

Care Plan Review
DSHS RW Part B Case Management
Reven Patlan Jr, MSSW - Training Specialist, DSHS HIV Care Services Group

• Review care plan requirements for Medical and Non-
Medical Case Management per DSHS service standards
• Review the TCT Care Plan screen and process of
creating a care plan
• Review FAQs for Case Management (+TCT Demo)
Learning Objectives

• Medical Case Management
(including Treatment
Adherence Services) |
Texas DSHS
• Non-Medical Case
Management | Texas DSHS
Requirements:
• Initial comprehensive
assessment
• Acuity Screening (required
for MCM only)
• Viral Suppression/Education
(MCM)
• Care Plan
• (Treatment adherence and
Viral Suppression for MCM)
• Referral and follow-up
• Case Closure
Case Management Standards

Care Plans

Care Plan Review
A care plan is required for clients receiving services
through Ryan White Part-B funded Medical and Non-
Medical Case Management. A Care Plan is a mutually
developed living document that assist both clients and
case managers with tracking progress towards goals (with
viral suppression being a primary goal of medical case
management).
A care plan should be updated with outcomes of
interventions and revised or amended in response to
changes in the client’s life circumstances or goals.
Regular “case notes” or “progress notes” should describe
the progress toward meeting care plan goals by
documenting progress in approved electronic health
records OR by utilizing the “Case Notes” screen in Take
Charge Texas.

Care Plan - Contents
• Problem Statement (need)
• Goals (Case managers should focus on no more than three
goals at a time in order to not overwhelm clients with tasks)
• Intervention
Tasks
Referrals
Service deliveries
• Individuals responsible for activity
• Anticipated time for each task

Care Plan Review
• The care plan is updated with
outcomes and revised or
amended in response to changes
in client life circumstances or
goals, at a minimum, every six (6)
months.
• Again, tasks, referrals, and
services should be updated as
they are identified or completed –
not only at set intervals.

Care Plan: Where Is It?
• The care plan should reside in the primary client record of
choice at your agency.
*The most important factor here is CONSITSENCY. Client care plans should be
filed (and updated) in the same place for everyone and should be easily
accessible.*

Care Plan Performance Measures
Percentage of clients with a care plan that contains all of the following:
a. Problem statement or need
b. Goal(s)
c. Intervention (tasks, referral, service delivery)
d. Responsible party for the activity
e. Timeframe for completion
Percentage of clients with care plans that have been updated at least every
6 months.
Percentage of client records with case notes that document the progress
towards meeting goal(s) identified in the care plan.

Creating a Care Plan

Once logged in, select a client and navigate to the Care
Plan screen under the “Case” column on the left
navigation panel:
Updates to TCT Care Plan Screen

Create a mutual goal with the client that addresses a need or barrier
that is specific, measurable, achievable, relevant, and time-bound
(SMART goals). Enter that goal into the care plan goal name and click
“Add Care Plan Goal” (You can edit this later under the “Care Plan
Actions” column)
For this example, we will create a goal to address medication
adherence challenges the client and case manager have identified.
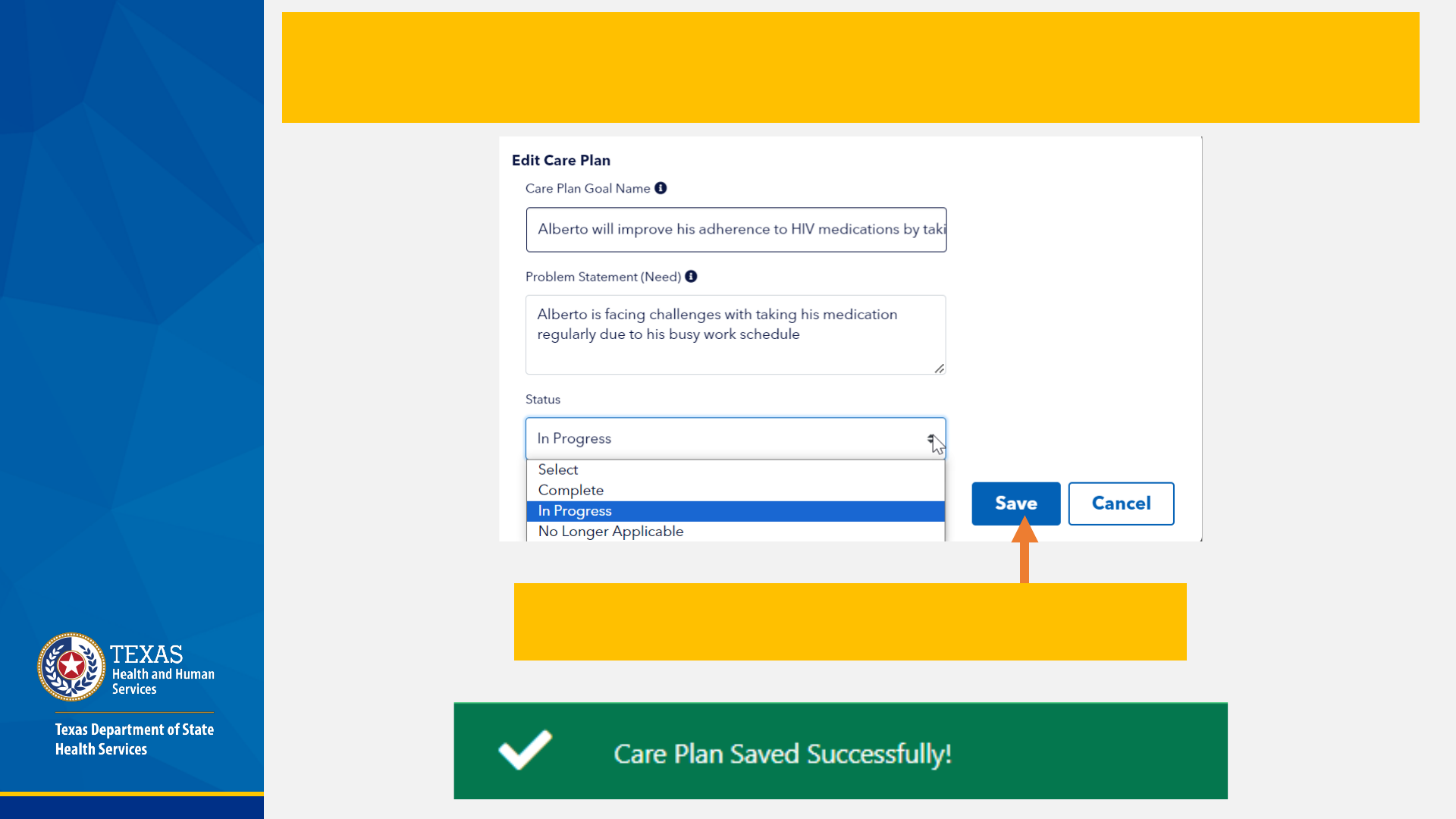
Clicking on the “Add Care Plan Goal” button will present this pop up where you can edit the Care
Plan Goal Name and add the Problem Statement (need). Once you have added the Goal and
Problem statement, you can use this screen to update the status of this goal, as shown below.
Click “Save” once completed and you will see a
confirmation banner at the top of the Care Plan Screen

Once your changes are saved, you will see the Goal and Problem Statement as shown below.
Adding additional goals will be displayed as in the below example
Click on “Plan Intervention Details” to add interventions and tasks to address the stated goals
and needs.
Note: Adding a fourth goal while there are three goals “In Progress” will result in the error
message below

Clicking on “Plan Intervention Details” will display the below pop-up. Click on “Add
Intervention” to list out tasks or activities to be completed to achieve the goal.
Begin filling out the fields to both identify the intervention and reflect
the status and outcome
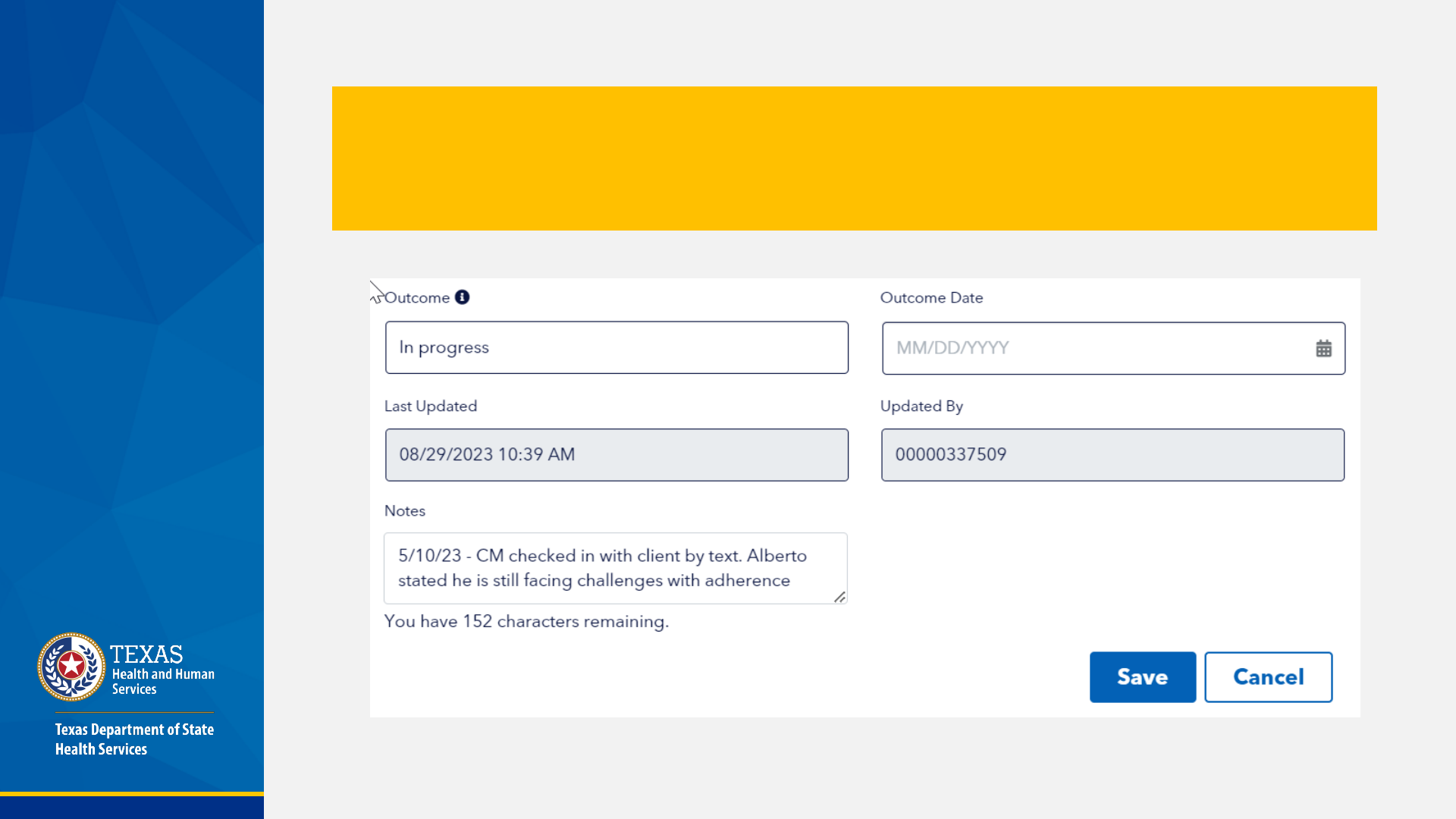
Once there has been an outcome or check-in, you can document this in the “Outcome”
fields below. Add any additional information in the “Notes” section that could be helpful
with tracking. A “last updated” filed will display the last time the record was edited by a
TCT user. Click “Save” to update the intervention/task.

Your intervention will now be shown under the related goal on the Intervention Screen as
shown below. Collaborate with the client to identify additional interventions that will help
achieve the identified goal. Click on “Add Intervention” to add additional tasks and
interventions. You can edit each intervention by clicking “Edit Intervention” in the
“Intervention Actions” column. Click “Save Changes” to ensure your work is saved in TCT.
Note: “Interventions”
are actions taken to
address a need or
barrier the client is
facing related to
their health and
wellbeing. This may
look like a referral, a
check-in, a reminder,
etc. Evidence based
“interventions”
should be used when
appropriate but are
not exclusively the
interventions listed in
a care plan.

Export to a File (PDF, Excel, Word)

FAQ – Case Management
No.
Care plans should ideally be reviewed and updated as
progress towards goals and interventions are met. At
minimum care plans should be updated every six months.
Note for MCM: Acuity screening is required for clients in
Medical Case Management, and frequency of contact and
updates to care plans should match the client's acuity
score and need.
Are care plans only updated and
reviewed every 6 months?

No.
The Care Plan is a living document to help keep track of progress
towards specific goals and needs that impact the client’s care and
well-being. Care plans should be updated as progress towards goals
and interventions are met.
Progress notes document the ongoing work you are doing with your
clients and contain much more information. Case/progress notes
supplement the care plan, and a progress note should be completed
for each meeting with you client (depending on your agency
procedures).
It is encouraged to reduce duplication of case managers
documentation when possible. A care plan note indicating a need for
follow up may state: “see case note for additional details” vs.
documenting the details in both the care plan and case notes. Case
notes and Care Plans should be kept in the Primary Client Record.
Are case/progress notes and the care
plan the same thing?

No.
The care plan should exist in the Primary Client Record. If
your agency uses an approved care plan document or
electronic record, then you do not need to use TCT for your
care plan. However, all clients in case management MUST
have a care plan. Ensure that any care plan documents or
electronic records capture the required information as
indicated by the DSHS Standards of Care.
TCT can be used by agencies that do not have electronic
health systems and would like to have a centralized system
of documentation. The same is true for case/progress notes.
I already complete a care plan using my agency
EHR. Do I still have to input the care plan into TCT?

No.
Medical Case Management is a service based on need and is
not appropriate or necessary for every client accessing services.
Medical Case Management is designed to only serve
individuals who have complex needs related to their ability to
access and maintain HIV medical care.
Medical Case Management should NOT be used as the only
access point for medical care and other agency services.
When clients can maintain their medical care, clients should be
graduated. Clients with ongoing existing need for Treatment
Adherence support due to mental illness or other documented
behavioral disorders meet the criteria for Medical Case
Management services.
Do clients have to be case managed
to receive HIV medical care?

Technically yes, however:
Referrals for health care and support services provided during a
case management visit (medical and non-medical) should be
reported in the appropriate case management service category
(i.e., Medical Case Management or Non-Medical Case
Management)
Referrals are a natural part of case management; the Referral
for Healthcare service category should not be used for referrals
that occur through case management services.
Funds cannot be used to duplicate referral services provided
through other service categories. “Double dipping” or billing
twice for the same service must be avoided!
Can a client receive referrals through
both RFHC and MCM/NMCM?

Q&A
Any additional questions?

Thank you!
Care Plan Review
Reven Patlan, MSSW
Training Specialist, HIV Care Services Group
Ruben.Patlan@dshs.Texas.gov

