COVID-19: Clinical Best Practices in
Physical Therapy Management
HOSTS:
Talia Pollok & James Tompkins
PRESENTERS:
Heidi Engel, Christiane Perme, Stephen Ramsey, Ellen Hillegass, Angela Campbell

BIOs
● Talia Pollok PT, DPT, CCS, formerly of University of Virginia Med Center
○ Education Chair, APTA Cardiovascular & Pulmonary Section
○ AACPT member
● James Tompkins PT, DPT, Associate Dean, Mayo Clinic School of Health Sciences
○ Secretary, APTA Academy of Acute Care Physical Therapy
○ AACPT member
● Heidi Engel PT, DPT, University of California San Francisco Medical Center
○ AACPT member
○ Cardiovascular & Pulmonary Section member
● Christiane Perme, PT, CCS, FCCM, Rehab Education Specialist, Houston Methodist Hospital Houston, TX
○ Cardiovascular & Pulmonary Section member, 2021 CSM Linda Crane Lecturer
○ AACPT members
● Stephen Ramsey PT, DPT, CCS, Piedmont Medical Center, Atlanta GA
○ Advocacy Chair, APTA Cardiovascular & Pulmonary Section
○ AACPT member
● Ellen Hillegass PT, EdD, CCS, FAPTA, Piedmont Medical Center & Mercer University, Atlanta GA
○ AACPT member
○ Cardiovascular & Pulmonary Section member
● Angela Campbell PT, DPT, CCS, Professor of Physical Therapy Springfield College
○ President, APTA Cardiovascular & Pulmonary Section
○ AACPT member

Housekeeping
● All microphones are muted upon entrance
● Hosts will record your questions & comments
● Audience questions & comments will be shared after all
speakers present
● Recording will be available on AACPT, HPA & CVP
websites by Monday March 30
● Certificate awarded upon completion of post-webinar
survey
● Thank you to

DISCLAIMER
This webinar is intended to educate clinicians. This is NOT A HOW-TO to train
inexperienced clinicians to start treating COVID-19 in the acute care setting.
The presenters feel strongly that, in general, we should be MINIMIZING our
contact with COVID-19 positive patients, as the more bodies that enter these
rooms the higher the likelihood of that body becoming a vector spreading the
disease between patients, our families, and into the community. The
seemingly simple process of donning/doffing PPE poses the biggest risk of
transmission. REPEATED PPE training, fit testing, and credentialing within your
institution is vital.

COVID-19
Pathophysiology
Clinical Presentation
& Medical Management
Ellen Hillegass, PT, PhD,
CCS, FAPTA
Mercer University
Atlanta, GA

Overview of Pathophysiology and Clinical
Presentation
• Pathophysiology: Brief overview of ARDS versus true pneumonia
• Clinical Presentation
• Patient demographics
• Symptoms
• Lab Values
• CT/CXR
• Multi-organ involvement
• Cardiac Involvement
• Myocarditis:
• lab values,
• ECG
• Severe Vs Non ICU co-vid

Pneumonia

Acute Respiratory Distress Syndrome
From: Cancer therapy
advisor

Symptoms of the Disease
• Common symptoms
• Dry cough
• Fever
• Fatigue
• Shortness of breath
• Uncommon symptoms
• Headache
• Sore throat
• Nasal congestion
• Chills
• Nausea/vomiting/diarrhea
Severe Disease symptoms
High Fever
Coughing up blood
Decreased white blood cells
Kidney dysfunction/ difficulty with
urination
From Seattle Intensivist:

ACR


Lab Values
• Increased C Reactive Protein (CRP)
• Rises day 3-5, peaks day 14
• Decreased Lymphocytes
• Decreases throughout first 14 days…lowest day 14
• Decreased Platelets
• Increased BUN/Cr
• Increased LFTs (AST/ALT/Total Bili)
• In typical ARDS we see increased PCT and Lactate…not finding this
• Increased ESR in over 50% patients
• Lab Value Info from Seattle Intensivist

CT/CXR findings
• CXR may be normal; recommend CT scans if possible
• If abnormal: bilateral peripheral opacities
• CT : Ground glass opacities, crazy paving, consolidation
• RARELY unilateral




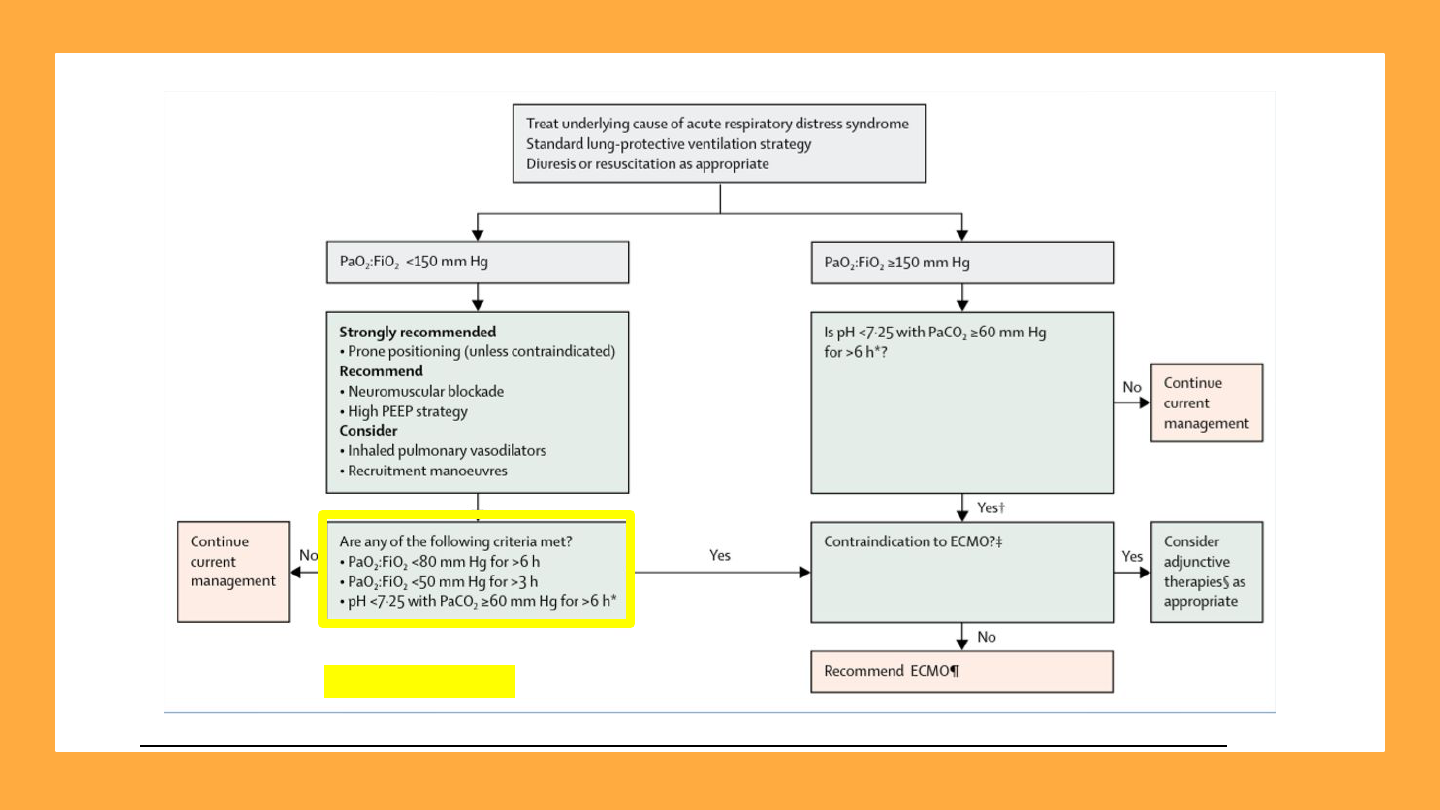
Covid 19: Principal Feature of Severe Presentation
Development of ARDS: Acute Respiratory Distress Syndrome
ARDS: acute onset HYPOXEMIC respiratory failure with bilateral infiltrates
Infiltrates are NOT necessarily secretions but more leakiness from
capillaries.
Guidelines EXIST for management of ARDS as well as Covid19
Conservative fluid strategies without shock
Early antibiotics if suspect bacterial co-infection
Lung protective ventilation (ARDS NET PROTOCOL…Low Tidal Volume
Increased PEEP)
Prone positioning
Consideration of ECMO if cannot improve hypoxemia
Formal guidelines: management of acute respiratory distress syndrome
• Papazian L et al, Formal Guidelines for management of acute respiratory distress syndrome Annals of Intensive Care volume 9, Article number: 69 (2019)
• http://www.ardsnet.org/files/ventilator_protocol_2008-07.pdf
• Griffiths MJD. Guidelines on management of ARDS https://bmjopenrespres.bmj.com/content/6/1/e000420
• Fan et al: https://www.thoracic.org/statements/resources/cc/ards-guidelines.pdf
• http://www.apta.org/PTinMotion/News/2020/03/26/AcuteHospitalCOVIDGuidelines/

Covid: Cardiac Issues
• ACE-2 is the binding site for the CoV- virus and ACE – are found in cardiomyocytes
• Troponin rise common in acute respiratory and also correlated with disease severity
• Abnormal troponin especially if using high sensitivy assay but does not mean MI…may indicate myositis
• Hs-cTni significantly elevated in more than ½ patients who died.
• From ACC: clinicians are advised to only measure troponin if the diagnosis of acute MI is being considered on clinical
grounds and an abnormal troponin should not be considered evidence for an acute MI without corroborating evidence.
• elevation of BNP or NT-proBNP is associated with an unfavorable course among patients with ARDS.
• Use of echocardiography or coronary angiography for COVID-19 patients with myocardial injury or elevated natriuretic
peptide should be restricted to those patients in whom these procedures would be expected to meaningfully affect
outcome.
• No data exist to suggest benefit from anti-platelet or anticoagulant therapy for those with acute myocardial injury with the
exception of those with Type 1 MI.
• The HFSA, ACC, and AHA recommend continuation of RAAS antagonists for those patients who are currently prescribed such
agents for indications for which these agents are known to be beneficial, such as heart failure, hypertension, or ischemic
heart disease.
• Resources:
• JAMA Insights: Care for Critically Ill patients with covid 19 by S Murthy March 11 2020
• www.acc.org

Bottom line on Cardiac Issues from ACC
• If elevations in Troponin, BNP or proBNP look for other
documentation of cardiac injury
• ECG, symptoms, arrhythmias, Echo
• Patients demonstrating heart failure, arrhythmia, ECG changes or
cardiomegaly should have echocardiography
• If have evidence of true acute MI (symptoms, ECG, troponins), or
evidence of myocarditis and also have history of CVD or angina or
high risk for CVD, TREAT like MI..await decreases in troponins and
other enzymes, await hemodynamic stability and then MONITOR
hemodynamics and symptoms with all activities

Other data from ACC on prognosis
• Case fatality rates for comorbid patients are materially higher than
the average population:
• Cancer: 5.6%
• Hypertension: 6.0%
• Chronic respiratory disease: 6.3%
• Diabetes: 7.3%
• Cardiovascular disease: 10.5%

Non Severe CoVID
• FOLLOW DISEASE TRANSMISSION PROTOCOLS AND DO NOT SEE
THESE PATIENTS UNLESS TAKE THESE PROTOCOLS AND PREFERABLY
LAST PATIENTS OF DAY
• Assess Oxygen status…CoVID is a hypoxemic disease
• Assess cardiac stability: look at ECG, Enzymes, Echo
• Assess hemodynamic stability with activity
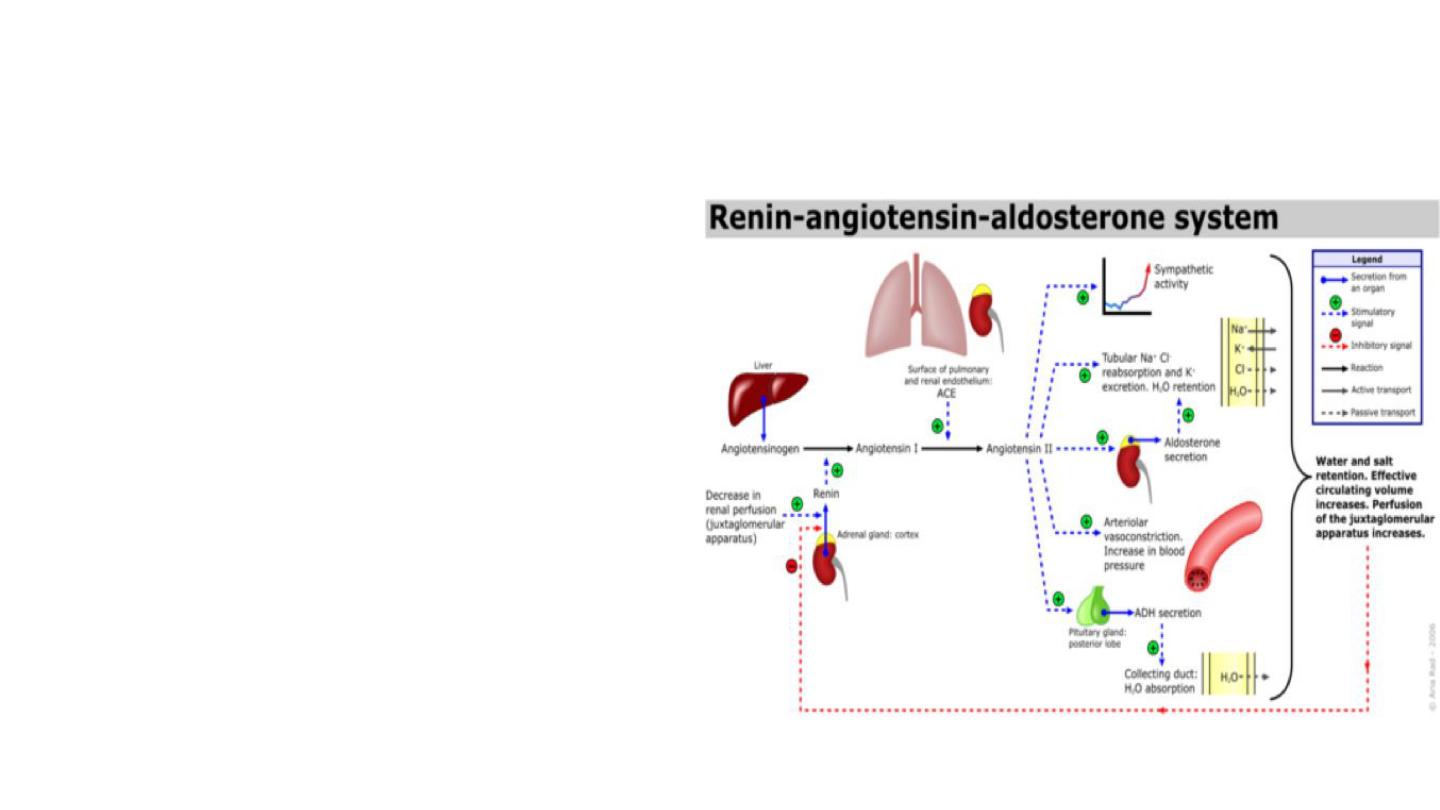
RAAS: Renin-Angiotensin-Aldosterone-System &
Covid-19
● ACEi / ARB & Covid19 risk
factor?
● Non-productive cough
● ACE2 is Covid-19
co-receptor
● ACE2 receptor upregulation
● ACEi/ARB use in elderly
● ACE genotype

ACE2, ACEi, ARB & Covid-19
● ACEi often drug of choice for HTN in elderly
○ Appears to preserve muscle function/ reduce sarcopenia
● ACE2 receptor upregulation:
○ ACEi/ ARB use
○ Diabetes
○ Ibuprofen/ NSAID use
● AHA/ACC advise patients currently to not stop ACE-/ ARB as research
is lacking and clinical anecdotes vary
● Current guidelines recommend acetaminophen for fever reduction in
Covid-19, but do not explicitly caution against NSAID use

ARDS: Acute Respiratory Distress Syndrome
● Leading cause Covid-19 mortality
● Subgroup appear to develop cytokine
storm
○ Labs: ESR & ferritin
○ Corticosteroids might be indicated
● Mechanical ventilation
○ Minimize barotrauma
○ Moderate to high PEEP
● Prone positioning
● ECMO

Prone Positioning
● Optimizes gas exchange/
improves oxygenation
● Prone positioning 16-18h
● Ventilated & non-ventilated
● Prone teams
● Sedation (+ inflammation)
→ CAW/ CIP

Airway Clearance Techniques (ACT) for Covid-19?
● Exudate/ excess mucus less common
● Cough & ACT - Aerosol Generating
Procedures (APGs)
○ ↑ Risk transmission
○ N95 mask advised
● ACT generally not
recommended
○ Unless compelling condition
○ Severe pulm edema (e.g. ARDS) is
relative contraindication*

Physiotherapy management for COVID-19 in the acute
hospital setting: Recommendations to guide clinical
practice
● Multi-national CPG endorsed by APTA, AACPT & APTA
CVP (http://www.apta.org/PTinMotion/News/2020/03/26/AcuteHospitalCOVIDGuidelines/)
● Staffing/workforce, screening, PPE, interventions
● “Respiratory physiotherapist” distinction
Thomas P, Baldwin C, Bissett B, Boden I, Gosselink R, Granger
CL, Hodgson C, Jones AYM, Kho ME, Moses R,
Ntoumenopoulos G, Parry SM, Patman S, van der Lee L
(2020): Physiotherapy management for COVID-19 in the acute
hospital setting. Recommendations to guide clinical practice.
Version 1.0, published 23 March 2020

References
1. Alhanzzi W, Moller MH, et al. Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill
Adults with Coronavirus Disease 2019 (COVID-19).
https://www.sccm.org/Research/Guidelines/Guidelines/Surviving-Sepsis-Campaign-Guidelines-on-the-Ma
nag
2. Diaz JH. Hypothesis: angiotensin-converting enzyme inhibitors and angiotensin receptor blockers may
increase the risk of severe COVID-19. Journal of Travel Medicine, 2020; DOI: 10.1093/jtm/taaa041\
3. Feng L, Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?
Lancet Res Med. DOI:https://doi.org/10.1016/S2213-2600(20)30116-8\
4. JONES, A., H.E. MONTGOMERY, and D.R. WOODS. Human performance: A role for the ACE genotype?
Exerc. Sport Sci. Rev., Vol. 30, No. 4, pp. 184–190, 2002.
5. Leung JM, Yang CX, et al. ACE-2 Expression in the Small Airway Epithelia of Smokers and COPD
Patients: Implications for COVID-19. doi: https://doi.org/10.1101/2020.03.18.20038455
6. Papazian, L., Aubron, C., Brochard, L. et al. Formal guidelines: management of acute respiratory distress
syndrome. Ann. Intensive Care 9, 69 (2019). https://doi.org/10.1186/s13613-019-0540-9
7. Patel AB, Verma A. COVID-19 and Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor
Blockers: What Is the Evidence? JAMA. Published online March 24, 2020.
doi:10.1001/jama.2020.4812ce?
8. Thomas P, Baldwin C, Bissett B, Boden I, Gosselink R, Granger CL, Hodgson C, Jones AYM, Kho ME,
Moses R, Ntoumenopoulos G, Parry SM, Patman S, van der Lee L (2020): Physiotherapy management
for COVID-19 in the acute hospital setting. Recommendations to guide clinical practice. Version 1.0,
published 23 March 2020

COVID-19: Considerations for
Mechanical Ventilation
Christiane Perme, PT, CCS, FCCM
Houston Methodist Hospital
Houston, TX

COVID-19: Oxygenation Strategies
➔ Clinical considerations: Understand the spectrum of disease severity:
◆ Asymptomatic infection: 80%
◆ Mild upper respiratory illness:15%
◆ Severe viral pneumonia with respiratory failure and/or death: 5%
➔ What is the SpO2 target?
◆ Recommendation: SpO2 92-96%
Thomas P et al. (2020): Physiotherapy management for COVID-19 in the acute hospital setting. Recommendations to guide clinical
practice. Version 1.0, published 23 March

COVID-19: Can intubation be avoided by High-flow
nasal cannula (HFNC) and non-invasive positive
pressure ventilation (NIPPV) ?
➔ Recommendation: Avoid HFNC/NIPPV for patients with ARDS!
➔ General consensus at this point suggests HFNC/NIPPV:
o May delay but not avoid invasive ventilation in patients with rapid
progression of disease
o May be used in selected patients in early stages and milder forms of acute
hypoxemic respiratory failure
o May increase the risk of viral transmission

COVID-19: Common ventilator settings for patients with ARDS
➔ Recommendation: Patients should be managed with lung-protective
strategies to minimize ventilator injury (ARDSnet)
➔ Ventilation:
◆ Tidal volume (Vt): 4-6 ml/kg predicted body weight
◆ Plateau pressures (Pplateau) < 30 cmH2O
◆ RR: 16-24 (May increase to 35 as needed if acidosis present)
◆ Mode of ventilation: Volume Control (AC/VC)
➔ Oxygenation:
◆ PEEP: Moderate to high levels as needed
◆ FiO2: 100% on intubation, rapidly wean to SpO2 92-96%

COVID-19: Physical Therapy considerations for patients on
mechanical ventilation
➔ Able to clearly understand:
◆ Severity of illness in ICU
◆ Medical management of the patient
◆ Difference between “ early mobility”, “ early physical therapy”, and ‘early
rehab” in ICU
◆ Importance of a “safety screen” prior to any physical therapy intervention
◆ Absolute and relative contraindications for out of bed activities
◆ Interdisciplinary collaboration

COVID-19: Can we implement simple strategies for early
mobility/exercise in ICU which can be used and sustained for
every patient...every day... in any ICU in the world?
➔ Early Mobility:
◆ Every patient in ICU gets out of bed at least once/daily, EXCEPT the
ones who should not be out of bed!
➔ Early exercises:
◆ 100 leg lifts/day!
◆ 100 arm lifts/day!

COVID-19:Take home messages
➔ Mobility and exercise MUST be a priority in the plan of care for every patient
in ICU!
➔ Early mobility and exercise in ICU is everyone’s job!
➔ Prevention of muscle weakness in ICU is much better than any treatment
currently available!

COVID-19: Resources for clinicians with limited ICU
experience
➔ Hodgson CL et al. Expert consensus and recommendations on safety criteria for
active mobilization of mechanically ventilated critically ill adults. Crit Care. 2014
Dec 4;18(6):658 PMID:25475522.
➔ Perme C, Chandrashekar R. Managing the patient on Mechanical Ventilation in ICU:
Early Mobility and Walking Program. Acute Care Perspectives. Spring 2008, Vol 17,
Number 1, 10-15.
➔ Perme C, Chandrashekar R. Early mobility and walking program for patients in
intensive care units: creating a standard of care. Am J Crit Care. 2009 May;
18(3):212-21. PMID: 19234100.

COVID-19: Resources available
➔ ICU Liberation Bundle (ABCDEF)
https://www.sccm.org/ICULiberation/ABCDEF-Bundles
➔ Devlin JW et al. Clinical Practice Guidelines for the Prevention and Management of
Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult
Patients in the ICU. Crit Care Med. 2018 Sep;46(9):e825-e873.PMID: 30113379.
➔ Thomas P et al. (2020): Physiotherapy management for COVID-19 in the acute hospital
setting. Recommendations to guide clinical practice. Version 1.0, published 23 March
➔ STAT Pearls/NCBI Bookshelf: Ventilator Management -
https://www.ncbi.nlm.nih.gov/books/NBK448186/
➔ Society of Critical Care Medicine: Critical Care For Non- ICU Clinicians -
https://www.sccm.org/covid19

Extracorporeal
Membrane Oxygenation
(ECMO)
for Novel COVID-19
Stephen Ramsey PT, DPT
Board Certified Specialist in Cardiovascular and Pulmonary Physical
Therapy

Outline
● Review of ECMO
● Use of ECMO in recent
Pandemic/Epidemics
● Use of ECMO in ARDS
● Evidence regarding mobilization of patients
on ECMO
● Current/existing evidence for the use of
ECMO for COVID-19
● Considerations for the role of PT for ECMO
patients with COVID-19
● Suggested Strategy for PT involvement for
ECMO patients with COVID-19

What is ECMO?
● ECMO (ECLS) is the use of mechanical devices
to support heart and/or lung function in severe
heart or lung failure, unresponsive to optimal
conventional care.
● Works by draining blood from the body (venous
system) into a pump that directs the blood
through the membrane lung (oxygenator) and
back into the patient.
● In the membrane lung exists a network of
thousands of small hollow fibers made of a
material that allows diffusion of oxygen(O2) and
carbon dioxide (CO2) across a gradient. Oxygen
is diffused into the blood, and CO2 is extracted
out. The blood is returned to a venous circulation,
arterial circulation, or both.
1

Types of
ECMO
1
VenoVenous (VV)
● Drains from vein: Returns
to vein
● Functionally bypasses
lungs
● Still reliant on native
cardiac function for
systemic perfusion
● Peripheral saturation of O2
may be low secondary to
mixing in venous system
with very little oxygenation
occurring in native lungs
○ SpO2 as low as 70’s at
rest.
● Can “rest” lungs
VenoArterial (VA)
● Drains from vein: Returns
to artery
● Functionally bypasses
lungs and heart
● Native CO as flow
through circuit
● Increases systemic
perfusion
● Allows for wean of
inotropes/pressors
● Can “rest” heart/lungs

Use of
ECMO in
Recent
Epidemics
and
Pandemics
● In previous infectious diseases, advanced modalities such as ECMO
were used for many patients with severe acute respiratory distress
syndrome (ARDS).
● Data from H1N1
2
- 2009
○ ECMO utilization 2.6%
○ Avg Age: 34 yo
○ Avg duration of ECMO: 10 days
○ Case Fatality Rate 21%
○ ICU Survival 71%
3
● Data from MERS
4
- 2015
○ ECMO utilization 5.8%
○ Avg duration of ECMO: 8 days

Proliferation of ECMO
Programs
Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases Ramanathan, Kollengode et al. The Lancet Respiratory Medicine, Volume 0, Issue 0

Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases Ramanathan, Kollengode et al. The Lancet Respiratory Medicine, Volume 0, Issue 0
ECMO for
ARDS
● CESAR Trial
5
: 63% disability-free survival at 6 months in 90
patients who were randomized to receive ECMO
● EOLIA Trial
6
: Early ECMO showed no significant difference in
60 day mortality when compared to control group (ventilator,
NMB, prone therapy). Did show:
○ Lower relative risk of treatment failure 0.62 (95% CI, 0.47 to 0.82;
P<0.001)
■ Treatment failure was defined as death by day 60 in patients
in the ECMO group, and as crossover to ECMO or death in
patients in the control group
○ Lower risk of Renal replacement therapy (RRT) at day 60 (50 vs.
32 days; median difference, 18 days; 95% CI, 0 to 51)
○ Underwent less prone position therapy

Mobilization
of Patients
on ECMO
● Growing pool of data regarding safety and feasibility of
mobilization of both VV and VA cases, with various
cannulation techniques.
● Safety/feasibility
○ VV: International Survey of 209 ECMO centers
7
■ 84% of centers mobilize patients. Just over 40% initiated PT
within 72 hours of cannulation.
■ 22% of centers reported routine ambulation
○ VA: Small retrospective cohort studies
8-9
■ Successful ambulation with femorally placed VA ECMO with
no adverse events.
● Outcome Data
○ Decreases in mechanical ventilation days, ICU and total hospital
length of stay in patients participating in PT while awaiting lung
transplantation.
10
○ Possible association between mobilization and decreased overall
hospital mortality.
11

COVID-19
● The pathological features of COVID-19 greatly resemble
those seen in SARS and Middle Eastern respiratory
syndrome (MERS) coronavirus infection.
12
● Disease that leads to increase in capillary vascular
permeability. Protein rich edema escapes from plasma into
interstitial space and subsequent alveolar (epithelium and
endothelium) injury.
○ 15-30% of cases develop ARDS
■ 4-15% mortality amongst ARDS group

● Disclaimer: This is a highly dynamic situation. No one truly knows if ECMO is the
right answer!
● WHO: Interim guidelines
for the management of suspected COVID-19
recommend administering venovenous (VV) ECMO to eligible patients with
COVID-19-related acute respiratory distress syndrome (ARDS) in expert centers
with sufficient case volumes to ensure clinical expertise.
13
Recommendations for ECMO in COVID-19

● Use pre-existing Criteria for candidacy
○ Use of EOLIA?
● What about the patients who develop cardiac dysfunction?
○ VA or VAV ECMO may be indicated
Recommendations for ECMO in COVID-19

Recommendations for ECMO in COVID-19
● In inexperienced Centers: ECMO is not a therapy to be rushed to the front lines
when all resources are stretched during a pandemic.
● Summary: ECMO may have a role in the management of some patients with
COVID-19 who have refractory hypoxemic respiratory failure. However, much
about the virus is unknown, including the natural history, incidence of late
complications, viral persistence, or the prognoses indifferent subsets of
patients.
14

■ 3/9/20
■ N 181 (28% total mortality)
● 31% developed ARDS (93% mortality)
○ Avg onset 12 days
● 23% HF (64% mortality)
● 20% septic Shock (100% mortality)
○ Avg onset 9 days
● 3 on ECMO
○ No survivors
• 3/13/20
• N 201 (21% total mortality)
• 41.8% developed ARDS (52.4% mortality)
• 1 total on ECMO
• 2/11/20
• N 278 (8.5% mortality)
• 20% developed ARDS
• 9 total on ECMO (3.2%)
Available Data for ECMO in Japan/Korea
● Seeing a slightly younger population. More ECMO utilization than China.
● >50 COVID19 cases reported on ECMO, with survivors, with many still receiving
treatment.
○ Japan: 20 patients as of 3/10.
○ Limited capacity, only 300 circuits in all of Japan!
○ Using judiciously
● Awaiting full data reports any day and anticipate this will guide recommendations
for ECMO going forward
Adapted from Webinar: “Preparing to Support Patients COVID-19 patients on ECMO”

Available Data for ECMO in US
● ELSO Registry data: 40 patients on ECMO with confirmed COVID-19
○ This is only registered centers who are reporting currently
○ Likely much more
● “If these epicenters of infection occur in sophisticated health care systems with
preexisting ECMO programs, this will provide vital information about the utility of
ECMO and help anticipate global demand. “
● “Should the initial experience be encouraging, it is likely that non-ECMO centers
will refer early to ECMO centers in anticipation of impending clinical deterioration.
This will disproportionately affect hospitals with ECMO programs, even when
ECMO is not required.
14

Considerations for
Mobilization in COVID-19
● Resource management
○ PPE
■ Could be a daily assessment based on your facility’s supply
● Heavy staff burden
○ Often requires RN, Perfusion, +/- RT
○ Do I feel comfortable possibly going in with skeleton crew?
● Pathophysiology of disease
○ Will mobility help?- Probably
○ Are ACT/AGP indicated?- Maybe not
● What can we delegate in our attempt to conserve resources?
○ Do we always have to be in room touching patient?
○ What about standing at door and directing care?

Patient Hemodynamically
stable for PT?
Yes
Have RN conduct screen
of mobility/strength
with PT supervision
Mobility deficits exist:
PT to engage in
mobility training
No significant mobility
deficits: PT continue to
be resource and
oversee RN mobilizing
patient
PT conduct initial
evaluation
Mobility deficits: Set
conservative POC
(3x/wk?)
Some deficits: POC
1-2x/wk. RN to mobilize
in between PT sessions
No significant mobility
deficits: Oversee RN
management for
mobilization of ECMO
patient
No
Follow in IDRs

Patient Hemodynamically
stable for PT?
Yes
Have RN conduct screen
of mobility/strength
with PT supervision
Mobility deficits exist:
PT to engage in
mobility training
No significant mobility
deficits: PT continue to
be resource and
oversee RN mobilizing
patient
PT conduct initial
evaluation
Mobility deficits: Set
conservative POC
(3x/wk?)
Some deficits: POC
1-2x/wk. RN to mobilize
in between PT sessions
No significant mobility
deficits: Oversee RN
management for
mobilization of ECMO
patient
No
Follow in IDRs

References
1. Brogan, T. V., Lequier, L., Lorusso, R., MacLaren, G., & Peek, G. (2017). Extracorporeal Life Support: The ELSO Red Book. (1 ed.) Extracorporeal Life Support Organization
2. The Australia and New Zealand Extracorporeal Membrane Oxygenation (ANZ ECMO) Influenza Investigators*. Extracorporeal Membrane Oxygenation for 2009 Influenza A(H1N1) Acute Respiratory Distress Syndrome. JAMA.
2009;302(17):1888–1895. doi:10.1001/jama.2009.1535
3. Davies A, Jones D, Bailey M, et al. Extracorporeal Membrane Oxygenation for 2009 Influenza A(H1N1) Acute Respiratory Distress Syndrome. JAMA. 2009;302(17):1888-1895.
4. Arabi YM,Al-Omari A Mandourah Y et al. Critically ill patients with the Middle East respiratory syndrome: a multicenter retrospective cohort study.Crit Care Med. 2017; 45: 1683-1695
5. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial Peek, Giles J et al. The Lancet,
Volume 374, Issue 9698, 1351 - 1363
6. Combes A, Hajage D, Capellier G, Demoule A, Lavoué S, Guervilly C, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378:1965–75.
7. Viau-Lapointe J, DeBacker J, Marhong JD, et al. Sedation and Mobilization During Venovenous Extracorporeal Membrane Oxygenation for Acute Respiratory Failure: An International Survey. In: B24. CRITICAL CARE: ACUTE
RESPIRATORY FAILURE - MECHANICAL VENTILATION AND BEYOND. American Thoracic Society; 2017:A3029-A3029.
8. Pasrija C, Mackowick KM, Raithel M, et al. Ambulation With Femoral Arterial Cannulation Can Be Safely Performed on Venoarterial Extracorporeal Membrane Oxygenation. The Annals of Thoracic Surgery. 2019;107(5):1389-1394.
9. Wells CL, Forreseter J, Vogel J, Rector R, Herr D. The Feasibility and Safety in Providing Early Rehabilitaion and Ambulation for Adults on Percutaneous Venous to Arterial Extracorporeal Membrane Oxygenation Support. In: A102.
TRANSPLANTATION: ADVANCES AND CHALLENGES. American Thoracic Society; 2017:A2710-A2710.
10. Rehder KJ, Turner DA, Hartwig MG, et al. Active Rehabilitation During Extracorporeal Membrane Oxygenation as a Bridge to Lung Transplantation. Respiratory Care. 2013;58(8):1291.
11. Munshi L, Kobayashi T, DeBacker J, et al. Intensive Care Physiotherapy during Extracorporeal Membrane Oxygenation for Acute Respiratory Distress Syndrome. Annals of the American Thoracic Society. 2016;14(2):246-253.
12. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Xu, Zhe et al. The Lancet Respiratory Medicine, Volume 0, Issue 0
13. Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases Ramanathan, Kollengode et al. The Lancet Respiratory Medicine, Volume 0, Issue 0
14. MacLaren G, Fisher D, Brodie D. Preparing for the Most Critically Ill Patients With COVID-19: The Potential Role of Extracorporeal Membrane Oxygenation. JAMA. Published online February 19, 2020. doi:10.1001/jama.2020.2342

Goals for Physical Therapy in
Acute Care with COVID-19
●Don’t be a vector of COVID
●Prioritize your list of patients- the COVID negative minimum
assist or moderate assist elderly, comorbidity or
immunocompromised patients need to get home ASAP
●Understand the complex needs of hospitalized COVID +
patients, be holistic, creative, comprehensive

COVID Overview UCSF School of Medicine
You Tube Channel
Jennifer Babik, MD, PhD

COVID Overview UCSF School of Medicine You Tube
Channel
Jennifer Babik, MD, PhD

COVID Overview UCSF School of Medicine You Tube
Channel
Jennifer Babik, MD, PhD

COVID Overview UCSF School of Medicine YouTube
Channel
Jennifer Babik, MD, PhD


A Work In Progress
●Learning as we go
●Testing problems-
○5,000 tests/million Korea
○100 test/million USA
○25% false negative for swab tests
●Supply chain problems
○Don/doff infectious problem
●WHO has 392 registered treatment trials
○Including multi-center studies for close contact prophylaxis

Goals for Physical Therapy in Acute Care
with COVID-19
●Don’t be a vector of COVID , geographic contained and flex scheduled
assignments
●Prioritize your list of patients- the COVID negative minimum assist or moderate
assist elderly, comorbidity or immunocompromised patients need to get home
ASAP
●Understand the complex needs of hospitalized COVID + patients, be holistic,
creative, comprehensive

When looking at each individual patient, the needs and capabilities
of the patient can be assessed as follows:
Admitting
Event
(not the same as
diagnosis)
Disease and Chronic Medical
Burden, Co-morbid conditions
Physiologic Reserve, Functional Baseline,
Psychosocial Suppport, Physical
Performance History, Age

Acute Patient Needs 1 to 2 weeks
●Isolation Psychosis
●Delirium
●Communication issues
●Dyspnea/Work of breathing
●Fatigue
●Pain
●Disempowered identity
●Fear
●Prevention of eminent muscle wasting

Acute/Chronic Needs~ d 14+
●As inflammatory process increases (and this may be rapid sudden surprising
overwhelming onset)
○Muscle wasting, muscle catabolism, ICU Acquired Weakness (ICUAW)
○Low endurance
○Fatigue
○Pain
○Depression

After Returning Home
● Restoring the life they knew, reconciling new body with identity, movement
as empowerment and understanding
● Moving past the trauma of the hospital stay
Look to the evidence produced for geriatric, oncology, and endurance
athletic populations
Basic physiologic principles still apply
Educate patient and family for long term reconditioning, strength training
Inpatient and Outpatient collaborations, creative home based solutions

PICS: SCCM THRIVE- myicucare.org
Post-intensive
care syndrome
Patient
Physical:
ICUAW, osteoporosis
ADLs, work
Pain, Ongoing need for
Healthcare
Cognitive:
Executive Functions
Memory
Attention
Visiospatial
Patient and
Family
Psychological
Financial:
Role identity
Work
Anxiety
Depression
Resources available
● Academy of Acute Care Physical Therapy. COVID-19 Resources, Link to
March 21, 2020 webinar with APTA Health Policy & Administration Section.
https://www.acutept.org/page/COVID19
● American College of Cardiology. ACC CLINICAL BULLETIN COVID-19
Clinical Guidance For the CV Care Team.
https://www.acc.org/~/media/665AFA1E710B4B3293138D14BE8D1213.pdf
Published 6 March 2020. Accessed 23 March 2020.
● One Pager ICU https://www.onepagericu.com/covid-resources
● Clinical management of severe acute respiratory infection (SARI) when
COVID-19 disease is suspected.
https://apps.who.int/iris/bitstream/handle/10665/331446/WHO-2019-nCoV-clin
ical-2020.4-eng.pdf Published 13 March 2020. Accessed 25 March 2020.