Bariatric Surgery
Last Review Date: July 14, 2023
Number: MG.MM.SU.18sv2
Medical Guideline Disclaimer
Property of EmblemHealth. All rights reserved. The treating physician or primary care provider must submit to EmblemHealth the clinical evidence
that the patient meets the criteria for the treatment or surgical procedure. Without this documentation and information, EmblemHealth will not
be able to properly review the request for prior authorization. The clinical review criteria expressed below reflects how EmblemHealth determines
whether certain services or supplies are medically necessary. EmblemHealth established the clinical review criteria based upon a review of
currently available clinical information (including clinical outcome studies in the peer reviewed published medical literature, regulatory status of
the technology, evidence-based guidelines of public health and health research agencies, evidence-based guidelines and positions of leading
national health professional organizations, views of physicians practicing in relevant clinical areas, and other relevant factors). EmblemHealth
expressly reserves the right to revise these conclusions as clinical information changes and welcomes further relevant information. Each benefit
program defines which services are covered. The conclusion that a particular service or supply is medically necessary does not constitute a
representation or warranty that this service or supply is covered and/or paid for by EmblemHealth, as some programs exclude coverage for
services or supplies that EmblemHealth considers medically necessary. If there is a discrepancy between this guideline and a member's benefits
program, the benefits program will govern. In addition, coverage may be mandated by applicable legal requirements of a state, the Federal
Government or the Centers for Medicare & Medicaid Services (CMS) for Medicare and Medicaid members. All coding and web site links are
accurate at time of publication. EmblemHealth Services Company LLC, (“EmblemHealth”) has adopted the herein policy in providing management,
administrative and other services to EmblemHealth Plan, Inc., EmblemHealth Insurance Company, EmblemHealth Services Company, LLC and
Health Insurance Plan of Greater New York (HIP) related to health benefit plans offered by these entities. All of the aforementioned entities are
affiliated companies under common control of EmblemHealth Inc.
Definitions
1. Bariatric surgical procedure types — restrictive, malabsorptive and combined, all of which may
be performed using either the laparoscopic or open approach.
a. Restrictive — the basic philosophy of restrictive procedures is to create a small gastric
reservoir that forces the patient to eat less at any one time. This objective is achieved by
reducing the size of the stomach pouch to 30 mL or less and leaving only a small channel
to the remaining stomach.
b. Malabsorptive — the goal of purely malabsorptive procedures is to bypass a major
portion of the absorptive surface of the small intestine for the achievement of rapid,
sustained weight loss without a necessary change in eating habits. Purely malabsorptive
procedures (without a restrictive component) are not recommended because of the
potential for complications, including liver failure and electrolyte depletion.
c. Combined restrictive and malabsorptive (hybrid techniques) — the basic philosophy of
combined restrictive and malabsorptive procedures is to balance the benefits and risks
of the two approaches.
2. Body Mass Index (BMI) — a quantitative method of defining obesity in a ratio of weight to
height (kg/m²).

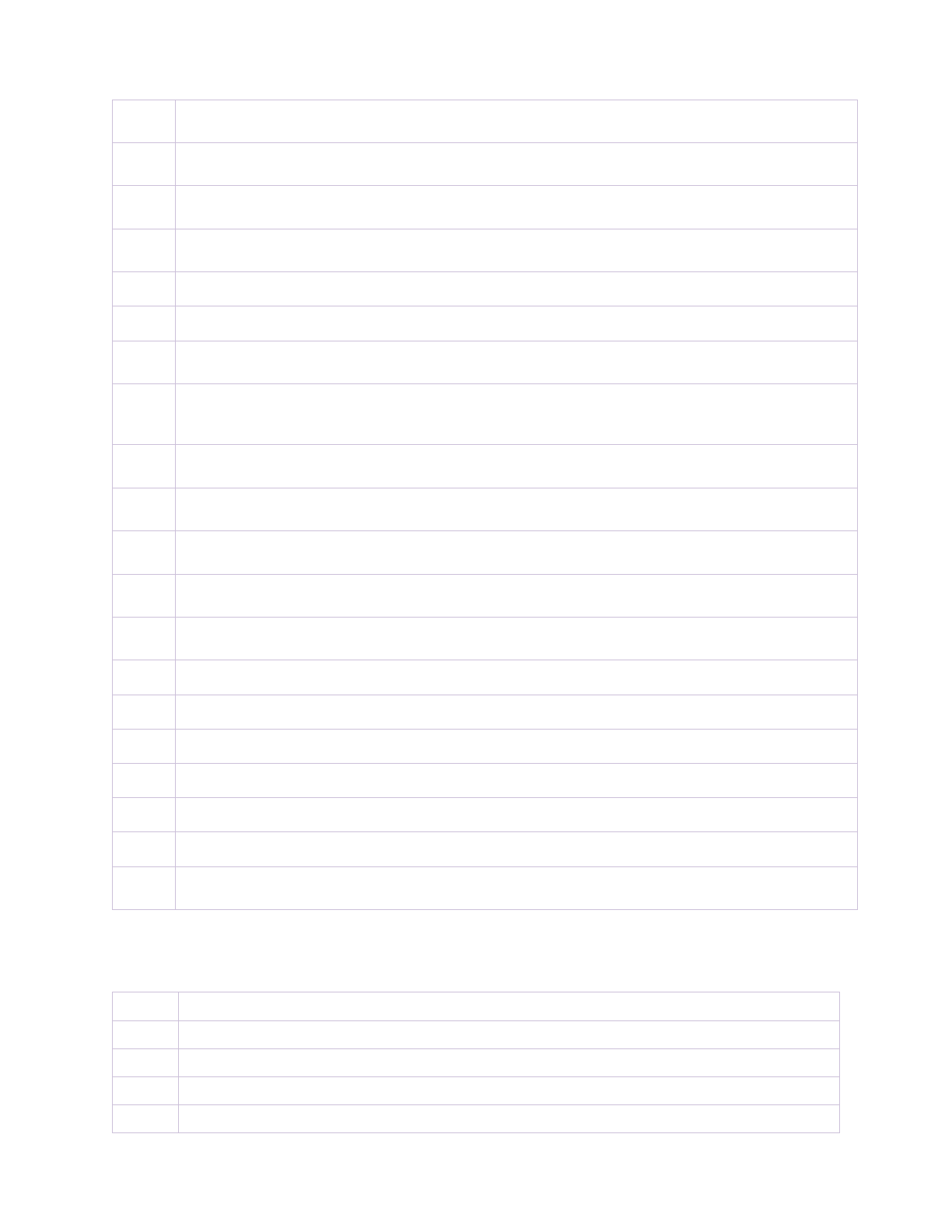
3. Classification
Adults (≥ 18 years of age)
BMI
Overweight
25–29.9 kg/m²
Obese (class I)
30–34.9 kg/m²
Severe obesity (class II)
35–39.9 kg/m²
Clinically severe (also referred to as
extreme or morbid) obesity (class III)
40–49.9 kg/m²
Super obesity
50–59.9 kg/m²
Super-super obesity
60+ kg/m²
Children/adolescents (< 18 years of age) BMI
Class II obesity
≥120% to <140% of the 95th percentile or a BMI ≥ 35
kg/m2 to <39 kg/m2, whichever is lower based on age and
sex
Class III obesity
≥140% of the 95th percentile or BMI ≥ 40kg/m2,
whichever is lower based on age and sex
4. Biliopancreatic Diversion with duodenal switch (BPD/DS) — a combined malabsorptive /
restrictive procedure whereby a suprapapillary Roux-en-Y duodeno-jejunostomy is performed in
combination with a 70%–80% greater curvature gastrectomy (sleeve resection of the stomach;
continuity of the gastric lesser curve is maintained while simultaneously reducing stomach
volume). A long-limb Roux-en-Y is then created. The efferent limb acts to decrease overall
caloric absorption and the long biliopancreatic limb, diverting bile from the alimentary contents,
is intended specifically to induce fat malabsorption.
5. Laparoscopic adjustable gastric banding (LAGB) — a gastric-restrictive implant device used as
an alternative to a gastric-restrictive surgery procedure to treat morbid obesity. The system
consists of a band of silicone elastomer with an inflatable inner shell and a buckle closure
connected by tubing to an access port placed outside the abdominal cavity. The inner diameter
of the band can be readily adjusted by the addition or removal of saline through the access port.
The band is placed laparoscopically around the upper stomach, 1 cm below the esophagogastric
junction. (Must be FDA-approved for Plan consideration) (Not covered for members < 18 years
of age)
6. Roux-en-Y gastric bypass (RYGB) — a large portion (approximately 90%) of the stomach is
excluded. A gastric pouch is created and anastomosed to the proximal jejunum, causing weight
reduction due to a reduction of food intake and mild malabsorption.
7. Single-anastomosis duodenoileal bypass with sleeve gastrectomy (SADI-S) — a simplification of
the duodenal switch (DS) in which the alimentary limb is eliminated, and the common channel is
lengthened. The sleeve is created first, and the duodenum is divided about 4 cm from the
pylorus. A single anastomosis is then created between the side of the first or second part of the
duodenum and the distal jejunum/proximal ileum, creating an afferent limb of biliopancreatic
fluid and an efferent limb that acts like a common channel.
8. Sleeve gastrectomy — a new procedure that is becoming increasingly popular. In this operation,
a tubular stomach is created along the lesser curvature by excising the greater curvature.
Approximately an 80–90% gastrectomy is performed. This is a restrictive procedure and
absorption remains normal.

9. Vertical gastric banding (VGB) / vertical-banded gastroplasty (VBG) (vertical gastric stapling or
partitioning) — A vertical row of staples and a horizontally placed reinforcing band are
positioned across the stomach, creating a proximal pouch and narrowed food outlet. Patients
become full post ingestion of only small food amounts.
10. The Obesity Surgery Mortality Risk Score (OS-MRS) — a risk stratification tool that physicians
should utilize when determining candidacy of the BMI ≥ 50 kg/m2 member. The OS-MRS assigns
1 point to each of 5 preoperative variables: Age, hypertension, male gender, known risk factors
for pulmonary embolism (i.e., previous thromboembolism, preoperative vena cava filter,
hypoventilation, pulmonary hypertension) and BMI.
Obesity Surgery Mortality Risk Score
Risk factor
Points
Age > 45 years
1
Hypertension
1
Male sex
1
Risk factors for pulmonary embolism
1
Body mass index ≥ 50 kg per m
2
1
Total:_____
Risk group (score)
Postoperative mortality risk (deaths/total
number of patients who underwent bariatric
surgery)
Low (0 or 1 points)
5/2164 (0.2%)
Moderate (2 or 3 points)
25/2142 (1.2%)
High (4 or 5 points)
3/125 (2.4%)
Guideline
Bariatric surgery is considered medically necessary when criteria A or B is met.
A. < 18 years of age utilizing any of the above procedures (except adjustable gastric banding) when
either of the following criteria are met:
1. Class II obesity, BMI ≥ 35 kg/m2 or 120% of the 95th percentile for age and sex, whichever is
lower
- Clinically significant disease, examples include but are not limited to type 2 diabetes
mellitus (T2DM), Idiopathic intracranial hypertension (IIH), and nonalcoholic
steatohepatitis (NASH), Blount disease, (slipped capital femoral epiphysis (SCFE),
Gastroesophageal reflux disease (GERD), obstructive sleep apnea (OSA) (apnea-
hypopnea index [AHI] >5), cardiovascular disease risks (hypertension [HTN],
hyperlipidemia, insulin resistance), depressed health-related quality of life
2. Class III obesity, BMI ≥ 40 kg/m2 or 140% of the 95th percentile for age and sex, whichever is
lower (comorbidities not required, but commonly present)
B. ≥ 18 years of age utilizing any of the above procedures (in conjunction with cholecystectomy if such is
requested) when all of the following criteria are met:

1. Full growth achieved.
2. Absence of specific obesity etiology (i.e., endocrine disorders, e.g., adrenal or thyroid conditions,
or treatment of metabolic cause provided, as applicable [does not pertain to diabetes]).
3. Psychological clearance by a mental health professional.
If the member has received any behavioral health issue intervention (i.e., counseling or drug
therapy) within the past 12 months, then the mental health provider should indicate that the
issue of surgery has been discussed with the member and that there are no identified
contraindications to the proposed surgery.
In addition, the member should have no history of substance abuse, or if there is a positive
history, the documentation should indicate that the member has been substance abuse free for
> 1 year or that he/she is in a controlled treatment program and is stabilized.
Other contraindications include active eating disorders, active substance abuse and untreated
psychiatric illness such as suicidal ideation, borderline personality disorder, schizophrenia,
terminal illness and uncontrolled depression.
AND
4. BMI ≥ 40 kg/m² or BMI 35–39.9 kg/m² with ≥ 1 significant comorbidity.
Accompanying documentation of the following associated comorbid conditions and associated
problems must be submitted; any of the following are applicable:
a. Daily functional interference to the extent that performance is extensively curtailed.
1
b. Documented circulatory insufficiency.
c. Documented physical trauma secondary to obesity complications, which causes the
member to be incapacitated.
d. Documented respiratory insufficiency.
e. Documented primary disease complication, as applicable:
i. Coronary heart disease and other atherosclerotic diseases.
ii. Hypertension.
iii. Osteoarthritis.
iv. Obstructive sleep apnea.
v. Type 2 diabetes.
Gastric Band Adjustments
Appropriate as follows:
1. Reduction of band volume: Complaints of difficulty swallowing, persistent reflux or heartburn,
nighttime coughing or regurgitation.
Reduction of band volume may also be appropriate in the setting of maladaptive eating habits
such as eating only soft, carbohydrate and fat laden food due to inability to tolerate any solid
foods. These complaints, however, should be taken in context with member’s compliance with
dietary follow up and recommendations.
2. Increase in band volume: Increased hunger, increased portion sizes.
1
The member must be unable to participate in employment and/or normal activities as a result of the clinically severe
obese condition, which could be resolved by weight reduction (e.g., treatable joint disease).

Adjustments would be expected at approximately 6-week intervals until appropriate fill volume has been
achieved (member is experiencing early and prolonged satiety with small meal sizes, satisfactory weight
loss).
Adjustments should be performed in the outpatient setting and without fluoroscopic guidance unless the
port is not palpable, there is difficulty accessing the port, or leakage is suspected.
Surgical Revision
Members are eligible for coverage of a surgical revision of a previous gastric restrictive surgery if it is
medically necessary as a result of a complication of the original procedure; i.e.:
1. Staple disruption.
2. Obstruction or chronic stricture.
3. Severe esophagitis.
4. Dilatation of the gastric pouch in a member who experienced appropriate weight loss prior to
the dilatation.
Note: Laparoscopic adjustable banding revisional surgery will be covered for band slippage or erosion,
both of which are deemed urgent medical conditions.
Surgical Repetition
Members are eligible for coverage of repeat bariatric surgery if both of the following criteria are met:
1. Insufficient weight loss (success defined as a weight loss of > 50% of excess body weight)
2. The medically necessary criteria (as outlined above) are met.
Note: Member compliance with prescribed post-procedure nutrition and exercise program is prerequisite
to consideration.
Postsurgical Panniculectomy Requests
(See Cosmetic and Reconstructive Surgery Procedures and/or Abdominoplasty/Panniculectomy)
Limitations/Exclusions
1. Surgical revision is not considered medically necessary for members who have a functional
operation (without any evidence of medical abnormality) because of inadequate weight loss.
2. Cholecystectomies performed incidental to bariatric surgery will only be covered if the bariatric
surgery has been authorized/approved.
3. Repair of an asymptomatic or incidentally identified hiatal hernia (CPT codes 43280, 43281,
43282, 43289, 43499 or 43659) will be denied as incidental/inclusive procedures when reported
with bariatric surgery code ranges 43770–43775 and 43842–43848, 43644, 43645, 43886, 43887
or 43888). Modifier 59 will not override these codes as hiatal hernia repair is considered an
integral part of obesity surgery.
4. Case-by-case consideration for preoperative esophagogastroduodenoscopy (EGD) (CPT 43235)
will be given for members symptomatic of gastroesophageal reflux disease (GERD) (e.g.,
heartburn, regurgitation, dysphagia, etc.).
5. Transoral outlet reduction (TORe) (e.g., the Overstitch device, CPT 43659) — a minimally
invasive endoscopic revision procedure performed in patients with weight regain or inadequate

weight loss following Roux-en-Y gastric bypass — is considered investigational due to insufficient
evidence of therapeutic value.
6. Adjustable gastric banding is considered investigational for members <18 years of age
7. All other gastric bypass/restrictive procedures (and other treatment modalities not listed above
as medically necessary) are considered investigational due to insufficient evidence of
therapeutic value. These include, but are not limited to, minimally invasive endoluminal gastric
restrictive surgical techniques (e.g., EndoGastric StomaphyX™ endoluminal fastener and delivery
system); laparoscopic gastric plication/laparoscopic greater curvature plication (LGCP), with or
without gastric banding; balloon-type systems (e.g., ReShape® Integrated Dual Balloon System
[CPT 43290, 42391, covered for Medicaid and Medicare only]) and vagus nerve-blocking devices
(e.g., MAESTRO® Rechargeable System).
Revision History
Jul. 14, 2023
Added SADI-S as covered procedure
Jun. 16, 2023
Clarified that CPT codes 43290 and 42391 are covered for Medicaid and Medicare only
Feb. 10, 2023
Added pediatric criteria
Aug. 12, 2022
Added Overstitch device as investigational
Dec. 10, 2021
Added case-by-case consideration language for preoperative esophagogastroduodenoscopy (EGD) for
members symptomatic of gastroesophageal reflux disease (GERD)
Feb. 12, 2021
Removed perquisite for 2 years of insufficient weight loss within Surgical Repetition criteria
Jul. 12, 2019
MCG Panniculectomy cross reference replaced with link to EmblemHealth’s reinstated
Abdominoplasty/Panniculectomy guideline, which communicates photo documentation requirement
Jun. 14, 2019
Modified sub criteria of “documented primary disease complication”:
“Medically refractory hypertension” changed to “Hypertension”
“Moderate to severe obstructive sleep apnea” changed to “Sleep apnea”
Jun. 8, 2018
Removed pre-surgical dieting prerequisite and statement that member must not have a life
threatening condition
Mar. 11, 2016
Clarified devices/techniques, within Limitations/Exclusions Section, which were determined by
EmblemHealth to be investigational
Applicable Procedure Codes
43290
Esophagogastroduodenoscopy, flexible, transoral; with deployment of intragastric bariatric balloon (eff.
1/1/2023) (Medicaid and Medicare only)
43291
Esophagogastroduodenoscopy, flexible, transoral; with removal of intragastric bariatric balloon(s) (eff.
1/1/2023) (Medicaid and Medicare only)
43644
Laparoscopy, surgical, gastric restrictive procedure; with gastric bypass and Roux-en-Y gastroenterostomy
(roux limb 150 cm or less)
43645
Laparoscopy, surgical, gastric restrictive procedure; with gastric bypass and small intestine reconstruction to
limit absorption
43659
Unlisted laparoscopy procedure, stomach
43770
Laparoscopy, surgical, gastric restrictive procedure; placement of adjustable gastric restrictive device (eg,
gastric band and subcutaneous port components)
43771
Laparoscopy, surgical, gastric restrictive procedure; revision of adjustable gastric restrictive device component
only
43772
Laparoscopy, surgical, gastric restrictive procedure; removal of adjustable gastric restrictive device component
only
43773
Laparoscopy, surgical, gastric restrictive procedure; removal and replacement of adjustable gastric restrictive
device component only
43774
Laparoscopy, surgical, gastric restrictive procedure; removal of adjustable gastric restrictive device and
subcutaneous port components
43775
Laparoscopy, surgical, gastric restrictive procedure; longitudinal gastrectomy (ie, sleeve gastrectomy)
43842
Gastric restrictive procedure, without gastric bypass, for morbid obesity; vertical-banded gastroplasty
43843
Gastric restrictive procedure, without gastric bypass, for morbid obesity; other than vertical-banded
gastroplasty
43845
Gastric restrictive procedure with partial gastrectomy, pylorus-preserving duodenoileostomy and
ileoileostomy (50 to 100 cm common channel) to limit absorption (biliopancreatic diversion with duodenal
switch)
43846
Gastric restrictive procedure, with gastric bypass for morbid obesity; with short limb (150 cm or less) Roux-en-
Y gastroenterostomy
43847
Gastric restrictive procedure, with gastric bypass for morbid obesity; with small intestine reconstruction to
limit absorption
43848
Revision, open, of gastric restrictive procedure for morbid obesity, other than adjustable gastric restrictive
device (separate procedure)
43860
Revision of gastrojejunal anastomosis (gastrojejunostomy) with reconstruction, with or without partial
gastrectomy or intestine resection; without vagotomy
43865
Revision of gastrojejunal anastomosis (gastrojejunostomy) with reconstruction, with or without partial
gastrectomy or intestine resection; with vagotomy
43886
Gastric restrictive procedure, open; revision of subcutaneous port component only
43887
Gastric restrictive procedure, open; removal of subcutaneous port component only
43888
Gastric restrictive procedure, open; removal and replacement of subcutaneous port component only
43999
Unlisted procedure, stomach
47562
Laparoscopy, surgical; cholecystectomy
47600
Cholecystectomy
S2083
Adjustment of gastric band diameter via subcutaneous port by injection or aspiration of saline (Commercial
and Medicaid only)
Applicable ICD-10 Diagnosis Codes
E66.01
Morbid (severe) obesity due to excess calories
Z68.35
Body mass index (BMI) 35.0-35.9, adult
Z68.36
Body mass index (BMI) 36.0-36.9, adult
Z68.37
Body mass index (BMI) 37.0-37.9, adult
Z68.38
Body mass index (BMI) 38.0-38.9, adult

Z68.39
Body mass index (BMI) 39.0-39.9, adult
Z68.41
Body mass index (BMI) 40.0-44.9, adult
Z68.42
Body mass index (BMI) 45.0-49.9, adult
Z68.43
Body mass index (BMI) 50-59.9, adult
Z68.44
Body mass index (BMI) 60.0-69.9, adult
Z68.45
Body mass index (BMI) 70 or greater, adult
Z68.54
Body mass index [BMI] pediatric, greater than or equal to 95th percentile for age [BMI of 40 or greater for
adolescents who have completed bone growth]
Z98.84
Bariatric surgery status
References
American Academy of Pediatrics. Clinical Practice Guideline for the Evaluation and Treatment of Children and
Adolescents With Obesity. 2023. https://publications.aap.org/pediatrics/article/151/2/e2022060640/190443/Clinical-
Practice-Guideline-for-the-Evaluation-and. Accessed July 20, 2023.
American College of Cardiology/American Heart Association Task Force. Guideline for the Management of Overweight
and Obesity in Adults. 2013. https://www.jacc.org/doi/full/10.1016/j.jacc.2013.11.004. Accessed July 20, 2023.
American Society of Metabolic and Bariatric Surgery. Updated Position Statement on Sleeve Gastrectomy as a Bariatric
Procedure. 2017: https://asmbs.org/app/uploads/2017/11/ASMBS-updated-position-statement-on-sleeve-gastrectomy.-
SOARD-Oct-2017-1.pdf. Accessed July 20, 2023.
Curr Pharm Des. 2011;17(12):1209-17. Bariatric surgery: indications, safety and efficacy. Ben-David K1, Rossidis G.
DeMaria EJ, Portenier D, Wolfe L. Obesity surgery mortality risk score: proposal for a clinically useful score to predict
mortality risk in patients undergoing gastric bypass. Surg Obes Relat Dis. 2007 Mar-Apr;3(2):134-40.
National Heart, Lung, and Blood Institute. Managing Overweight and Obesity in Adults. Systematic Evidence Review From
the Obesity Expert Panel, 2013. http://www.nhlbi.nih.gov/sites/www.nhlbi.nih.gov/files/obesity-evidence-review.pdf.
Accessed July 20, 2023.
New York Health Plan Association. Obesity Surgery Workgroup. Surgical Management of Obesity Consensus Guideline.
2004: https://ag.ny.gov/sites/default/files/press-releases/archived/nov28a_04_attach1.pdf. Accessed July 20, 2023.
Scand J Surg. 2015 Mar;104(1):18-23. doi: 10.1177/1457496914552344. Epub 2014 Sep 30. Changing trends in bariatric
surgery. Lo Menzo E1, Szomstein S1, Rosenthal RJ2.
Snow V, Barry P, Fitterman N, Qaseem A, Weiss K, for the Clinical Efficacy Assessment Subcommittee of the American
College of Physicians. Pharmacological and surgical management of obesity in primary care: a clinical practice guideline
from the American College of Physicians. Ann Intern Med. 2005;142:525-531.
Technology Evaluation Center. Newer techniques in bariatric surgery for morbid obesity. Assessment Program.
2003;18(10):1-52.
Technology Evaluation Center. Special report: the relationship between weight loss and changes in morbidity following
bariatric surgery for morbid obesity. Assessment Program. 2003;18(9):1-26.
The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). Guidelines for the Clinical Application of
Laparoscopic Bariatric Surgery. 2008: http://www.sages.org/publications/guidelines/guidelines-for-clinical-application-
of-laparoscopic-bariatric-surgery/. Accessed July 20, 2023.
Kim JJ, Rogers AM, Ballem N, Schirmer B. ASMBS updated position statement on insurance mandated preoperative
weight loss requirements. Surgery for Obesity and Related Diseases. 2016;12(5):955-959.
doi:10.1016/j.soard.2016.04.019.
Aminian A, Chang J, Brethauer SA, Kim JJ; American Society for Metabolic and Bariatric Surgery Clinical Issues Committee.
ASMBS updated position statement on bariatric surgery in class I obesity (BMI 30-35 kg/m(2)). Surg Obes Relat Dis. 2018
Aug;14(8):1071-1087. doi:10.1016/j.soard.2018.05.025. Epub 2018 Jun 9. Review. PubMed PMID: 30061070.

ASGE Standards of Practice Committee (2015). The role of endoscopy in the bariatric surgery patient. Surgery for Obesity
and Related Diseases, 11(3), 507-517. https://doi.org/10.1016/j.soard.2015.02.015. Accessed July 20, 2023.
Hayes inc. Evolving Evidence Review. OverStitch Endoscopic Suturing System (Apollo Endosurgery Inc.) for Transoral
Outlet Reduction. Lansdale, PA: Hayes Inc.; July 2022, amended July 2023.
Specialty matched clinical peer review.
