ACS), 1-Year Estimates.
<100%
FPL
18%
100-199%
FPL
29%
200-399%
FPL
35%
400%+
FPL
18%
Family Income
(%FPL)
1 or
More
Full-
Time
Worke
rs
77%
Part-Time
Workers
10%
No
Workers
13%
Family Work Status

The Uninsured and the ACA: A Primer 11
Adults are still more likely than children to be uninsured. Nonelderly adults were more than twice as
likely as children (12% vs. 5%) to be uninsured in 2017.
55
This disparity reflects ongoing differences in
eligibility for public coverage. While the ACA has increased Medicaid eligibility levels for adults, states
have expanded coverage for children even higher through CHIP, while adults without children are
excluded from Medicaid in all but one non-expansion state.
56
Uninsured rates for children are low, and most uninsured children are eligible for Medicaid or
CHIP. Largely due to expanded eligibility for public coverage under Medicaid and CHIP, the uninsured
rate for children is relatively low: in 2017, 5% of children nationwide were uninsured.
57
Over three in five
(64%) uninsured children are eligible for Medicaid, CHIP, or other public programs.
58
Some of these
children may be reached by covering their parents, as research has found that parent coverage in public
programs is associated with higher enrollment of eligible children.
59
,
60
Insurance coverage continues to
vary by state and region, with
individuals living in non-expansion
states being most likely to be
uninsured (Figure 7). In 2017,
thirteen out of the eighteen states
with the highest uninsured rates were
non-expansion states.
61
Economic
conditions, availability of employer-
sponsored coverage, and
demographics are other factors
contributing to variation in uninsured
rates across states.
While most of the uninsured are U.S. citizens, non-citizens continue to be at much higher risk of
being uninsured. In 2017, three out of four (75%) uninsured nonelderly individuals were citizens.
However, non-citizens (including those who are lawfully present and those who are undocumented) are
more likely than citizens to be uninsured in 2017. Among citizens, 8% were uninsured in 2017, compared
to 33% of non-citizens.
62
Cost still poses a major barrier to coverage for the uninsured. Nearly half (45%) of uninsured adults
in 2017 said that they lacked coverage was because of high cost.
63
Though financial assistance is
available to many of the remaining uninsured under the ACA,
64
not everyone who is uninsured is eligible
for free or subsidized coverage. In addition, some uninsured who are eligible for help may not be aware of
coverage options or may face barriers to enrollment.
65
Outreach and enrollment assistance was key to
facilitating both initial and ongoing enrollment in ACA coverage, but these programs face challenges due
to funding cuts and high demand.
66
,
67
Figure 7
Uninsured Rate Among the Nonelderly by State,
2017
NOTE: Includes nonelderly individuals ages 0 to 64.
SOURCE: Kaiser Family Foundation analysis of 2017 American Community Survey (ACS), 1-Year Estimates.
HI
AK
WA
OR
WY
UT
TX
SD
OK
ND
NM
NV
NE
MT
LA
KS
ID
CO
CA
AR
AZ
WI
WV
VA
TN
SC
OH
NC
MO
MS
MN
MI
KY
IA
IN
IL
GA
FL
AL
VT
PA
NY
NJ
NH
MA
ME
DC
CT
DE
RI
MD
<7% (9 States + DC)
7%-10% (23 States)
>10% (18 States)
United States: 10.2%
The Uninsured and the ACA: A Primer 12
Access to health coverage changes as a person’s situation changes. In 2017, 22% of uninsured
nonelderly adults said they were uninsured because the person who carried the health coverage in their
family lost their job or changed employers.
68
More than one in ten were uninsured because of a marital
status change, the death of a spouse or parent, or loss of eligibility due to age or leaving school (11%),
and some lost Medicaid because of a new job/increase in income or the plan stopping after pregnancy
(11%).
69
Most people who remained uninsured nonelderly adults in 2017 were uninsured for more than a
year. Though the share of uninsured who lacked coverage for more than a year decreased from 81% in
2013 to 74% in 2017,
70
the vast majority of uninsured people were still long-term uninsured.
People who
have been without coverage for long periods may be particularly hard to reach through outreach and
enrollment efforts.
The Uninsured and the ACA: A Primer 13
How does lack of insurance affect access to care?
Health insurance makes a difference in whether and when people get necessary medical care, where
they get their care, and ultimately, how healthy they are. Uninsured people are far more likely than those
with insurance to postpone health care or forgo it altogether. The consequences can be severe,
particularly when preventable conditions or chronic diseases go undetected.
Compared to those who have health coverage, people without health insurance are more likely to
skip preventive services and report that they do not have a regular source of health care. Adults
who are uninsured are over three times more likely than insured adults to say they have not had a visit
about their own health to a doctor or
other health professional’s office or
clinic in the past 12 months.
71
They
are also less likely to receive
recommended screening tests such
as blood pressure checks, cholesterol
checks, blood sugar screening, pap
smear or mammogram (among
women), and colon cancer
screening.
72
Part of the reason for
poor access among the uninsured is
that half do not have a regular place
to go when they are sick or need
medical advice, while the majority of
insured people do have a regular
source of care (Figure 8).
73
Uninsured people are more likely than those with insurance to report problems getting needed
medical care. One in five (20%) uninsured adults say that they went without needed care in the past year
because of cost compared to 3% of adults with private coverage and 8% of adults with public coverage.
74
Many uninsured people do not obtain the treatments their health care providers recommend for them. In
2017, 19% of uninsured adults said they delayed or did not get a needed prescription drug due to cost,
compared to 14% with public coverage and 6% with private coverage.
75
And while insured and uninsured
people who are injured or newly diagnosed with a chronic condition receive similar plans for follow-up
care from their doctors, people without health coverage are less likely than those with coverage to obtain
all the recommended services.
76
,
77
Because uninsured people are less likely than those with insurance to have regular outpatient
care, they are more likely to have negative health consequences. Because uninsured patients are
also less likely to receive necessary follow-up screenings than their insured counterparts,
78
they have an
increased risk of being diagnosed at later stages of diseases, including cancer, and have higher mortality
rates than those with insurance.
79
,
80
,
81
In addition, when uninsured people are hospitalized, they receive
Figure 8
6%
3%
6%
11%
14%
8%
9%
12%
19%
20%
24%
50%
Postponed or did not
get needed prescription
drug due to cost
Went without needed
care due to cost
Postponed seeking care
due to cost
No usual source of care
Uninsured
Medicaid/Other Public
Employer/Other Private
Barriers to Health Care Among Nonelderly Adults by
Insurance Status, 2017
NOTE: Includes nonelderly individuals ages 18 to 64. Includes barriers experienced in past 12 months. Respondents who said
usual source of care was the emergency room were included among those not having a usual source of care. All differences
between uninsured and insurance groups are statistically significant (p<0.05).
SOURCE: Kaiser Family Foundation analysis of the 2017 National Health Interview Survey.

The Uninsured and the ACA: A Primer 14
fewer diagnostic and therapeutic services and also have higher mortality rates than those with
insurance.
82
,
83
,
84
,
85
Uninsured children also face
problems getting needed care.
Uninsured children are more likely to
lack a usual source of care, to delay
care, or to have unmet medical needs
than children with insurance (Figure
9).
86
Further, uninsured children with
common childhood illnesses and
injuries do not receive the same level
of care as others and are at higher
risk for preventable hospitalizations
and for missed diagnoses of serious
health conditions.
87
,
88
Among children
with special health care needs, those
without health insurance have worse
access to care than those with
insurance.
89
Lack of health coverage, even for short periods of time, results in decreased access to care.
Research has shown that adults who experience gaps in their health insurance coverage are less likely to
have a regular source of care or to be up to date with blood pressure or cholesterol checks than those
with continuous coverage.
90
Research also indicates that children who are uninsured for part of the year
have more access problems than those with full-year coverage.
91
,
92
Similarly, adults who lack insurance
for an entire year have poorer access to care than those who have coverage for at least part of the
year, suggesting that even a short period of coverage can improve access to care.
93
Research demonstrates that gaining health insurance improves access to health care
considerably and diminishes the adverse effects of having been uninsured. A seminal study of a
Medicaid expansion in Oregon found that uninsured adults who gained Medicaid coverage were more
likely to have an outpatient visit or receive a prescription and less likely to have depression or stress in
the short term than their counterparts who did not gain coverage.
94
Findings two years out from the
expansion showed significant improvements in access, utilization, and self-reported health among the
adults who gained coverage.
95
In addition, a large body of research on the impact of Medicaid expansion
under the ACA demonstrates that gains in Medicaid coverage positively impact access to care and
utilization of health care services.
96
Research also shows that individuals who gained marketplace
coverage in 2014 were far more likely than those who remained uninsured to obtain a usual source of
care and receive preventive care services.
97
Public hospitals, community clinics and health centers provide a crucial health care safety net for
uninsured people; however, the safety net does not close the access gap for the uninsured. Safety
Figure 9
27%
15%
9%
13%
22%
25%
4%
2%
1%
3%
5%
15%
2%
1%
1%
2%
3%
12%
No Usual
Source of Care
Postponed
Seeking Care
Due to Cost
Went Without
Needed Care
Due to Cost
Last MD
Contact
>2 Years Ago
Unmet Dental
Need Due
to Cost
Last Dental Visit
>2 Years Ago
Uninsured Medicaid/Other Public Employer/Other Private
Children’s Access to Care by Health Insurance
Status, 2017
NOTE: Includes children ages 0 to 18. Includes barriers experienced in past 12 months. Respondents who said usual source of
care was the emergency room were included among those not having a usual source of care. All differences between uninsured
and insurance groups are statistically significant (p<0.05).
SOURCE: Kaiser Family Foundation analysis of the 2017 National Health Interview Survey.
The Uninsured and the ACA: A Primer 15
net providers, including public and community hospitals, community health centers, rural health centers,
and local health departments, provide care to many people without health coverage. In addition, nearly all
other hospitals and some private physicians provide some charity care. However, safety net providers
have limited resources and service capacity, and not all uninsured people have geographic access to a
safety net provider.
98
,
99
The ACA has led to significant growth in the number of health centers and their
service capacity through both new grant funds and new patient revenues due to expanded coverage.
100
However, this impact has been more limited in states not expanding Medicaid, where a much larger share
of health center patients remains uninsured than in states that did expand.
101
In addition, health centers in
all states report that securing needed specialty care for their uninsured patients is a major challenge.
102
The Uninsured and the ACA: A Primer 16
What are the financial implications of lacking insurance?
For many uninsured people, the costs of health insurance and medical care are weighed against equally
essential needs, like housing, food, and transportation to work, and many uninsured adults report being
very or moderately worried about paying basic monthly expenses such as rent or other housing costs and
monthly bills.
103
When uninsured people use health care, they may be charged for the full cost of that care
(versus insurers, who negotiate discounts) and often face difficulty paying medical bills. Providers absorb
some of the cost of care for the uninsured, and while uncompensated care funds cover some of those
costs, these funds do not fully offset the cost of care for the uninsured.
Most uninsured people do not receive health services for free or at reduced charge. Hospitals
frequently charge uninsured patients two to four times what health insurers and public programs actually
pay for hospital services.
104
,
105
In 2015, only 27% of uninsured adults reported receiving free or reduced
cost care.
106
Uninsured people often must pay "up front" before services will be rendered. When people without
health coverage are unable to pay the full medical bill in cash at the time of service, they can sometimes
negotiate a payment schedule with a provider, pay with credit cards (typically with high interest rates), or
be turned away.
107
,
108
Among uninsured adults in 2015, a third (33%) were asked to pay for the full cost of
medical care before they could see a doctor.
109
People without health insurance have lower medical expenditures than those with insurance, but
they pay a much larger portion of their medical costs out-of-pocket. Nonelderly people without
health coverage had an average of $1,719 in health spending in 2016, less than half of average annual
spending for people with any private coverage ($4,846) and less than a third of average annual spending
for people with only public coverage ($6,421).
110
Despite lower overall medical spending, people without
insurance who use services pay a greater percentage of their expenses out-of-pocket than those with
insurance. As a result, in 2014, those without insurance who used medical services paid an average of
$752 out of pocket, compared to $658 for those with any private coverage and just $236 for those with
public coverage.
111
Providers incur billions in the cost of uncompensated care for the uninsured, not all of which is
offset by funding to defray these costs. In 2013, before the ACA was fully implemented, the
uncompensated costs of care for the uninsured amounted to about $85 billion, and funding from a
number of sources helped providers defray these costs. Most of these funds came from the federal
government through a variety of programs including Medicaid and Medicare disproportionate share
hospital (DSH) payments, the Veterans Health Administration, the Indian Health Service, the Community
Health Centers block grant, and the Ryan White CARE Act, though states and localities provided billions
and the private sector provided a small share. Given the high cost of hospital-based care, the majority of
the cost of uncompensated care is incurred in hospitals. While substantial, these payments to providers
for uncompensated care amount to a small slice of total health care spending in the U.S.
112

The Uninsured and the ACA: A Primer 17
With the expansion of coverage under the ACA, providers in states that expanded Medicaid are
seeing reductions in uncompensated care costs. For example, between 2013 and 2015, total
uncompensated care costs for hospitals (including charity care costs and bad debt) dropped from $37.3
billion to $28.7 billion, a $8.6 billion or 23% drop.
113
States that expanded Medicaid saw greater declines
in uncompensated care than states that have not expanded.
114
Anticipating fewer uninsured and lower
levels of uncompensated care, the ACA called for a reduction in federal Medicaid DSH payments; these
cuts have been postponed and are now scheduled to begin in 2020.
115
Being uninsured leaves individuals
at an increased risk of financial
strain due to medical bills. In 2017,
nonelderly uninsured adults were
over twice as likely as those with
insurance to have problems paying
medical bills (29% vs. 14%; Figure
10) with nearly two thirds of
uninsured who had medical bill
problems unable to pay their medical
bills at all (65%).
116
Uninsured adults
are also more likely to face negative
consequences due to medical bills,
such as using up savings, having
difficulty paying for necessities,
borrowing money, or having medical
bills sent to collection.
117
Most uninsured people have few, if any, savings or assets they can easily use to pay health care
costs. Uninsured people typically have limited access to funds to finance care. Only 40 and 50 percent of
single- and multi-person households with an uninsured person, respectively, had liquid assets in excess
of $1,000 in 2016, and less than a fifth (18 percent) in both household types had liquid assets above
$5,000.
118
Uninsured nonelderly adults are over twice as likely as insured adults to worry about being able
to pay costs for normal health care (61% vs. 27%; Figure 10). Furthermore, over three quarters of
uninsured nonelderly adults (76%) say they are very or somewhat worried about paying medical bills if
they get sick or have an accident, compared to 45% of insured adults.
119
Uninsured people are at risk of medical debt. Like any bill, when medical bills are not paid or are paid
off too slowly, they are turned over to a collection agency. Nearly three in five consumers (59%) reported
being contacted regarding a collection for medical bills in the United States.
120
In 2017, uninsured adults
were more likely than insured adults to say they have medical bills that are being paid off over time (31%
vs. 24%).
121
More than half (53%) of uninsured people said they had problems paying household medical
bills in the past year.
122
Figure 10
29%
61%
76%
31%
14%
27%
45%
24%
Problems paying or
unable to pay
medical bills
Worried about being
able to pay costs
for normal care
Worried about paying
medical bills if
get sick
Medical bills being
paid off over time
Uninsured Insured
Problems Paying Medical Bills by Insurance Status,
2017
NOTE: Includes nonelderly individuals ages 18 to 64. All differences between uninsured and insured groups are statistically
significant (p<0.05).
SOURCE: Kaiser Family Foundation analysis of the 2017 National Health Interview Survey.

The Uninsured and the ACA: A Primer 18
Conclusion
The ACA led to historic drops in the uninsured rate, with millions of previously uninsured Americans
gaining insurance and access to health services and protection from catastrophic health costs. Prior to
the ACA, the options for the uninsured population were limited in the individual market, as coverage was
often expensive and insurers could deny coverage based on health status. Medicaid and CHIP have
provided coverage to many families, but pre-2014 eligibility levels were low for parents and few states
provided coverage to adults without dependent children. The ACA filled in many of these gaps by
expanding Medicaid to low-income adults and providing subsidized coverage to people with incomes from
100 to 400% of poverty in the marketplaces.
Nonetheless, even with the ACA, the nation’s system of health insurance continues to have many gaps
that currently leave millions of people without coverage, and recent actions to alter the ACA under the
Trump Administration may limit availability of coverage. For the first time since passage of the law, the
number of uninsured people increased in 2017, and 27.4 million remain uninsured. Nearly half (45%) of
the remaining uninsured are outside the reach of the ACA either because their state did not expand
Medicaid, they are subject to immigrant eligibility restrictions, or their income makes them ineligible for
financial assistance. The remainder are eligible for assistance under the law but may still struggle with
affordability and knowledge of options and require targeted outreach to help them gain coverage. Going
without coverage can have serious health consequences for the uninsured because they receive less
preventive care, and delayed care often results in serious illness or other health problems. Being
uninsured can also have serious financial consequences, with many unable to pay their medical bills,
resulting in medical debt.
Ongoing debate about altering the ACA or limiting Medicaid to populations traditionally served by the
program could lead to further loss of coverage and place more people in jeopardy of facing access
barriers or financial strain due to being uninsured. On the other hand, if additional states opt to expand
Medicaid as allowed under the ACA, there may be additional coverage gains as low-income individuals
gain access to affordable coverage. The outcome of current debate over health coverage policy in the
nation and the states has substantial implications for people’s coverage, access, and overall health and
well-being.
Rachel Garfield and Kendal Orgera are with the Kaiser Family Foundation. Anthony Damico is an
independent consultant to the Kaiser Family Foundation.

The Uninsured and the ACA: A Primer 19
Appendix Table 1: Uninsured Rate Among the Nonelderly, 2013-2017
2013
Uninsured
Rate
2016
Uninsured
Rate
2017
Uninsured
Rate
Change in
Uninsured
Rate
2013-2017
Change in
Uninsured
Rate
2016-2017
Total - Nonelderly
a
16.8%
10.0%
10.2%
-6.6%
*
0.2%
*
Age
Children - Total
7.5%
4.7%
5.0%
-2.6%
*
0.3%
*
Adults - Total
20.6%
12.1%
12.3%
-8.2%
*
0.2%
*
Adults 19-25
26.8%
14.6%
14.8%
-11.9%
*
0.2%
Adults 26-34
26.3%
15.6%
15.6%
-10.7%
*
0.0%
Adults 35-44
21.2%
13.6%
13.6%
-7.6%
*
0.0%
Adults 45-54
17.4%
10.4%
10.7%
-6.7%
*
0.3%
*
Adults 55-64
13.4%
7.5%
7.9%
-5.5%
*
0.4%
*
Annual Family Income
<$20,000
28.0%
17.1%
17.2%
-10.8%
*
0.0%
$20,000 - $39,999
27.4%
16.8%
17.3%
-10.1%
*
0.5%
*
$40,000 +
11.4%
7.1%
7.5%
-3.9%
*
0.4%
*
Family Poverty Level
b
<100%
26.2%
16.5%
16.6%
-9.6%
*
0.1%
100-199%
28.4%
17.0%
17.2%
-11.2%
*
0.3%
200-399%
17.7%
11.3%
11.7%
-5.9%
*
0.4%
*
400%+
6.8%
4.1%
4.5%
-2.3%
*
0.3%
*
Household Type
1 Parent with children
c
11.5%
6.8%
7.1%
-4.4%
*
0.3%
2 Parents with children
c
10.8%
6.9%
7.2%
-3.6%
*
0.3%
*
Multigenerational
d
20.5%
11.8%
11.6%
-8.9%
*
-0.2%
Adults living alone or with other adults
20.1%
11.6%
11.8%
-8.3%
*
0.3%
*
Other
22.5%
13.5%
13.6%
-8.8%
*
0.1%
Family Work Status
2+ Full-time
13.4%
8.2%
8.5%
-5.0%
*
0.3%
*
1 Full-time
16.5%
10.2%
10.4%
-6.1%
*
0.2%
*
Only Part-time
e
26.2%
14.4%
14.6%
-11.6%
*
0.2%
Non-Workers
21.2%
12.7%
13.0%
-8.2%
*
0.3%
*
Race/Ethnicity
White only (non-Hispanic)
12.3%
7.1%
7.3%
-5.0%
*
0.3%
*
Black only (non-Hispanic)
18.8%
10.7%
11.1%
-7.7%
*
0.5%
*
Hispanic
30.0%
19.1%
18.9%
-11.1%
*
-0.2%
Asian/Native Hawaiian and Pacific
Islander
15.8%
7.2%
7.2%
-8.6%
*
0.0%
Am. Indian/Alaska Native
30.4%
22.0%
22.0%
-8.4%
*
0.1%
Two or more races
f
13.5%
7.7%
7.9%
-5.6%
*
0.2%
Citizenship
U.S. citizen - native
13.8%
7.9%
8.2%
-5.6%
*
0.3%
*
U.S. citizen - naturalized
20.3%
9.8%
10.0%
-10.3%
*
0.2%
Non-U.S. citizen, resident for < 5 years
38.5%
26.4%
27.2%
-11.3%
*
0.8%
Non-U.S. citizen, resident for 5+ years
51.4%
37.0%
36.0%
-15.4%
*
-1.0%
*
* Indicates a statistically significant difference from 2017 at the p < 0.05 level.
a
Nonelderly includes all individuals under age 65.
b
The U.S. Census Bureau’s poverty threshold for a family with two adults and one child was $19,730 in 2017.
c
Parent includes any
person with a dependent child.
d
Multigenerational families with children include families with at least three generations in a
household. Other families include those with adults are caring for children other than their own (e.g., a niece living with her aunt).
e
Part-time workers are defined as working < 35 hours per week.
f
Respondents can identify as more than one racial or ethnic group.
The hierarchy we use for determining racial/ethnic categories places all respondents who self-identify as mixed race who do not also
identify as Hispanic into the “Two or More Races” category. All individuals who identify with Hispanic ethnicity fall into the Hispanic
category regardless of selected race.
SOURCE: Kaiser Family Foundation analysis of the 2013-2017 American Community Survey (ACS).

The Uninsured and the ACA: A Primer 20
Endnotes
1
Kaiser Family Foundation analysis of 2013 American Community Survey (ACS), 1-Year Estimates.
2
Kaiser Family Foundation analysis of the 2017 American Community Survey (ACS), 1-Year Estimates.
3
Kaiser Family Foundation analysis of the 2017 National Health Interview Survey.
4
Ibid.
5
Kaiser Family Foundation State Health Facts, “Distribution of Eligibility for ACA Health Coverage Among those
Remaining Uninsured as of 2017,” accessed January 2019, https://www.kff.org/health-reform/state-
indicator/distribution-of-eligibility-for-aca-coverage-among-the-remaining-uninsured/.
6
U.S. Department of Health and Human Services, Office of The Assistant Secretary for Planning and Evaluation,
2018 Poverty Guidelines. Available at: https://aspe.hhs.gov/poverty-guidelines.
7
Samuel L Dickman, David Himmelstein, and Steffie Woolhandler, Inequality and the health-care system in the USA
(London, England: The Lancet, April 8, 2017), https://doi.org/10.1016/S0140-6736(17)30398-7.
8
Kaiser Family Foundation analysis of the 2013 Kaiser Survey of Low-Income Americans and the ACA, 2014.
9
Jennifer Tolbert, The Coverage Provisions in the Affordable Care Act: An Update (Washington, DC: Kaiser Family
Foundation, March 2015), https://www.kff.org/report-section/the-coverage-provisions-in-the-affordable-care-act-an-
update-health-insurance-market-reforms/.
10
Tricia Brooks, Karina Wagnerman, Samantha Artiga, and Elizabeth Cornachione, Medicaid and CHIP Eligibility,
Enrollment, Renewal, and Cost Sharing Policies as of January 2018: Findings from a 50-State Survey (Washington,
DC: Kaiser Family Foundation, March 2018), https://www.kff.org/medicaid/report/medicaid-and-chip-eligibility-
enrollment-renewal-and-cost-sharing-policies-as-of-january-2018-findings-from-a-50-state-survey/.
11
Kaiser Family Foundation State Health Facts, “Status of State Action on the Medicaid Expansion Decision,”
accessed January 2019, http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-
the-affordable-care-act/.
12
Kaiser Family Foundation State Health Facts, “Medicaid Expansion Enrollment,” accessed January 2019,
https://www.kff.org/health-reform/state-indicator/medicaid-expansion-enrollment/.
13
Linda J Blumberg, John Holahan, and Erik Wengle, Are Nongroup Marketplace Premiums Really High? Not in
Comparison with Employer Insurance, (Washington, DC: Urban Institute, February 2017),
https://www.urban.org/research/publication/are-nongroup-marketplace-premiums-really-high-not-comparison-
employer-insurance.
14
Some states run their own marketplace, and other state marketplaces are run by the federal government. Kaiser
Family Foundation State Health Facts, “State Health Insurance Marketplace Types, 2018,” accessed January 2019,
http://kff.org/health-reform/state-indicator/state-health-insurance-marketplace-types/.
15
Kaiser Family Foundation, Web Briefing for Journalists: Key Issues Ahead of Marketplace Open Enrollment,
October 2018, https://www.kff.org/health-costs/event/web-briefing-for-journalists-key-issues-ahead-of-marketplace-
open-enrollment/
16
Ibid.
17
Kaiser Family Foundation. 2018 Employer Health Benefits Survey (Washington, DC: Kaiser Family Foundation,
October 2018), https://www.kff.org/health-costs/report/2018-employer-health-benefits-survey/.
18
U.S. Department of the Treasury, Internal Revenue Service, Form Rev. Proc. 2017-36, (Washington, DC: 2017),
https://www.irs.gov/pub/irs-drop/rp-17-36.pdf.
19
U.S. Department of the Treasury, Internal Revenue Service, Form Rev. Proc. 2018-34, (Washington, DC: 2018),
https://www.irs.gov/pub/irs-drop/rp-18-34.pdf.
20
Under the SHOP, employers with no more than 50 full-time equivalent (FTE) employees can purchase coverage
and employers with no more than 25 FTE employees and annual wages below a limit ($53,000 for tax year 2017)
may be eligible for tax credits for up to two years to reduce the cost of SHOP coverage. Beginning in January 2016,
states had the option to expand the SHOP to include employers with 100 or fewer FTEs. For tax years beginning in
2014 or later, employers could receive a tax credit of up to 50% of the employer’s contribution to the premium,
calculated on a sliding scale basis tied to average wages and number of employees. For small businesses with tax-
exempt status meeting the requirements above, the tax credit is 35% of the employer contribution. In order to qualify,

The Uninsured and the ACA: A Primer 21
a business must pay premiums on behalf of employees enrolled in a qualified health plan offered through the SHOP
marketplace or qualify for an exemption to this requirement. “Small Business Health Care Tax Credit and the SHOP
Marketplace,” Internal Revenue Service, accessed December 2018, https://www.irs.gov/affordable-care-
act/employers/small-business-health-care-tax-credit-and-the-shop-marketplace. Centers for Medicare and Medicaid
Services, Health Insurance Marketplace, Who Can Use the SHOP Marketplace (Baltimore, MD: CMS, Health
Insurance Marketplace, October 2014), https://marketplace.cms.gov/outreach-and-education/who-can-use-shop.pdf
21
Kaiser Family Foundation, 2018 Employer Health Benefits Survey, (Washington, DC: Kaiser Family Foundation,
October 2018), https://www.kff.org/report-section/2018-employer-health-benefits-survey-summary-of-findings/.
22
Kaiser Family Foundation State Health Facts, “Health Insurance Coverage of Nonelderly 0-64,” accessed January
2019, https://www.kff.org/other/state-indicator/nonelderly-0-64/.
23
Kaiser Family Foundation analysis of the 2010 and 2017 National Health Interview Survey.
24
“Individual Share Responsibility Provision – Reporting and Calculating the Payment.” ACA Individual Shared
Responsibility Provision Calculating the Payment | Internal Revenue Service. February 2018.
https://www.irs.gov/affordable-care-act/individuals-and-families/aca-individual-shared-responsibility-provision-
calculating-the-payment.
25
Lawfully present immigrants who would be eligible for Medicaid but are in a five-year waiting period are eligible for
tax credits for marketplace coverage. Samantha Artiga and Anthony Damico, Health Coverage and Care for
Immigrants (Washington, DC: Kaiser Family Foundation, July 2017), http://www.kff.org/disparities-policy/issue-
brief/health-coverage-and-care-for-immigrants/.
26
R. Savransky, The Hill, Trump: There is no such thing as Obamacare anymore, October 2017,
http://thehill.com/policy/healthcare/355658-trump-there-is-no-such-thing-as-obamacare-anymore.
27
Ashley Kirzinger, Liz Hamel, Biana DiJulio, Cailey Muñana, and Mollyann Brodie. Kaiser Health Tracking Poll –
November 2017: The Politics of Health Insurance Coverage, ACA Open Enrollment, (San Francisco, CA: Kaiser
Family Foundation, November 2017), https://www.kff.org/health-reform/poll-finding/kaiser-health-tracking-poll-
november-2017-the-politics-of-health-insurance-coverage-aca-open-enrollment/.
28
Karen Pollitz, Jennifer Tolbert, and Maria Diaz. Data Note: Changes in 2017 Federal Navigator Funding,
(Washington, D.C.: Kaiser Family Foundation, October 2017), https://www.kff.org/health-reform/issue-brief/data-note-
changes-in-2017-federal-navigator-funding/.
29
Rabah Kamal, Ashley Semanskee, Michelle Long, Gary Claxton, and Larry Levitt, How the Loss of Cost-Sharing
Subsidy Payments is Affecting 2018 Premiums, (San Francisco, CA: Kaiser Family Foundation, October 2017),
https://www.kff.org/health-reform/issue-brief/how-the-loss-of-cost-sharing-subsidy-payments-is-affecting-2018-
premiums/.
30
Rabah Kamal, Cynthia Cox, Care Shoaibi, Brian Kaplun, Ashley Semanskee, and Larry Levitt, An Early Look at
2018 Premium Changes and Insurer Participation on ACA Exchanges (San Francisco, CA: Kaiser Family Foundation,
August 2017), https://www.kff.org/health-reform/issue-brief/an-early-look-at-2018-premium-changes-and-insurer-
participation-on-aca-exchanges/.
31
Rabah Kamal, Cynthia Cox, Rachel Fehr, Marco Ramirez, Katherine Horstman, and Larry Levitt, How Repeat of
the Individual Mandate and Expansion of Loosely Regulated Plans are Affecting 2019 Premiums, (San Francisco,
CA: Kaiser Family Foundation, October 2018), https://www.kff.org/health-costs/issue-brief/how-repeal-of-the-
individual-mandate-and-expansion-of-loosely-regulated-plans-are-affecting-2019-premiums/.
32
Karen Pollitz and Gary Claxton, Proposals for Insurance Options That Don’t Comply with ACA Rules: Trade-offs in
Cost and Regulation, (Washington, DC: Kaiser Family Foundation, April 2018), https://www.kff.org/health-
reform/issue-brief/proposals-for-insurance-options-that-dont-comply-with-aca-rules-trade-offs-in-cost-and-regulation/.
33
Karen Pollitz, Michelle Long, Ashley Semanskee, and Rabah Kamal, Understanding Short-Term Limited Duration
Health Insurance (Washington, DC: Kaiser Family Foundation, April 2018), https://www.kff.org/health-reform/issue-
brief/understanding-short-term-limited-duration-health-insurance/.
34
MaryBeth Musumeci, Robin Rudowitz, Elizabeth Hinton, Larisa Antonisse, and Cornelia Hall, Section 1115
Medicaid Demonstration Waivers: The Current Landscape of Approved and Pending Waivers, (Washington, DC:
Kaiser Family Foundation, September 2018), https://www.kff.org/report-section/section-1115-medicaid-
demonstration-waivers-the-current-landscape-of-approved-and-pending-waivers-issue-brief/.

The Uninsured and the ACA: A Primer 22
35
Kaiser Family Foundation, Proposed Changes to “Public Charge” Policies for Immigrants: Implications for Health
Coverage, (Washington, DC: Kaiser Family Foundation, September 2018), https://www.kff.org/disparities-policy/fact-
sheet/proposed-changes-to-public-charge-policies-for-immigrants-implications-for-health-coverage/.
36
Kaiser Family Foundation State Health Facts, “Marketplace Enrollment, 2014-2019,” Trend Graph: United States
2014-2019, accessed January 2019, https://www.kff.org/health-reform/state-indicator/marketplace-enrollment.
37
Robin Rudowitz, MaryBeth Musumeci, and Cornelia Hall, Year End Review: December State Data for Medicaid
Work Requirements in Arkansas (Washington, DC: Kaiser Family Foundation, January 2019),
https://www.kff.org/medicaid/issue-brief/state-data-for-medicaid-work-requirements-in-arkansas/.
38
MaryBeth Musumeci, Robin Rudowitz, and Barbara Lyons, Medicaid Work Requirements in Arkansas: Experience
and Perspectives of Enrollees (Washington, DC: Kaiser Family Foundation, December 2018),
https://www.kff.org/medicaid/issue-brief/medicaid-work-requirements-in-arkansas-experience-and-perspectives-of-
enrollees/.
39
Kaiser Family Foundation, In Focus: Immigrant Families, including Immigrants Lawfully in the U.S. and Those Who
Are Undocumented, Report Rising Fear and Anxiety Affecting Their Daily Lives and Health (Washington, DC,
December 13, 2017), https://www.kff.org/disparities-policy/press-release/in-focus-immigrant-families-including-
immigrants-lawfully-in-the-u-s-and-those-who-are-undocumented-report-rising-fear-and-anxiety-affecting-their-daily-
lives-and-health/.
40
Kaiser Family Foundation analysis of 2013 American Community Survey (ACS), 1-Year Estimates.
41
Kaiser Family Foundation analysis of the 2017 American Community Survey (ACS), 1-Year Estimates.
42
Ibid.
43
Kaiser Family Foundation analysis of the 2017 American Community Survey (ACS), 1-Year Estimates.
44
Kaiser Family Foundation State Health Facts, “Distribution of Eligibility for ACA Health Coverage Among those
Remaining Uninsured as of 2017,” accessed January 2019, https://www.kff.org/health-reform/state-
indicator/distribution-of-eligibility-for-aca-coverage-among-the-remaining-uninsured/.
45
Kaiser Family Foundation analysis based on 2017 Medicaid eligibility levels and March 2017 Current Population
Survey, Annual Social and Economic Supplement.
46
Tricia Brooks, Karina Wagnerman, Samantha Artiga, and Elizabeth Cornachione, Medicaid and CHIP Eligibility,
Enrollment, Renewal, and Cost-Sharing Policies as of January 2018: Findings from a 50-State Survey (Washington,
DC: Kaiser Family Foundation, March 2018), https://www.kff.org/medicaid/report/medicaid-and-chip-eligibility-
enrollment-renewal-and-cost-sharing-policies-as-of-january-2018-findings-from-a-50-state-survey/.
47
Kaiser Family Foundation analysis of the 2017 American Community Survey (ACS), 1-Year Estimates.
48
Kaiser Family Foundation analysis of the 2017 National Health Interview Survey.
49
Kaiser Family Foundation analysis of the March 2017 Current Population Survey, Annual Social and Economic
Supplement.
50
“Poverty Thresholds,” U.S. Census Bureau, accessed October 2018, http://www.census.gov/data/tables/time-
series/demo/income-poverty/historical-poverty-thresholds.html.
51
Kaiser Family Foundation analysis of the 2017 American Community Survey (ACS), 1-Year Estimates.
52
See Supplemental Tables, Table 8.
53
Kaiser Family Foundation analysis of the March 2018 Current Population Survey, Annual Social and Economic
Supplement.
54
Kaiser Family Foundation analysis of the 2017 American Community Survey (ACS), 1-Year Estimates.
55
Ibid.
56
Tricia Brooks, Karina Wagnerman, Samantha Artiga, and Elizabeth Cornachione, Medicaid and CHIP Eligibility,
Enrollment, Renewal, and Cost-Sharing Policies as of January 2018: Findings from a 50-State Survey (Washington,
DC: Kaiser Family Foundation, March 2018), https://www.kff.org/medicaid/report/medicaid-and-chip-eligibility-
enrollment-renewal-and-cost-sharing-policies-as-of-january-2018-findings-from-a-50-state-survey/.
57
Kaiser Family Foundation analysis of the 2017 American Community Survey (ACS), 1-Year Estimates.

The Uninsured and the ACA: A Primer 23
58
Other public programs include some state-funded programs for immigrants otherwise ineligible for Medicaid. Kaiser
Family Foundation analysis based on 2018 Medicaid eligibility levels and 2017 American Community Survey, 1-Year
Estimates.
59
Julie L. Hudson and Asako S. Moriya, “Medicaid Expansion for Adults Had Measureable ‘Welcome Mat’ Effects on
Their Children,” Health Affairs 36, no.9 (September 2017): 1643-51.
60
Elisabeth W. Burak, Health Coverage for Parents and Caregivers Helps Children (Washington, DC: Georgetown
University Center for Children and Families, March 2017), https://ccf.georgetown.edu/wp-
content/uploads/2017/03/Covering-Parents-v2.pdf.
61
Kaiser Family Foundation analysis of the 2017 American Community Survey (ACS), 1-Year Estimates.
62
Ibid.
63
Kaiser Family Foundation analysis of the 2017 National Health Interview Survey.
64
Rachel Garfield, Anthony Damico, Kendal Orgera, Gary Claxton, and Larry Levitt, Estimates of Eligibility for ACA
Coverage among the Uninsured in 2016 (Washington, DC: Kaiser Family Foundation, June 2018),
https://www.kff.org/uninsured/issue-brief/estimates-of-eligibility-for-aca-coverage-among-the-uninsured-in-2016/.
65
Ashley Kirzinger, Liz Hamel, Cailey Muñana, and Mollyann Brodie. Kaiser Health Tracking Poll – March 2018: Non-
Group Enrollees, (San Francisco, CA: Kaiser Family Foundation, April 2018), https://www.kff.org/health-reform/poll-
finding/kaiser-health-tracking-poll-march-2018-non-group-enrollees/.
66
Karen Pollitz, Jennifer Tolbert, and Ashley Semanskee. 2016 Survey of Health Insurance Marketplace Assister
Programs and Brokers (Washington, DC: Kaiser Family Foundation, June 2016), http://www.kff.org/health-
reform/report/2016-survey-of-health-insurance-marketplace-assister-programs-and-brokers/
67
Karen Pollitz, Jennifer Tolbert, and Maria Diaz. Data Note: Further Reductions in Navigator Funding for Federal
Marketplace States, (Washington, D.C.: Kaiser Family Foundation, September 2018), https://www.kff.org/health-
reform/issue-brief/data-note-further-reductions-in-navigator-funding-for-federal-marketplace-states/.
68
Kaiser Family Foundation analysis of the 2016 National Health Interview Survey.
69
Ibid.
70
Ibid.
71
Kaiser Family Foundation analysis of the 2017 National Health Interview Survey.
72
Ibid.
73
Ibid.
74
Ibid.
75
Ibid.
76
Jack Hadley, “Insurance Coverage, Medical Care Use, and Short-term Health Changes Following an Unintentional
Injury or the Onset of a Chronic Condition,” JAMA 297, no. 10 (March 2007): 1073-84.
77
Broadwater-Hollifield et al. “Predictors of Patient Adherence to Follow-Up Recommendations after an ED Visit,”
The American Journal of Emergency Medicine 33, no.10 (October 2015): 1368-73.
78
Silvia Tejada et al., “Patient Barriers to Follow-Up Care for Breast and Cervical Cancer Abnormalities.” Journal of
Women's Health 22, no. 6 (June 2013): 507-517.
79
Steffie Woolhandler, et al., “The Relationship of Health Insurance and Mortality: Is Lack of Insurance Deadly?”
Annals of Internal Medicine 167 (June 2017): 424-431.
80
Andrea S. Christopher, et al., “Access to Care and Chronic Disease Outcomes Among Medicaid-Insured Persons
Versus the Uninsured,” American Journal of Public Health 106, no. 1 (January 2016): 63-69.
81
Institute of Medicine, America’s Uninsured Crisis: Consequences for Health and Health Care (Washington, DC:
Institute of Medicine, February 2009),
http://iom.nationalacademies.org/~/media/Files/Report%20Files/2009/Americas-Uninsured-Crisis-Consequences-for-
Health-and-Health-Care/Americas%20Uninsured%20Crisis%202009%20Report%20Brief.pdf.
82
Fizan Abdullah et al., “Analysis of 23 Million US Hospitalizations: Uninsured Children Have Higher All-Cause In-
Hospital Mortality,” Journal of Public Health 32, no. 2 (June 2010): 236-44.

The Uninsured and the ACA: A Primer 24
83
Steffie Woolhandler, et al., “The Relationship of Health Insurance and Mortality: Is Lack of Insurance Deadly?”
Annals of Internal Medicine 167 (June 2017): 424-431.
84
Destini A Smith, et al., “The effect of health insurance coverage and the doctor-patient relationship on health care
utilization in high poverty neighborhoods.” Preventive Medicine Reports 7 (2017): 158-161.
85
Andrea S. Christopher, et al., “Access to Care and Chronic Disease Outcomes Among Medicaid-Insured Persons
Versus the Uninsured,” American Journal of Public Health 106, no. 1 (January 2016): 63-69.
86
Kaiser Family Foundation analysis of the 2017 National Health Interview Survey.
87
Institute of Medicine, America’s Uninsured Crisis: Consequences for Health and Health Care (Washington, DC:
Institute of Medicine, February 2009),
http://iom.nationalacademies.org/~/media/Files/Report%20Files/2009/Americas-Uninsured-Crisis-Consequences-for-
Health-and-Health-Care/Americas%20Uninsured%20Crisis%202009%20Report%20Brief.pdf.
88
Amanda Haboush-Deloye, Spencer Hensley, Masaru Teramoto, Tara Phebus, Denise Tanata-Ashby, “The Impacts
of Health Insurance Coverage on Access to Healthcare in Children Entering Kindergarten,” Maternal and Child Health
Journal 18, no.7 (Sep 2014): 1753-64.
89
MaryBeth Musumeci, Medicaid Restructuring and Children with Special Health Care Needs (Washington, DC:
Kaiser Family Foundation, July 2017), https://www.kff.org/report-section/medicaid-restructuring-and-children-with-
special-health-care-needs-issue-brief/.
90
Sara Collins et al., Gaps in Health Insurance: Why So Many Americans Experience Breaks in Coverage and How
the Affordable Care Act Will Help (The Commonwealth Fund, April 2012),
http://www.commonwealthfund.org/~/media/Files/Publications/Issue%20Brief/2012/Apr/1594_collins_gaps_in_hlt_ins
_tracking_brief_v2.pdf.
91
Amy Cassedy, Gerry Fairbrother, and Paul Newacheck, “The Impact of Insurance Instability on Children’s Access,
Utilization, and Satisfaction with Health Care,” Ambulatory Pediatrics 8, no. 5 (October 2008): 321-8.
92
Thomas Buchmueller, Sean Orzol, and Lara Shore-Sheppard, “Stability of Children’s Insurance Coverage and
Implications for Access to Care: Evidence from the Survey of Income and Program Participation”, International
Journal of Health Care Finance and Economics 14, no.2 (Jun 2014).
93
Salam Abdus, “Part-Year Coverage and Access to Care for Nonelderly Adults,” Medical Care 52, no. 8 (August
2014): 709-14.
94
Amy Finkelstein et al., “The Oregon Health Insurance Experiment: Evidence from the First Year” (National Bureau
of Economic Research, July 2011), http://www.nber.org/papers/w17190.
95
Katherine Baicker et al., “The Oregon Experiment — Effects of Medicaid on Clinical Outcomes,” New England
Journal of Medicine 368 (May 2013): 1713-1722.
96
Larisa Antonisse, Rachel Garfield, Robin Rudowitz, and Samantha Artiga, The Effects of Medicaid Expansion on
the ACA: Updated Findings From a Literature Review (Washington, D.C.: Kaiser Family Foundation, March 2018),
https://www.kff.org/medicaid/issue-brief/the-effects-of-medicaid-expansion-under-the-aca-updated-findings-from-a-
literature-review-march-2018/.
97
James B Kirby and Jessica P. Vistnes,“Access to Care Improved for People Who Gained Medicaid or Marketplace
Coverage in 2014” Health Affairs,35, no.10 (Oct 2016): 1830-1834.
98
Sara Rosenbaum, Jennifer Tolbert, Jessica Sharac, Peter Shin, Rachel Gunsalus, and Julia Zur, Community
Health Centers: Growing Important in a Changing Health Care System, (Washington, DC: Kaiser Family Foundation,
March 2018), https://www.kff.org/medicaid/issue-brief/community-health-centers-growing-importance-in-a-changing-
health-care-system/.
99
Allen Dobson, Joan DaVanzo, Randy Haught, and Phap-Hoa Luu, Comparing the Affordable Care Act’s Financial
Impact on Safety-Net Hospitals in States That Expanded Medicaid and Those That Did Not, (New York, NY: The
Commonweath Fund, November 2017), https://www.commonwealthfund.org/publications/issue-
briefs/2017/nov/comparing-affordable-care-acts-financial-impact-safety-net.
100
Peter Shin et al., Health Center Patient Trends, Enrollment Activities, and Service Capacity: Recent Experience in
Medicaid Expansion and Non-Expansion States, (Washington, DC: Kaiser Commission for Medicaid and the
Uninsured, Dec 2015), http://kff.org/medicaid/issue-brief/health-center-patient-trends-enrollment-activities-and-
service-capacity-recent-experience-in-medicaid-expansion-and-non-expansion-states.

The Uninsured and the ACA: A Primer 25
101
Julia Paradise, Sara Rosenbaum, Anne Markus, Jessica Sharac, Chi Tran, David Reynolds, and Peter Shin,
Community Health Centers: Recent Growth and the Role of the ACA (Washington, DC: Kaiser Family Foundation,
January 2017), https://www.kff.org/medicaid/issue-brief/community-health-centers-recent-growth-and-the-role-of-the-
aca/.
102
Ibid.
103
Kaiser Family Foundation analysis of the 2017 National Health Interview Survey.
104
Gerard Anderson , “From ‘Soak The Rich’ To ‘Soak The Poor’: Recent Trends In Hospital Pricing” Health Affairs 26, no. 4
(May 2007): 780-789.
105
Stacie Dusetzina, Ethan Basch, and Nancy Keating, “For Uninsured Cancer Patients, Outpatient Charges Can Be
Costly, Putting Treatments out of Reach,” Health Affairs 34, no. 4 (April 2015): 584-591.
106
Kaiser Family Foundation analysis of the 2015 Kaiser Family Foundation/New York Times Medical Bills Survey.
107
Brent Asplin et al., “Insurance Status and Access to Urgent Ambulatory Care Follow-up Appointments,” JAMA
294, no. 10 (September 2005): 1248-54.
108
Brendan Saloner, et al., “Most Uninsured Adults Could Schedule Primary Care Appointments Before The ACA,
But Average Price Was $160,” Health Affairs 34, no. 5 (May 2015), https://doi.org/10.1377/hlthaff.2014.1258.
109
Kaiser Family Foundation analysis of the 2015 Kaiser Family Foundation/New York Times Medical Bills Survey.
110
MEPS Summary Tables. Use, expenditures, and population. Available at:
https://meps.ahrq.gov/mepstrends/hc_use/.
111
Roemer, M. I. Out-of-Pocket Health Care Expenses by Insurance Coverage, 2000-2014. Statistical Brief #500.
February 2017. Agency for Healthcare Research and Quality, Rockville, MD.
http://meps.ahrq.gov/mepsweb/data_files/publications/st500/stat500.pdf
112
Ibid.
113
Medicaid and CHIP Payment and Access Commission (MACPAC), Report to Congress on Medicaid and CHIP,
Chapter 3: Annual Analysis of Disproportionate Share Hospital Allotments to States, (MACPAC, March 2018),
https://www.macpac.gov/wp-content/uploads/2018/03/Annual-Analysis-of-Disproportionate-Share-Hospital-
Allotments-to-States.pdf.
114
Ibid.
115
42 U.S.C. § 1396r-4 (f)(7)(A).
116
Kaiser Family Foundation analysis of the 2017 National Health Interview Survey.
117
Liz Hamel, Mira Norton, Karen Pollitz, Larry Levitt, Gary Claxton, and Mollyann Brodie, The Burden of Medical
Debt: Results from the Kaiser Family Foundation/New York Times Medical Bills Survey (Washington, DC: Kaiser
Family Foundation, January 2016), http://www.kff.org/health-costs/report/the-burden-of-medical-debt-results-from-
the-kaiser-family-foundationnew-york-times-medical-bills-survey/.
118
Matthew Rae, Gary Claxton, and Larry Levitt, Do Health Plan Enrollees have Enough Money to Pay Cost
Sharing? (Washington, DC: Kaiser Family Foundation, November 2017), https://www.kff.org/health-costs/issue-
brief/do-health-plan-enrollees-have-enough-money-to-pay-cost-sharing/.
119
Kaiser Family Foundation analysis of the 2017 National Health Interview Survey.
120
Consumer Financial Protection Bureau, “Consumer Experiences with Debt Collection: Findings from the CFPB’s
Survey of Consumer Views on Debt.” (Consumer Financial Protection Bureau: January 2017),
https://www.consumerfinance.gov/data-research/research-reports/consumer-experiences-debt-collection-findings-
cfpbs-survey-consumer-views-debt/.
121
Ibid.
122
Liz Hamel, Mira Norton, Karen Pollitz, Larry Levitt, Gary Claxton, and Mollyann Brodie, The Burden of Medical
Debt: Results from the Kaiser Family Foundation/New York Times Medical Bills Survey (Washington, D.C.: Kaiser
Family Foundation, January 2016), https://www.kff.org/report-section/the-burden-of-medical-debt-section-1-who-has-
medical-bill-problems-and-what-are-the-contributing-factors/.

THE HENRY J. KAISER FAMILY FOUNDATION
Headquarters
185 Berry Street Suite 2000
San Francisco CA 94107
650 854 9400
Washington Ofces and Conference Center
1330 G Street NW
Washington DC 20005
202 347 5270
This publication (#7451-14) is available on the
Kaiser Family Foundation’s website at kff.org.
The Kaiser Family Foundation
is a nonprot organization
based in San Francisco, California.
Filling the need for trusted information on national health issues.
