
Original Paper
Mobile Apps to Support Caregiver-Resident Communication in
Long-Term Care: Systematic Search and Content Analysis
Rozanne Wilson
1
, PhD; Diana Cochrane
1
, MHLP; Alex Mihailidis
2,3,4
, PhD; Jeff Small
1
, PhD
1
School of Audiology and Speech Sciences, Faculty of Medicine, The University of British Columbia, Vancouver, BC, Canada
2
Department of Occupational Sciences and Occupational Therapy, Faculty of Medicine, University of Toronto, Toronto, ON, Canada
3
Institute of Biomaterials and Biomedical Engineering, University of Toronto, Toronto, ON, Canada
4
Toronto Rehabilitation Institute, Toronto, ON, Canada
Corresponding Author:
Rozanne Wilson, PhD
School of Audiology and Speech Sciences
Faculty of Medicine
The University of British Columbia
2177 Wesbrook Mall
Vancouver, BC, V6T 1Z3
Canada
Phone: 1 6048225798
Email: r[email protected]
Abstract
Background: In long-term residential care (LTRC), caregivers’ attempts to provide person-centered care can be challenging
when assisting residents living with a communication disorder (eg, aphasia) and/or a language-cultural barrier. Mobile
communication technology, which includes smartphones and tablets and their software apps, offers an innovative solution for
preventing and overcoming communication breakdowns during activities of daily living. There is a need to better understand the
availability, relevance, and stability of commercially available communication apps (cApps) that could support person-centered
care in the LTRC setting.
Objective: This study aimed to (1) systematically identify and evaluate commercially available cApps that could support
person-centered communication (PCC) in LTRC and (2) examine the stability of cApps over 2 years.
Methods: We conducted systematic searches of the Canadian App Store (iPhone Operating System platform) in 2015 and 2017
using predefined search terms. cApps that met the study’s inclusion criteria underwent content review and quality assessment.
Results: Although the 2015 searches identified 519 unique apps, only 27 cApps were eligible for evaluation. The 2015 review
identified 2 augmentative and alternative cApps and 2 translation apps as most appropriate for LTRC. Despite a 205% increase
(from 199 to 607) in the number of augmentative and alternative communication and translation apps assessed for eligibility in
the 2017 review, the top recommended cApps showed suitability for LTRC and marketplace stability.
Conclusions: The recommended existing cApps included some PCC features and demonstrated marketplace longevity. However,
cApps that focus on the inclusion of more PCC features may be better suited for use in LTRC, which warrants future development.
Furthermore, cApp content and quality would improve by including research evidence and experiential knowledge (eg, nurses
and health care aides) to inform app development. cApps offer care staff a tool that could promote social participation and
person-centered care.
International Registered Report Identifier (IRRID): RR2-10.2196/10.2196/17136
(JMIR Aging 2020;3(1):e17136) doi: 10.2196/17136
KEYWORDS
mobile apps; communication barrier; dementia; caregivers; long-term care; patient-centered care
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 1http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

Introduction
Background and Rationale
With the growing aging population, there are more people living
with chronic conditions that contribute to physical, sensory
(vision/hearing), and cognitive limitations. The complex health
care needs of older adults living with chronic conditions may
require the services offered in long-term residential care (LTRC)
homes. Most LTRC residents (85%) are functionally dependent
and require care staff assistance (eg, nurse and residential care
aide) while completing activities of daily living (ADLs) [1],
and 25% of residents live with dual sensory loss (hearing and
vision) [2]. Besides physical and sensory limitations, an
estimated 90% of residents live with some cognitive impairment,
with 2 out of 3 residents living with Alzheimer disease and
related dementias (ADRD) [1]. Furthermore, many residents
experience communication difficulties associated with chronic
conditions (eg, sensory loss, dementia, and stroke) and/or a
cultural-language mismatch with care staff that can challenge
interpersonal relationships, and care staffs’ ability to meet
residents’ unique needs [3].
Implementation of a person-centered philosophy of care and
person-centered interventions in LTRC depends on effective
caregiver-resident communication [4]. Person-centered
communication (PCC) involves sharing information and
decisions between care staff and residents, being compassionate
and empowering care provision, and being sensitive to resident
needs, preferences, feelings, and life history [5]. By creating an
environment that uses strategies and tools to enhance PCC,
LTRC care staff can meet residents’ unique needs and foster
interpersonal relationships with the residents [6]. For example,
care staffs’ use of social and task-focused communication
strategies (eg, greet the resident and provide one direction at a
time, respectively) with residents living with dementia support
the successful completion of ADLs [7,8]. Verbal and nonverbal
behaviors (eg, use the resident’s name and make gestures)
contribute to positive communication between residents and
care staff with different linguistic/cultural backgrounds [3].
Although guidelines for supporting person-centered language
in LTRC exist [9], the LTRC setting faces many challenges that
can act as barriers to PCC. One such challenge is language
diversity. In countries that have a history of welcoming
immigrants (eg, Canada, the United States, and Australia), care
staff and residents with diverse linguistic and ethnocultural
backgrounds often comprise LTRC settings [10-14]. For
example, in Canada, most immigrant seniors live in urban areas
(eg, Vancouver and Toronto), with approximately 50% of the
Vancouver senior population being immigrants [15]. Similarly,
it is common to find that English is not the first language of
residential care aides, nor are they born in Canada [16].
Therefore, diversity in the LTRC setting is typical in major
Canadian urban areas, leading to mismatches between care staff
and residents’first language and/or ethnocultural backgrounds.
The shortage of qualified care staff, low wages among
residential care aides, and restrictions on who can provide
specific types of care can lead to a reduction in the time needed
to foster frequent, quality interpersonal interactions with
residents [17]. Finally, resource constraints inherent to the LTRC
setting (eg, time and staffing) can lead to task-focused care
rather than person-focused care and to fewer instances of
caregiver-resident interpersonal interactions [18].
Several traditional approaches to supporting caregiver-resident
communication have been tried in LTRC, including professional
medical translator services for non-English–speaking residents,
communication training programs [19], evidence-based
communication strategies [7,8], employing bilingual care staff
[20], and using augmentative and alternative communication
(AAC) techniques, tools, and strategies (eg, communication
boards and gestures). AAC can be used to address the needs of
residents living with acquired communication disorders (eg,
aphasia and dementia) by supplementing remaining speech
abilities or replacing the voice output when speech is no longer
viable [20,21]. Although the aforementioned supports can be
beneficial, they are often inaccessible to caregivers or residents
because of the limited time available for training and/or
implementation during care routines, limited funding, and
limited on-demand availability.
There is growing recognition of the potential role of technology
in supporting the health care of older adults [21], with a focus
on person-centered care [22-25]. In particular, the use of mobile
communication technology (MCT), which includes mobile
devices such as tablets and smartphones, along with their
software apps, offers an innovative approach for supporting
person-centered care. There are several advantages to using
MCT in health care settings: (1) the devices are accessible,
portable, small, lightweight, rechargeable, relatively easy to
use, and inexpensive, have advanced features (eg, camera and
sound recording), and have enough computing power to support
web searching; (2) a variety of apps are available in the major
app marketplaces; and (3) a wireless connection offers
continuous, simultaneous, and interactive communication from
any location [26].
In a short period, the availably of mobile apps has increased
exponentially across the 2 largest app marketplaces: Google
Play (Android platform) and the App Store (iPhone Operating
System [iOS] platform). For example, in 2014, there were an
estimated 2.6 million apps across the 2 marketplaces [27] and,
by 2019, this number climbed to 5.5 million apps (111%
increase) [28]. In addition to the convenience and commonplace
of MCT, the appeal of using apps in health care may be because
of the range of available built-in features that can support
individuals’needs, preferences, and abilities (ie, person-centered
care), including larger touch screen interfaces with tactile
feedback, motion sensors, voice recognition, cameras, video
recorders, and multimedia content (eg, images, sound, and text)
[29]. App content can also be customized to support the unique
needs of a target population. For example, apps designed for
older populations can incorporate larger text and zoom
capability; allow for preferred vocabulary, photos, and text; and
have the options to save voice and video recordings. Thus,
MCTs are useful tools for health care professionals and can
support target populations with specific needs, such as those
living with ADRD [29-32]. However, more information is
needed to determine how these technologies could address
specific challenges that caregivers encounter with target
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 2http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

populations (eg, dementia [33]) living in LTRC. Furthermore,
given the rapidly changing landscape of the app marketplace
(eg, new, updated, and removed apps), it is important to better
understand the stability of apps in the marketplace. The
longevity of apps has important implications in the LTRC
context. For example, for training care staff to use an app that
is subsequently removed from the marketplace would be a waste
of financial resources. The first step to examining the use of
MCT in the LTRC setting is to better understand the suitability
of currently available commercial apps for supporting
communication in the LTRC context and the stability of these
apps over time.
Using mobile devices, along with AAC apps and language
translation apps, collectively referred to as communication apps
(cApps) in this paper, may offer an innovative approach to
enhancing PCC in LTRC. In particular, cApps have the potential
to support care staff and residents living with acquired
neurogenic communication disorders [34] and/or
linguistic/ethnocultural barriers [14] during daily activities. For
example, cApps could be used as follows: (1) support residents’
participation in their own care; (2) help identify, save, and share
residents’ individualized needs and preferences during care
routines; (3) personalize activities and social engagement; (4)
support information sharing between care staff and residents
during daily care; (5) prevent and/or overcome communication
breakdowns during ADLs by meeting residents’unique needs;
and (6) promote social participation. However, to date, there
appears to be no evidence about the availability of cApps that
could support communication between care staff and LTRC
residents during daily care routines. Recently, regulations and
guidelines for the development and use of technologies in health
care have been developed [35]. However, the existing
commercially available apps were likely developed with limited
regulatory oversight, resulting in little evidence for the validity
and reliability of app content and questionable quality [36].
Therefore, we need to better understand the availability and the
content quality of currently available cApps. This information
will help to determine which cApp could be suitable for
supporting caregiver-resident communication in LTRC.
Research Aims
This app review aimed to systematically identify and examine
existing commercially available AAC and translation apps (ie,
cApps) that care staff could access to support PCC with LTRC
residents during daily activities. The specific objectives of this
study were as follows:
1.
To systematically identify commercially available apps
designed for adults living with a communication impairment
(AAC apps) and/or experiencing a language barrier
(translation apps).
2.
To assess cApp content (description of app characteristics
and PCC features), with a focus on suitability and relevance
to the LTRC setting.
3.
To assess the quality of eligible cApps, with a focus on
functionality, ease of use, and customization.
4.
To recommend the top existing cApps best suited for
supporting caregiver-resident communication during ADLs.
5.
To replicate the review to better understand how a rapidly
evolving app marketplace may impact the suitability and
longevity of cApps in the LTRC setting over a 2-year
period.
Methods
Identification Phase
Search Strategy
The systematic search for cApps in the Canadian marketplace
was conducted between April and June 2015 and involved 5
steps: (1) internet search for AAC and translation apps using
the Google search engine; (2) consultation with a
speech-language pathologist (SLP) with expertise and
knowledge in using AAC apps with adults living with a
communication impairment (ie, clinical expert) to identify AAC
apps recommended for use by adults living with a
communication impairment; (3) scientific literature search
focused on the use of mobile apps to support communication
in the LTRC setting; (4) preliminary search of the official
Canadian app stores of the 2 major operating systems (Android
and iOS): Google Play and App Store; and (5) comprehensive
search of the Canadian App Store (iOS platform; Figure 1).
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 3http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

Figure 1. Summary of the steps involved in the identification phase of the communication app reviews. Note that a consultation with a clinical expert
and a preliminary search were not conducted for the 2017 review. iOS: iPhone Operating System.
Initial Identification
To gain a better understanding of the scope of the relevant and/or
recommended AAC and translation apps available in the app
marketplace, a Google search, a consultation with a clinical
expert, a review of the scientific literature, and preliminary
marketplace searches were completed. The Google search was
conducted to help flag popular AAC and translation apps that
should appear in the marketplace searches. The Google searches
were done using a Google Chrome web browser by a single
author (RW) on the same PC laptop computer (Windows 8;
logged into a Google account) and involved separate searches
for AAC apps and translation apps (Table 1). Google algorithms
place the most relevant search results on the first result page
and the majority of searchers stay on the first page [37]. To
ensure comprehensiveness, the first 3 pages of the internet
search results (50 results per page) were screened for links to
specific apps and for links to websites that recommended apps
useful for older adults living with a communication impairment
or language barrier. Next, a consultation meeting with a clinical
expert took place. The SLP shared a detailed spreadsheet of
AAC apps that she used with her clients and identified which
AAC apps would be appropriate for adults living with a
communication impairment in the LTRC setting. The scientific
literature search was conducted to identify research reporting
on the use of MCT to address the communication needs of
vulnerable residents in LTRC. Searches were conducted in
MEDLINE, AgeLine, and the Cumulative Index to Nursing and
Allied Health Literature academic electronic databases in April
2015 and in February 2016 (RW). Broad search terms were
used to capture subdomains of communication
challenges/barriers, including language differences or aphasia.
Free vocabulary (keywords) and controlled vocabulary (eg,
Medical Subject Heading terms) were used for the combined
concepts (Table 1). No date restrictions were applied to the
searches and search results were limited to peer-reviewed
academic literature and the English language. No relevant results
were found in the literature searches. Finally, 2 reviewers
(authors RW and DC) performed a preliminary search of both
the App Store (iOS) and Google Play (Android) on a desktop
computer to assess which marketplace appeared to have the
highest inventory of AAC and translation apps. On the basis of
information gathered from the Google search, the clinical expert,
and the preliminary search of both market stores, the App Store
(iOS) had the highest inventory of AAC and translation apps.
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 4http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

Table 1. Search terms used in Google Chrome and electronic databases.
Search terms (controlled and free vocabulary)Search location
Google Chrome
Function
augmentative and alternative communication apps for smartphones or tablets
AAC
a
AAC apps for smartphones or tablet
adult augmentative and alternative communication apps for smartphones or tablets
adult AAC apps for smartphones or tablets
AAC apps for smartphones or tablets for frail elderly
AAC apps for smartphones or tablets for long-term care residents
AAC apps for smartphones or tablets in hospital for patients
communication app for adult patients
translation apps for smartphones or tabletsTranslation
translation apps for smartphones or tablets
medical and health care translation apps
Electronic databases
Population
older adult*, OR aging OR ageing, OR aged OR, senior*, OR elder*, OR frail elder*, OR dementia,
OR nursing home resident*
Older adults
AND
caregiver*, OR nurse*, OR nurse aide, OR health care aide*Caregivers
AND
communication, OR communication barrier, OR communication aids for disabled, OR assistive technol-
ogy, OR alternative and augmentative communication, OR AAC, OR communication disorder, OR
communication impairment
Communication barrier
AND
Intervention
smartphone*, OR computer*-handheld, OR tablet computer*, OR cell* phone, OR portable computer*,
OR mobile app*, OR software app*, OR computer software, OR app*
Mobile communication technology
AND
Outcome
Person-centred care, OR Personhood, OR person-centred communication, OR communication strategies,
OR person-centredness
Person-centered communication
AND
Setting
nursing home, OR long term care, OR institutional care, OR nursing home patient*, OR nurse-patient
relations, OR nurse attitude*
Long-term residential care
a
AAC: augmentative alternative communication.
App Store Search
For this study, the identification of AAC and translation apps
that support interpersonal communication between LTRC
residents and care staff during ADLs focused on a
comprehensive search of the Canadian iOS marketplace: App
Store for desktop computer searches and for mobile device
searches (tablet and smartphone). AAC apps were searched in
the medical, communication, education, lifestyle, and health
and fitness categories of the App Store. Several keyword
searches were conducted, with the keywords “AAC,” “AAC
communication,” “adult communication apps,” and
“communication disability” returning most of the search results.
The translation apps were searched in the medical education,
health and fitness, reference, productivity, utilities, and business
categories, using the keywords “translation apps,” “translate
apps,” “medical,” and/or “health care translator apps,” and
“multi-language translate.” To verify search results, 2 authors
(RW and DC) performed independent searches for AAC apps
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 5http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

and for translation apps in the App Store, producing similar
results.
Selection Phase
The iOS marketplace search results were exported to Microsoft
Excel, and a single reviewer (DC) removed duplicates and
screened the remaining apps (names/titles) for being foreign
(ie, non-English title) and/or unrelated to interpersonal
communication (eg, dictionary app). If the app’s name did not
clearly indicate that it was unrelated to communication or was
foreign, the app was included for eligibility screening. For apps
available in multiple versions, the complete version (ie, fully
featured, no limitations, and no in-app purchase required) was
included for eligibility screening and the less complete apps
were marked as duplicates. In the case of apps with multiple
versions that were identical except for the voice setting (male
or female), the adult female voice version was selected and the
other version was marked as a duplicate. This decision was
made because LTRC care staff are typically female [16].
Following the initial screening, the study’s inclusion and
exclusion criteria were applied (Textboxes 1 and 2). Two
reviewers (authors RW and DC) independently applied the
inclusion/exclusion criteria to approximately 20.0% of the apps
(AAC: 36/181; translation: 4/18) by reviewing the App Store
description. Following acceptable agreement, any disagreements
were discussed, with final inclusion/exclusion decisions based
on consensus. If needed, a third reviewer (JS) would assist in
the inclusion/exclusion decision. A single reviewer (DC) applied
the inclusion/exclusion criteria to all remaining apps. AAC apps
and translation apps that met all the inclusion criteria, and none
of the exclusion criteria, were included for metadata extraction,
feature coding, and quality assessment.
Textbox 1. Inclusion criteria for communication apps study eligibility.
•
Communication function: augmentative and alternative communication (AAC)
•
The app’s primary function is AAC for adults
•
Communication was included as a keyword or in the text description of the app
•
Can communicate basic needs (eg, feelings, emotions, preferences, and activities)
•
Available in English
•
Can support communication between a care provider and a patient in a health care setting
•
Can be customized to support individual needs and preferences
•
Includes all visual and auditory feedback functions (ie, images, text, and speech/sound)
•
Communication function: translation apps
•
The app’s primary function is language translation
•
Available in multiple languages
•
Incudes text-to-speech, speech-to-text, and speech-to-speech translation functions
•
Could be used over the web and offline (eg, download language libraries for offline use)
•
Option to save words/common phrases to a word bank on a tablet device
•
Customization option (eg, save favorite words for quick access)
Textbox 2. Exclusion criteria for communication apps study eligibility.
•
Communication function: augmentative and alternative communication (AAC)
•
Requires substantial changes/modifications to use in the long-term residential care setting during the completion of activities of daily living (eg,
need to import most images, create text and speech, add/delete built-in features)
•
No longer available in the Canadian App Store
•
Images are not adult appropriate (eg, child cartoon characters)
•
Unrelated to communication with adults living with a communication difficulty
•
Unrelated to communicating basic needs
•
Does not include all visual and auditory feedback functions (ie, image, text, and speech/sound)
•
Communication function: translation apps
•
Does not support human-language translation
•
Converting English to a single language was the only translation option
•
Text-to-text was the only available feature of the app
•
No longer available in the Canadian App Store
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 6http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

Evaluation Phase
Data Extraction for Content Analysis
Using a tablet device, a single author (DC) extracted the
metadata content for all eligible AAC and translation apps from
information provided in the Canadian App Store descriptions.
In addition, if available, information was extracted from the
developer’s website and/or through reviewing web-based
training modules or videos demonstrating the app. For content
analysis, the authors (RW and JS) developed a detailed feature
coding scheme to guide data collection for each cApp. For each
cApp, extracted descriptive data were entered into a standard
Microsoft Excel worksheet that contained the following
metadata categories: (1) general description: search date, app
name, app function, screenshot, keywords, and brief app
description; (2) technical information: marketplace/platform,
category, language, last software update, cost, and marketplace
longevity; (3) target user: general, living with a communication
disability, living with aphasia, and other; and (4) other: upgrade
with purchase, offline ability, technical support, translation
function, and indication of informed design (ie, SLP, clinician,
end user, and/or research was used to inform the development
of the app).
On the basis of the extracted metadata, a set of secondary
selection features were compiled for the AAC apps and for
translation apps (Textbox 3). These secondary selection features
were considered to be ideal characteristics of an app used in the
LTRC setting (eg, a low-cost app with technical support would
increase access and offer technical assistance to care staff) and
were strongly considered during the identification of the cApps
best suited to support PCC during ADLs in the LTRC setting.
Evaluated cApps were identified as having a secondary selection
feature by indicating yes or no for the presence or absence of a
feature.
Textbox 3. Secondary selection features.
•
Communication function: augmentative and alternative communication (AAC)
•
Low cost (app <Can $100 [US $75.5])
•
In the marketplace for at least two years (longevity/stability)
•
Web-based and offline capabilities
•
Technical support (email, phone, and web)
•
Includes a translation function
•
No cost/low cost for additional languages
•
Communication function: translation apps
•
Low cost (app <Can $100 [US $75.5])
•
In the marketplace for at least two years (longevity/stability)
•
Web-based and offline capabilities
•
Technical support (email, phone, and web)
•
No cost/low cost for additional languages
In addition, during the prepurchase review of the eligible cApps,
data were collected on built-in and customizable features that
support resident needs, preference, and feeling, as well as
sharing of information between residents and care staff (eg,
supports vision loss, option to add personal pictures, and
two-way communication). All built-in and custom features were
coded as being present (yes) or absent (no) in each app. The
detailed feature coding scheme aided in the identification of
cApps that included the highest number of PCC features (ie,
built-in and customizable) relevant to the LTRC setting.
Quality Assessment
For both the AAC and translation apps, quality assessment rating
criteria (Table 2) were derived from 3 dimensions of the Mobile
Application Rating Scale [38] that were deemed relevant to this
study: engagement (customization), functionality (ease of use),
and aesthetics (graphic presentation and visual appeal). Each
of the criteria was rated on a scale of 0 to 2 (0=poor, 1=fair,
2=good or 0=not at all easy, 1=somewhat easy, 2=easy). cApp
quality assessment was conducted in 2 steps: a prepurchase
quality assessment and a final quality assessment of purchased
cApps. During the prepurchase quality assessment step, 3
reviewers (authors RW, DC, and JS) independently applied the
quality assessment rating criteria to the cApps by reviewing the
store description, product tutorials/videos, or web-based videos
(eg, YouTube) or by downloading freely available cApps.
During the prepurchase evaluation, the initial quality assessment
did not include ratings on sound quality (AAC) and translation
accuracy because this information was typically unavailable
without purchasing the app. All apps were assessed in
alphabetical order. After ratings were complete, each reviewer
judged whether the app was suitable for supporting
communication in LTRC (yes/no/possible), followed by a
decision to purchase/download the app for further evaluation
(yes/no/maybe).
Following an independent review, the 3 authors convened to
comparatively discuss the apps’ initial quality assessment ratings
and the apps’ suitability for communication in LTRC.
Collectively, the reviewers generated a shortlist of cApps that
would be purchased/downloaded to undergo a final quality
assessment. Although the cApp ratings were deemed important
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 7http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

to the purchase/download decision, cApps that included features
appropriate for caregiver-resident communication in LTRC, as
well as cApps with customization abilities, were given a higher
degree of consideration in the purchase decision. In addition,
if there were disagreements between reviewers’ decision to
purchase/download a cApp, the undecided cApp was included
for further evaluation. Therefore, the approach taken to generate
the shortlist could result in the purchase/download of a cApp
with a lower median initial quality assessment rating, as well
as the decision not to purchase/download a cApp with a higher
initial quality assessment rating. Two reviewers (authors DC
and JS) independently documented their experience using each
shortlisted cApp and completed the final quality assessment for
the AAC and translation apps. All shortlisted apps were
downloaded to an iPad Mini 4 device with an iOS 9 operating
system and a 7.9″ display for a direct user experience.
Table 2. Quality assessment rating categories for communication apps.
Categories
b,c,d
Communication function
a
Augmentative and alternative communication
•
Sound quality: How intelligible is the audio output?
•
Graphic presentation: What is the visual interface quality (image resolution detail
[pixels] and image clarity)?
•
Visual interface presentation: What is the overall appeal of the app look (ie, color
display, patterns, lines, scale, image/text type, image/text appropriateness, and dis-
play options)?
•
Ease of use: Overall, how easy is it to use the software interface (ie, app is intuitive
to learn and requires minimal explanation to use; instructions are clear; simple,
straightforward display; quick access to common features and commands; well-or-
ganized [layout] and easy to navigate)?
•
Customization: How easy is it to customize the app?
Translation
•
Sound quality
•
Graphic presentation
•
Visual interface presentation
•
Ease of use
•
Translation accuracy: How accurate are the translated words/text
a
The maximum total score for the final quality assessment ratings=10 (augmentative and alternative communication and translation apps).
b
Sound quality, graphic presentation, visual interface presentation, and translation accuracy were rated on a scale of 0 to 2 (0=poor, 1=fair, 2=good).
c
Ease of use and customization were rated on a scale of 0 to 2 (0=not at all easy, 1=somewhat easy, 2=easy).
d
Sound quality and translation accuracy were only applied in the final quality assessment of purchased/downloaded cApps.
Final Recommendation Phase
Following the independent assessment of all cApps, 3 reviewers
(RW, DC, and JS) reconvened to discuss their experience with
each app. The final selection of the most suitable cApps in the
AAC category and in the language translation category was
determined by research team consensus and was based on the
combined findings of a three-stage comparative process
involving the review of the extracted feature data, the initial
quality assessment of eligible cApps, the user experience, and
the final quality assessment of the purchased cApps.
Replication Review
The identification phase of the replication review took place in
October 2017, and the evaluation phase was completed in July
2018. Apart from a consultation with a clinical expert, the
identification phase involved the same methodological approach
as the original 2015 review. Three trained research assistants
completed the Google search, the comprehensive iOS
marketplace search, and the initial screening (duplicates, foreign,
and unrelated), while 1 author (RW) conducted the scientific
literature search in October 2017. For the 2017 systematic app
review, all search terms used in the Google search, in the
comprehensive app store search, and in the literature search
were identical to the terms used in the 2015 search (Table 1).
As with the 2015 review, Google searches were performed using
the Google Chrome web browser and involved separate searches
for AAC apps and translation apps. A single research assistant
performed all AAC internet searches on the same PC laptop
computer, and a single research assistant performed all
translation searches on the same PC laptop computer. The
literature search returned no relevant results. To replicate the
2015 review, only the Canadian App Store (iOS platform) was
searched during the 2017 review.
Two reviewers (RW and DC) completed the selection,
evaluation, and recommendation phases of the 2017 replication
review. An agreement check was performed for eligibility
assessment, whereby 2 reviewers independently assessed
approximately 20.0% of the apps (AAC: 61/306; translation:
60/300). Following acceptable agreement, any disagreements
were discussed, with final inclusion/exclusion decisions based
on consensus and, if needed, a third reviewer (JS). A single
reviewer (DC) applied the inclusion/exclusion criteria to all
remaining apps. There were two instances in which the
procedure for the 2017 replication review differed from the
2015 review. First, multiple versions of the same app (eg, lite
[free] and pro [cost]) were treated as unique apps in the 2017
replication review because each version included different
features and was anticipated to have varying quality levels.
Therefore, a lite version may qualify for evaluation, whereas
the pro version may not because of the higher cost. Apps that
underwent software updates since the 2015 review were still
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 8http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

considered the same version of the app. Second, secondary
selection features were applied to eligible cApps before the
evaluation phase of the 2017 replication review to further narrow
the pool of cApps that underwent quality assessment. Only
cApps with all secondary selection features were evaluated in
the 2017 review. As with the 2015 review, all quality assessment
ratings were completed using an iPad mini 4 (iOS 12.2 operating
system and 7.9″ display).
Data Analysis
Descriptive statistics are used to summarize cApp
characteristics, PCC features, and quality assessment ratings.
To quantify change between the 2015 review and the 2017
replication review, the number and/or proportional
increase/decreases are reported, with numbers/percentages
presented from 2015 to 2017 (ie, from X to Y).
Results
Original Review
The 2015 App Store searches identified a total of 752 cApps
(AAC=614; translation=138). The search terms AAC, AAC
communication, and communication disability accounted for
90.4% (555/614) of all identified AAC apps. The search terms
translation apps and translate apps accounted for 72.5%
(100/138) of all translation apps identified in the initial search.
After screening for duplicates, foreign, and unrelated apps, a
total of 181 unique AAC apps and a total of 18 unique
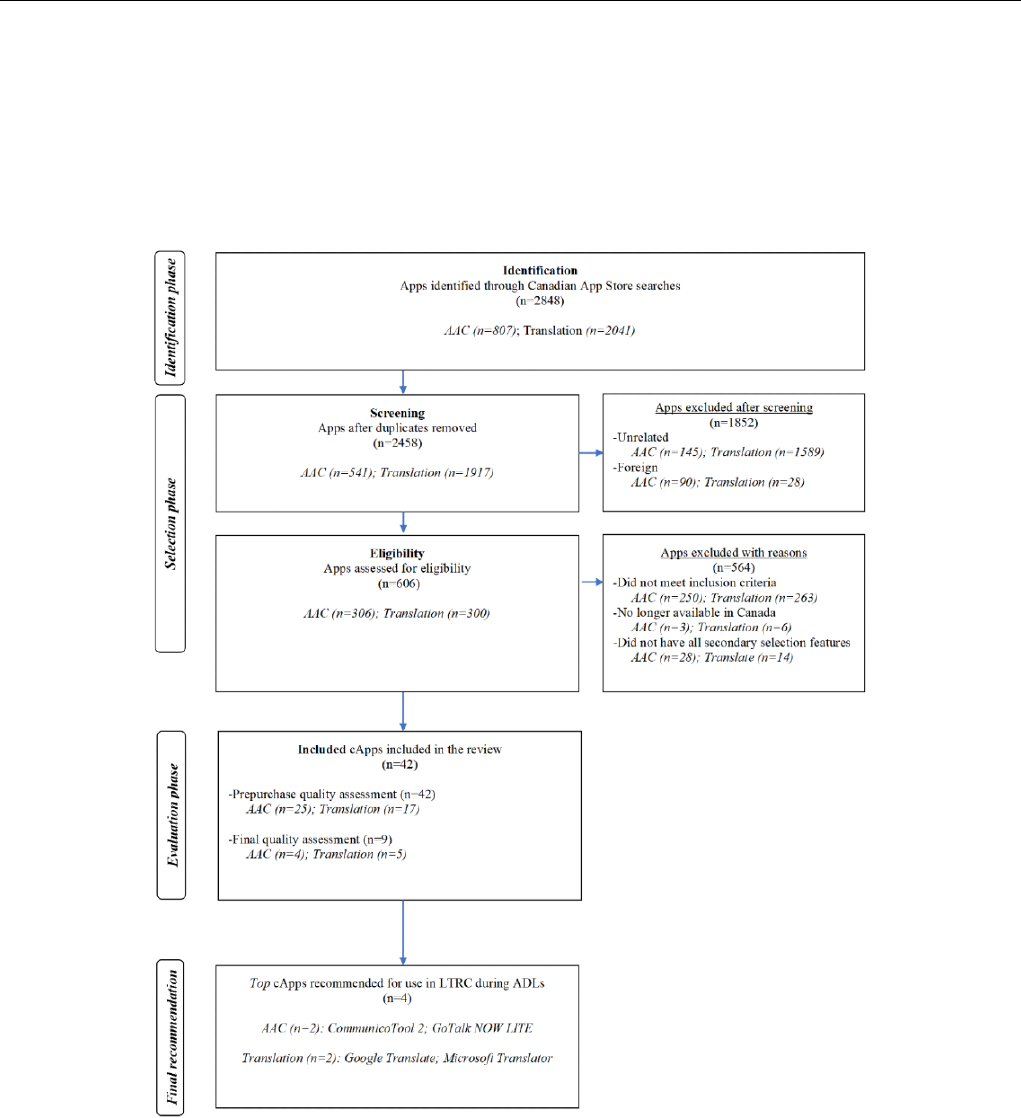
translation apps were identified. Figure 2 displays the 2015
search results, which was guided by the Preferred Reporting
Items for Systematic Reviews and Meta-Analyses flow diagram
template [39]. After applying this study’s inclusion/exclusion
criteria to the identified apps, 27 cApps were included in the
study (Tables 3 and 4).
Figure 2. Flow diagram summarizing the results of the identification, selection, evaluation, and final recommendation phases involved in the 2015
communication app review. The presentation of results was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow
diagram template AAC: augmentative and alternative communication; ADLs: activities of daily living; LTRC: long-term residential care.
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 9http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

Table 3. List of communication apps evaluated in the 2015 review.
AppsCategory
Augmentative and alternative communication (n=23)
•
Alexicom Elements Adult Home (Female)
a
•
App2Speak
a,b
•
AutisMate365
c
•
ChatAble
a
•
CommunicAide
•
CommunicoTool Adult
a,d
•
Compass (DynaVox)
•
Conversation Coach
a,b,d
•
Easy Speak—AAC
c
•
Functional Communication System
c
•
GoTalk NOW
a,d
•
iAssist Communicator
c
•
iCommunicate
a
•
image2talkb
b,e
•
MyTalkTools
a,d
•
PictureCanTalk
a,c
•
Proloquo2Go
a
•
Smart_AAC (med)
d
•
Sono Flex
a,d
•
SoundingBoard
•
Talkforme
c
•
TalkTablet
a,d
•
TouchChat AAC
Translation (n=4)
•
Google Translate
a,b
•
iTranslate
a,d
•
SayHi Translate
c
•
TableTop Translator
a,b
a
Indicates that this app met study eligibility in the 2015 review and in the 2017 review.
b
Indicates that the same version of the app was evaluated in the 2015 and in the 2017 reviews.
c
Indicates that this app was no longer available in the marketplace during the 2017 review.
d
Indicates that a different version of the same app was evaluated in the 2017 review (eg, 2015: CommunicoTool Adult; 2017 CommunicoTool 2).
e
For cApps with multiple versions, if a version of the cApp was evaluated in both the 2015 and in the 2017 review (eg, GoTalk NOW LITE and GoTalk
Start different versions [ie, fewer features] of GoTalk NOW), it was not categorized as a newly evaluated cApp.
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 10http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

Table 4. List of communication apps evaluated in the 2017 replication review.
AppsCategory
Augmentative and alternative communication (n=25)
a
•
App2Speak
•
CommunicoTool 2
•
Conversation Coach
•
Conversation Coach Lite
b
•
CoughDrop
c
•
Gabby
c
•
GoTalk NOW LITE
b
•
GoTalk Start
b
•
image2talk
•
iMyVoice Lite
b,c
•
iMyVoice Symbolstix
c
•
iSpeakUp
c
•
iSpeakUp Free
b,c
•
LetMeTalk
c
•
Mighty AAC
c
•
MyTalkTools Mobile Lite
•
SmallTalk Aphasia—Female
c
•
Sono Flex Lite
b
•
TAlkTablet CA AAC/Speech for aphasia
d
•
TalkTablet LITE—Eval Version
b
•
TalkTablet US AAC/Speech for aphasia
d
•
urVoice AAC—Text to speech with type and talk
c
•
Visual Express
c
•
Visual Talker
c
•
Voice4u AAC
c
Translation (n=17)
•
Google Translate
•
Instant Translator—Converse
c
•
iTranslate Translator
c
•
iTranslator—Speech translation
c
•
iVoice
c
•
LINGOPAL 44
c
•
Microsoft Translator
c
•
Multi Translate Voice
c
•
Online—Translator.com
c
•
Voice Translator Reverso
c
•
Speak & Translate—Translator
c
•
TableTop Translator
•
The Interpreter—translator
c
•
Translator with Speech HD
c
•
Translator—Speak & Translate
c
•
TravTalk—Talking & Recording Phrasebook
c
•
Yandex.Translate: 94 languages
c
a
For cApps with multiple versions, if a version of the cApp was evaluated in both the 2015 and in the 2017 review (eg, GoTalk NOW LITE and GoTalk
Start different versions [ie, fewer features] of GoTalk NOW), it was not categorized as a newly evaluated cApp.
b
cApps that were newly evaluated in the 2017 review.
c
A free or low-cost version of a fully featured app that is available for a higher cost.
d
A different version of the same app.
Content Analysis
Extracted metadata for the evaluated cApps indicated that 91%
(21/23) of AAC apps were only available for the iOS platform,
while 50% (2/4) of translation apps were available for both the
iOS and the Android marketplaces. The majority of AAC apps
(18/23, 78%) were categorized as education apps and most
likely included one or more of the following keywords: AAC
(18/23, 78%), communication disability (10/23, 43%), basic
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 11http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

needs (4/23, 17%), or daily living (4/23, 17%). Half of the
translation apps (2/4) were categorized as business apps and all
were labelled with the keyword translate. The majority of AAC
apps (18/23, 78%) identified people living with a communication
disability as the target user, whereas all translation apps (n=4)
were designed for a general audience. Most AAC apps were
available in English only (17/23, 74%), and the last software
update was within 1 year (17/23, 74%). All translation apps’
software was updated in the current year (ie, 2015). Some of
the free AAC apps were limited versions of an app that could
be upgraded with a purchase (eg, CommunicAide (free) and
CommunicAide Pro, Can $99.99 [US $75.5]), and the majority
(14/23, 61%) of AAC apps provided no indication of informed
design. Only 17% (4/23) of the AAC App Store description
and/or the developer’s webpage indicated the inclusion of an
SLP in the development of the app (App2Speak, Chatable,
CommunicAide Free, and CommunicoTool Adult), while 9%
(2/23) indicated research was used to inform the content
(Compass [DynaVox] and Proloquo2Go), and 13% (3/23)
included the end user (Talkforme, image2talk, and
MyTalkTools).
Most of the AAC apps cost Can $100 (US $75.5) or less (17/23,
75%), were available in the marketplace for 2 years or more
(18/23, 78%), and provided technical support (22/23, 96%;
Table 5). All translation apps cost less than Can $25 (US $18.9),
3 out of the 4 apps provided technical support, and the majority
(3/4, 75%) were available in the marketplace for 2 years or
more. Although about half of the AAC apps indicated some
offline functionality, only 1 translation app (Google Translate)
had limited offline functionality. Although no AAC app included
all secondary selection features, 83% (19/23) of the AAC apps
contained three or more of these features. GoTalk NOW,
SoundingBoard, AutisMate365, Conversation Coach, Functional
Communication System, and MyTalkTools contained the most
of these features. Except for online and offline capabilities, 75%
(3/4) of the translation apps included each of the secondary
selection features.
Appraisal of PCC features indicated that 3 AAC apps (GoTalk
NOW, Talkforme, and MyTalkTools) contained 11 or more of
the built-in and custom features. Only 1 AAC app contained all
5 custom features (GoTalk NOW) and 1 AAC app included
nearly all the built-in features (Talkforme). One translation app
contained 86% (6/7) of all applicable features (Google
Translate). Almost half of the AAC apps included 50% to 74%
of the features that were deemed to support PCC, and 75% (3/4)
of the translation apps contained some of the features (Table
6). Although all AAC apps indicated that they supported hearing
loss (eg, speech rate adjustment, voice customization, and
speech-to-text function), only 43% (10/23) supported vision
loss (eg, high-resolution images, zoom function, and large
images) and two-way communication (ie,
conversation/interpersonal). All translation apps supported
hearing and vision loss. Only 3 AAC apps included a built-in
translation function (Talkforme, MyTalkTools, and TouchChat
AAC). The majority of AAC apps included multiple display
modes, natural voice output, and text-to-speech output. The
ability to add personal photos/images and the option to add
personal voice recordings were the most common custom
features among the AAC apps, and all translation apps included
vocabulary customization.
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 12http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

Table 5. Secondary selection feature summary of the evaluated communication apps (cApps; note: as the percentages were rounded, some categories
may not add up to 100%.
Change over time, (%)
d
2017 replication review2015 reviewSecondary feature
TranslationAACTranslation (n=17)
c
, n (%)AAC (n=25)
b
, n (%)Translation (n=4), n (%)AAC
a
(n=23), n (%)
Cost in Can $ (low cost: app <Can $100 [US $75.5])
7613515 (88)10 (40)2 (50)4 (17)Free
−761672 (12)6 (24)2 (50)2 (9)<$25 (US $18.9)
0−470 (0)4 (16)0 (0)7 (30)$25-$49 (US
$18.9-US $37)
0−1000 (0)0 (0)0 (0)1 (4)$50-$75 (US
$18.9-US $37.8)
0−690 (0)1 (4)0 (0)3 (13)$75-$100 (US
$37.8-US $75.5)
0−380 (0)4 (16)0 (0)6 (26)>$100 (US
$75.5)
1−313 (76)19 (76)3 (75)18 (78)In the marketplace for
at least two years
(longevity/stability)
e
3007517 (100)25 (100)1 (25)13 (57)Web and offline capa-
bilities
f
25416 (94)25 (100)3 (75)22 (96)Technical support
(email, phone, web)
N/A−69N/A1 (4)
N/A
g
3 (13)Includes a translation
function
0N/A17 (100)N/A4 (100)N/ANo cost/low cost for
additional languages
a
AAC: augmentative and alternative communication.
b
In total, 11 AAC apps were evaluated in both the 2015 review and in the 2017 review.
c
In total, 3 translation apps were evaluated in the 2015 review and in the 2017 review.
d
A negative percentage indicates a decrease in the percentage of cApps with the secondary feature over the 2-year period.
e
The app copyright date was used to document marketplace longevity. In the absence of a copyright date, the oldest software update date was used.
f
Functions/features available offline may be limited compared with the features available during app use over the web.
g
Not applicable.
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 13http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

Table 6. Summary of features that support person-centered communication (PCC) in the evaluated communication apps (cApps; this table describes
PCC features found in the evaluated cApps during the 2015 review and in the 2017 replication review, as well as evaluates the percentage of cApps
with a PCC feature between the 2015 and 2017 reviews. Data were extracted from the Canadian App Store description and during the prepurchase
review of the cApps. Feature categories were not mutually exclusive; therefore, 1 app could have several built-in features and/or custom features).
Change over time, (%)
b
2017 review2015 reviewPerson-centered communication features
TranslationAACTranslation
(n=17)
AAC
(n=25), n
(%)
Translation (n=4),
n (%)
AAC
a
(n=23), n
(%)
Built-in features (n=9)
6−269 (53)8 (32)2 (50)10 (43)
Supports vision loss
c
−6016 (94)25 (100)4 (100)23 (100)
Supports hearing loss
d
−351511 (65)25 (100)4 (100)20 (87)
Multiple display representations
e
−68−311 (24)17 (68)3 (75)16 (70)
Natural sounding voice output
f
N/A4N/A25 (100)
N/A
g
22 (96)Text-to-speech function
N/A−56N/A1 (4)N/A2 (9)Speech-to-speech function
N/A−69N/A1 (4)N/A3 (13)Translation function
N/A26N/A11 (44)N/A8 (35)Available in multiple languages
−45−357 (41)7 (28)3 (75)10 (43)
Supports two-way communication
h
Custom features (n=5)
−2912712 (71)17 (68)4 (100)7 (30)
Can customize vocabulary
i
−28−33 (18)19 (76)1 (25)18 (78)Can add/save personalized photos/images
N/A−9N/A8 (32)N/A8 (35)Can to add/save personalized text
N/A−8N/A15 (60)N/A15 (65)Option to add/save personal voice record-
ings
N/A41N/A6 (24)N/A4 (17)Can add/save personalized videos
Total number of features
j
N/AN/A0 (0)0 (0)0 (0)0 (0)
cApps
k
with all applicable features
−28−383 (18)2 (8)1 (25)3 (13)cApps with most features (approximately
75% or more)
−3708 (47)12 (48)3 (75)11 (48)cApps with some features (approximately
50%-74%)
N/A136 (35)11 (44)0 (0)9 (39)cApps with few features (less than 50%)
a
AAC: augmentative and alternative communication.
b
Percent change calculation: ([percentage of 2017 apps with the feature−percentage of 2015 apps with the feature]/percent of 2015 apps with the
feature)*100. A negative percentage indicates a decrease in the percentage of cApps with the person-centered communication feature over the 2-year
period.
c
Features that support vision loss include high-resolution images, zoom function, and large pictures/text.
d
Features that support hearing loss include volume control, earbud option, speech rate adjustment, voice customizations, and speech-to-text function.
e
Multiple display representations indicate that the app includes two or more features: text, handwriting option, speech input, camera/photo pictures,
images, symbols, and video.
f
Information about voice output was not available for 4 AAC apps during the data extraction phase.
g
Not applicable.
h
Supports two-way communication means that the app could be used for caregiver-resident task-focused and/or interpersonal-focused communication
(eg, conversation view).
i
Option to customize vocabulary includes saving frequently used words/phrases in the following manner: pages, favorite lists, history, and add personalized
vocabulary.
j
A total of 14 person-centered features applied to AAC apps (built-in=9; custom=5). A total of 7 person-centered features were applicable for translation
apps (built-in=5; custom=2).
k
cApp: communication app.
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 14http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

Quality Assessment
Initial quality assessment of the eligible cApps indicated that 7
AAC apps were highly rated: Alexicom Elements Adult (median
8), TalkforMe (median 8), App2Speak (median 7),
CommunicAide (median 7), CommunicoTool Adult (median 6),
Functional Communication System (median 6), and GoTalk
NOW (median 6). After considering secondary selection features
and the initial quality assessment during a research team
discussion, 9 AAC apps and 3 translations apps were shortlisted
for purchase/download (Table 7). Following completion of the
final quality assessment ratings for each of the shortlisted cApps,
CommunicoToolAdult and GoTalkNOW had the highest median
ratings for AAC apps (Table 7). The research team reconvened
for a final comparative review of the cApps. On the basis of
consensus decisions, the top recommended cApps were
finalized: CommunicoTool Adult, GoTalk NOW, Google
Translate, and TableTop Translator (Multimedia Appendix 1).
Although TableTop Translator and SayHi shared the same
developer, the researchers selected TableTopTranslator because
this app included more language options and the screen display
supported two-way communication.
Table 7. Communication apps downloaded for final quality assessment ratings (the final quality assessment rating is based on the median rating of 2
reviewers. The maximum total rating score for cApps apps was 10).
Quality assessment ratings
cApp communication function and name
a
2017 search (n=8)2015 search (n=12)
Augmentative and alternative communication
8.56.5App2Speak
8.5
b,c
9
b
CommunicoTool Adult
N/A
d
5Functional Communication System
8
b,e
7.5
b
GoTalk NOW
N/A0iAssist Communicator
N/A3iCommunicate
N/A0image2talk
N/A1SoundingBoard
N/A1.5Talkforme
Translation
9.5
b
8
b
Google Translate
9.5
b
N/AiVoice Translator
10
b
N/AMicrosoft Translator
8N/AOnline-Translator.com
8.5
8
b
TableTop Translator
f
N/A8SayHi Translate
a
Communication apps (cApps) are listed in alphabetical order.
b
Top recommended cApps for use in long-term residential care to support communication between residents and caregivers.
c
CommunicoTool 2 was evaluated in the 2017 review.
d
Not applicable.
e
GoTalk NOW LITE was evaluated during the 2017 review.
f
TableTop Translator and SayHi shared the same developer.
Replication Review
Content Analysis
Following a comprehensive search of the App Store and the
removal of duplicates, foreign, and unrelated apps, a total of
607 apps were screened for study eligibility (Figure 3). A total
of 93 apps met the study’s inclusion criteria. After applying the
secondary selection features to further narrow down the pool
of cApps, a total of 42 apps were evaluated (AAC: n=25;
translation: n=17; Tables 3 and 4). In all, 36% (9/25) of the
evaluated AAC apps were a different version of the same app
(eg, Conversation Coach and Conversation Coach Lite). A total
of 28% (7/25) of the evaluated AAC apps were a low-cost or
free version of an app that was also available in a fully featured
version for a greater cost (Tables 3 and 4). None of the evaluated
translation apps was a different version of the same app. The
majority of the AAC apps were available only for the iOS
platform (19/25, 76%), cost less than Can $25 (US $18.9) or
were free (16/25, 64%), and were only available in English
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 15http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX
(14/25, 56%). Only 3 AAC apps indicated informed design
(SLP: Apps2Speak and Voice4u AAC; end user: image2talk),
and only 1 AAC app included a translation function
(LetMeTalk). Most translation apps were only available in the
iOS marketplace (15/17, 88%), were available for 2 years or
longer (13/17, 76%), were free (15/17, 88%), and offered
technical support (16/17, 94%). All translation apps had recent
software updates and had some offline functions (Table 5).
Figure 3. Flow diagram summarizing the results of the identification, selection, evaluation, and final recommendation phases involved in the 2017
communication app replication review. The presentation of results was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses
flow diagram template AAC: augmentative and alternative communication; ADLs: activities of daily living; LTRC: long-term residential care.
The majority of cApps contained at least some PCC features
(AAC: 14/25, 56%; translation: 11/17, 65%; Table 6). The AAC
apps with the highest number of PCC features were GoTalk
NOW LITE (11/14), GoTalk Start (11/14), and CommunicoTool
2 (10/14). The translation apps with the highest number of PCC
features were Google Translate (6/7), TableTopTranslator (6/7),
Translator with Speech HD (6/7), Microsoft Translator (5/7),
Multi Translate Voice: Say It (5/7), and Voice Translator
Reverso (5/7). All AAC apps supported hearing loss, included
multiple display representations, multiple output modes, and a
text-to-speech function, while very few included a
speech-to-speech function or a translation function.
Quality Assessment
All cApps that underwent final quality assessment were highly
rated (Table 7). On the basis of researcher consensus, the
following cApps were deemed to be best suited for supporting
communication between residents living in LTRC and their
caregivers during ADLs: GoTalk NOW LITE, CommunicoTool
2, Google Translate, and Microsoft Translate (Multimedia
Appendix 1). Although App2Speak was rated higher than GoTalk
NOW LITE, the app contained fewer PCC features than GoTalk
NOW LITE (8 and 11, respectively) and fewer features than
CommunicoTool 2. Importantly, App2Speak included only 2
custom features (add personal pictures and voice recordings)
compared with GoTalk NOW LITE, which contained 4 custom
features.
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 16http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

Stability of Evaluated Communication Apps Over Time
Between the 2015 review and the 2017 replication review, the
number of AAC apps identified in the iOS marketplace increased
by 31.4% (from 614 to 807) and the number of identified
translation apps increased exponentially (from 138 to 2041;
Figures 2 and 3). In all, 61% (14/23) of the eligible AAC apps
in the 2015 review also met study eligibility in the 2017 review
(Tables 3 and 4). Of the 2015 eligible/evaluated AAC apps,
35% (8/23) were no longer available in the marketplace in 2017.
Two AAC apps identified in the 2015 review were excluded in
the 2017 review because one required a substantial change for
use in the LTRC setting and the other included images that were
not adult appropriate (eg, child cartoon images; SoundingBoard
and TouchChat AAC, respectively). Finally, 1 AAC app was
excluded from the 2015 review but was deemed eligible in the
2017 review (Gabby). The images in Gabby were categorized
as not adult appropriate in the original 2015 review; however,
the updated version of Gabby contained images that were
considered adult appropriate. Except for the SayHi app, which
is no longer available in the App Store, all translation apps that
were eligible in the 2015 review also met study inclusion in the
2017 review.
A similar number of AAC apps were evaluated in the 2015 and
the 2017 reviews (n=23 and n=25, respectively). Of the 25 AAC
apps evaluated in the 2017 review, 3 (12%) were the same
version of the app evaluated in the 2015 review (App2Speak,
Conversation Coach, and image2talk) and 9 (36%) were a
different version of the same app evaluated in the 2015 review
(eg, Conversation Coach Lite and Sono Flex Lite; Tables 3 and
4). Notably, CommunicoTool Adult (2015 review) was no longer
available in the App Store and was replaced by CommunicoTool
2 (2017 review). For this study, CommunicoTool 2 was
considered a different version of the same app because its
features were quite like those of CommunicoTool Adult.
Although GoTalk NOW was the only version of the app that
was evaluated in the 2015 review, GoTalk NOW, GoTalk NOW
PLUS, GoTalk NOW LITE, and GoTalk Start were all eligible
versions of the same app in the 2017 review. After applying the
secondary selection criteria, only GoTalk NOW LITE and
GoTalk Start were evaluated in the 2017 review because these
versions were classified as low cost (<Can $100 [US $75.5]).
The cost of GoTalk NOW increased by 22% (from Can $89.99
[US $67.9] to Can $109.99 [US $83.1]). The number of
evaluated translation apps increased by 325% in the 2017 review
(from 4 to 17). Three of the four translation apps (75%)
evaluated in the 2015 review were also evaluated in the 2017
review.
Stability of Communication App Features Over Time
Over the 2-year period, the majority of the evaluated cApps
were only available for the iOS marketplace; however, the
largest increase was observed in the percentage of AAC apps
available across both iOS and Android platforms (167%; from
2/23, 9% to 6/25, 24%), and a decrease occurred among the
translation apps (76%; from 2/4, 50% to 2/12, 12%). Between
2015 and 2017, the majority of AAC apps continued to indicate
that adults living with a communication disability were the
target user, while translation apps continued to target the general
users. There was a 44% increase in the percentage of AAC apps
with no indication of informed design (from 14/23, 61% to
22/25, 88%), and the largest percent decrease was seen in AAC
apps that included a translation function (69%; from 2/23, 13%
to 1/25, 4%). For the secondary selection features (Table 5),
only two remained stable over time across cApps: in the
marketplace for 2 years or more and available technical support.
The largest percent change increase was observed in AAC apps
that were free (135%; from 4/23, 17% to 10/25, 40%) or cost
less than Can $25 (US $18.9; 167%; from 2/23, 9% to 6/25,
24%) and in translation apps that included web-based and offline
capability (300%; from 1/4, 25% to 17/17, 100%).
For PCC features, the overall percentage of AAC apps that
included approximately 50% to 74% of the PCC features
remained stable over the 2-year period (48%), whereas the
percentage of evaluated translation apps with at least some PCC
features decreased by 37% between 2015 and 2017 (from 3/4,
75% to 8/17, 47%; Table 5). Many of the custom PCC features
included in AAC apps remained stable over the 2-year period,
specifically features that supported hearing loss, used a natural
sounding voice output, included a text-to-speech function, and
offered an option to add/save personalized photos/images.
Between 2015 and 2017, the largest percent increase occurred
among AAC apps that included an option to customize
vocabulary (127%; from 7/23, 30% to 17/25, 68%), whereas
the largest decrease occurred for the percentage of AAC apps
that included a translation option. Over the 2-year period,
translation apps witnessed the largest decrease among the
percentage of apps that included a natural sounding voice (68%;
from 3/4, 75% to 11/25, 24%), whereas the percentage of
translation apps that supported two-way communication
decreased by 45% (from 3/4, 75% to 7/25, 41%).
Discussion
Principal Findings
This study’s comprehensive review of cApps available in the
iOS marketplace aimed to identify and assess the features and
quality of cApps that would be most appropriate for use with
residents living in LTRC homes. In addition, this study
examined the stability/instability of cApps over a 2-year period.
The 2015 review process culminated in selecting 2 AAC apps
(CommunicoTool Adult and GoTalk NOW) and 2 language
translation apps (Google Translate and TableTop Translate)
that provided the most suitable overall content and usability
features for enhancing communication between care staff and
residents living in LTRC. For purposes of augmenting
communication with images, video, sound, and text, these top
2 AAC apps contained features and functionality that promote
a multimodal understanding of messages, appealing and
high-quality images and audio/video capabilities, and the
capacity to customize content to individuals. One of these AAC
cApps, GoTalk NOW, has received an endorsement from
researchers in the field of AAC [40]. The top 2 language
translation apps in the 2015 review offered features that provided
high-quality voices, accurate translation, the capacity to save
commonly translated phrases, and versatility in translating across
modalities (eg, text to speech). Together, these 4 cApps provide
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 17http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

a promising starting point for integrating communication
technology into LTRC person-centered care practices. It is
interesting to note that, during the predownload initial quality
assessment, the top recommended cApps did not have the
highest median quality assessment ratings. For example,
Alexicom Elements Adult, Talkforme, App2Speak, and
CommunicAide received the highest median rating for AAC
apps, and SayHi Translate was the highest-rated translation app.
However, once the shortlisted cApps were downloaded and
used, the respective features, functionality, and usability of the
top recommended cApps were judged to be superior to all the
other downloaded apps. For example, CommunicoTool Adult
included the option to have a human voice, the built-in photos
were clear and relevant, and the app was customizable, and
GoTalk NOW was easy to use, had several built-in and
customizable features, and the stock pictures were relevant.
Google Translate allowed for web-based and offline (ie, saved
phrases) functions, was free, and was easy to use, whereas
TableTop Translator supported face-to-face conversation with
a unique split-screen function.
Overall, the majority of cApps evaluated in 2015 (20/27, 74%)
demonstrated marketplace stability over a 2-year period. In the
2017 review, only one of the top recommended cApps from the
2015 review was replaced with a newly evaluated translation
app, whereas the top AAC apps were different versions of the
same app recommended in the 2015 review. The decision to
recommend Microsoft Translator over TableTop Translator
was based on several factors. The visual interface quality, the
sound quality, and the visual interface presentation of Microsoft
Translator were rated higher compared with TableTop
Translator. Also, TableTop Translator uses Microsoft for
translations, had not undergone any recent updates, and the app
crashed several times while attempting to translate when using
the app. Although CommunicoTool Adult was replaced by
CommunicoTool 2, the newer version remained a top
recommended cApp for use in the LTRC setting to support
caregiver-resident communication during ADLs.
Although many of the AAC apps evaluated in 2015 and in 2017
include features and functionality that could support
communication between LTRC staff and residents (ie, support
hearing loss, included multiple display options, a text-to-speech
function, add personal photos; technical support), less than half
of AAC apps contained some (ie, 50%-74%) of these features.
For instance, in both reviews, there was a limited number of
evaluated AAC apps that supported two-way communication,
included a speech-to-speech option or a translation function,
supported vision loss, or provided options to add/save
personalized text or videos. Moreover, the majority of AAC
apps provided no indication of informed design, with less than
10% indicating SLP involvement in the design/development of
the app. Importantly, it appears that none of the cApps, including
the ones shortlisted in the 2015 and 2017 reviews, were
specifically developed to support PCC, particularly with frail
elderly residents living with sensory, motor, or cognitive
impairments, and/or language barriers. For example, the stored
voices linked to images in AAC apps (eg, speaking the word
orange when clicking on image of orange) and translator’s
voices have not taken into account the potential impact of
speaker/listener dialect or accent, nor the use of male versus
female voice, on residents’and staff’s ability to understand the
voice. The images on these apps are also generic, which means
that some of the images are not relevant for the LTRC context
because they have a different appearance than what is
encountered in the resident’s specific care environment (eg,
dining area, shower, and meals or snacks). Using voices from
the same dialect of the residents with voice qualities that
accommodate to the high-frequency hearing loss of many
residents, along with images that align with elderly residents’
current and previous life experiences, is an important way to
reduce the information processing demands of residents and
maximize their familiarity with the content. In view of older
adults’reluctance to learn new technologies, making the content
as relevant and meaningful to their life experience and current
needs should promote person-centered care and, thereby, greater
acceptance of MCT and cApps during their daily activities.
All AAC apps that were evaluated in both the 2015 and 2017
reviews claimed to support hearing loss by offering volume
control and input for listening devices (eg, earbuds). In addition,
some AAC apps provided an option to adjust the speech rate,
to customize the voice output, or to use a speech-to-text
function. Although these features can enhance one’s listening
experience, the technical specifications are not capable of being
adapted to different hearing loss profiles. Therefore, future apps
found in the iOS marketplace should be designed to interface
with hearing aid apps (eg, Mobile Ears) running on mobile
devices [41]. The significance of meeting the hearing health
needs of elderly residents in LTRC is apparent when considering
that most residents in LTRC are living with hearing loss [42]
and that failing to accommodate to their hearing loss can have
repercussions on their cognitive and social well-being [2,43,44].
For example, Amieva et al [45] reported that people living with
hearing loss who use hearing aids or other assisted listening
devices are much less likely to experience cognitive decline
than those who do not use hearing supportive devices. These
authors also provided evidence that ensuring persons with
hearing loss use their hearing aids is an important factor in the
person’s likelihood of using new technologies (eg, smartphone).
Given that hearing aid use enables persons to engage in
communication, it would follow that the use of other types of
communication enhancement devices, such as cApps with
features that support hearing, could be used in conjunction with
hearing aids to help maintain cognitive and social functioning
in aging and dementia. Future research is needed to explore the
potential long-term benefits to cognitive and social health
associated with regular use of hearing aids (or other assistive
listening devices) and cApps in LTRC.
Many older adults in LTRC also experience significant declines
in their vision [46]. This challenge can be addressed to some
extent by ensuring residents are wearing appropriate corrective
lenses and that the size of the images and text fonts is enough
for each resident’s vision needs. However, because MCT devices
are small, the upper range of expanding images and text is highly
constrained by the size of the device. Consequently, there is a
need for accommodating the visual needs of residents while
maintaining portability. One possible solution yet to be realized
would be to pair the MCT device (eg, tablet) that care staff use
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 18http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

with special glasses for the resident that connect wirelessly to
the MCT, allowing the image or text to be projected up close
[47]. Another option, also yet to appear on the market, would
be to use an MCT device that has an easy-to-use
expandable/retractable display.
Other potential obstacles to overcome in using cApps effectively
in LTRC relate to constraints on care staff in employing cApps
during ADLs and on residents’physical abilities to interact via
an MCT device. First, the demands on staff attending to multiple
residents within a short period would require that the cApps be
easily accessed in terms of activating a resident’s customized
cApp profile. This would entail having an umbrella home page
that links to each resident’s profile, a function that is currently
not available on any cApps. Second, the staff are often engaged
in care activities that require them to use both arms and hands,
making it difficult to switch between care tasks and the use of
an MCT device. Staff would need to plan their care activities
in such a way that accessing the cApp does not interfere with
the task or risk injury to either them or the resident. A related
constraint is that care activities require staff to be very mobile,
frequently bending over, while they assist residents during
ADLs. These demands would make it necessary for the MCT
device to be as small as possible so that it could be positioned
in an easily accessed, yet secure, pocket/holster. As mentioned
above, the size of an MCT device limits the size of images and
text appearing on the cApp. This double-edged challenge of
portability and resident user feasibility will require creative
technical and functional solutions. As Reis et al [48] note,
“technologies should complement and enhance service delivery
and never impose themselves as an extra burden on already
work-overloaded health professionals” [48]. Other challenges
for successful use of cApps in LTRC include the need for care
staff to have access to Wi-Fi, to be able to seamlessly update
and transfer customized settings across different care staffs’
MCT devices, and to be provided with ongoing training on how
to effectively use MCT in a person-centered way during
activities that are often physically and emotionally demanding.
From the resident’s perspective, the use of technology for the
current generation of residents is usually a novel experience
and one that may be confusing and/or unappealing to them [49].
For this reason, it would be important to introduce cApps and
MCT in a gradual fashion, perhaps beginning with a minimally
demanding app such as passively listening to music [50,51].
Once a resident gets accustomed to the device, a caregiver can
try out additional features and functions based on the resident’s
needs, abilities, and preferences. A second, and related,
constraint for residents’ use of cApps is their limited capacity
to point to, touch, or drag/swipe because of their lack of
familiarity with a cApp interface as well as their diminished
fine motor skills and tactile sensitivities (see Armstrong et al
[29] for a detailed discussion). Manufacturers of MCT devices
and cApps should consider how the user interface could be more
suitably adapted to accommodate older adults’ motor and
sensory capacities.
Limitations
Although this study is the first to systematically search the app
marketplace to identify and evaluate AAC and translation apps
that would be suitable for use in the LTRC setting to support
caregiver-resident communication, the review was limited to
cApps found in the Canadian (English) iOS marketplace.
Therefore, future research is needed to systematically review
cApps available in additional platforms and app stores (eg,
Google Play). To better understand the ways that cApps may
change in the marketplace over time, we compared two time
points: 2015 and 2017. Therefore, the percent changes reported
in this study cannot be interpreted as trends in the marketplace.
Finally, given the fast-changing landscape of the mobile app
marketplace, future research should consider performing an app
store search to verify the continued availability of the top
recommended apps reported in this study.
Future Directions
To date, there is limited empirical research published on the
use of mobile technology to support caregiver-resident
communication in LTRC, and there is no available evidence to
support the use of any of the identified cApps for
caregiver-resident communication. Therefore, there is a need
for future research to empirically examine the feasibility of
using currently available cApps in the LTRC setting, as well as
identify gaps in the use of this technology within different LTRC
contexts. A better understanding of how care staff could use
cApps to support PCC in LTRC should lead to improved quality
of care and quality of life for residents living in LTRC homes.
Conclusions
The use of cApps may offer an innovative solution to support
person-centered health care for residents living in LTRC homes.
This study identified several cApps available in the App Store
that aim to facilitate adult communication in general; however,
very few cApps were designed with built-in features and custom
features that would effectively support PCC in the LTRC setting.
Although comparisons of our top-rated cApps demonstrated
the inclusion of features that are potentially useful for supporting
PCC, there was no indication that the currently available cApps
were specifically designed for use in the LTRC setting to
enhance caregiver-resident communication during ADLs.
Furthermore, no cApp developer appeared to involve
stakeholders (eg, clinicians, researchers, residents, and care
staff) in the development and design process.
The ubiquitous nature of MCT (tablets/smartphones and their
apps) and the growing use of mobile health in a variety of health
care settings offer nurses and residential care aides an accessible
and innovative tool to promote social participation and
person-centered care. However, it is important to identify the
availability and stability of commercially available cApps, as
well as to conduct comprehensive reviews of the content and
quality of existing apps, to ensure that cApps can be used to
overcome communication barriers in the LTRC setting.
Moreover, to improve the content and quality of cApps and to
maximize the benefits of using mobile technology in care
practices, it is imperative to include nurses and other care staff
in the future development and design of cApps used in LTRC.
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 19http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

Acknowledgments
This study was supported by the Canadian Frailty Network (Technology Evaluation in the Elderly Network), which is supported
by the Government of Canada through the Networks of Centres of Excellence program. The TVN Health Technology Innovation
Grant (HTIG2014-20) was awarded to JS, AM, and RW. The content of this paper is solely the responsibility of the authors and
does not necessarily represent the policy of TVN.
The authors are grateful for the support of Patricia Dowden, PhD, CCC-SLP (Speech & Hearing Sciences, the University of
Washington) for her contribution to the identification of available cApps for supporting communication with adults living with
a communication impairment during the 2015 app review. The authors also thank Tiffiny Zang, Sarah Mermuys, Laura Murray,
and Kelly Salmon for their valuable research assistant support during the identification and initial screening phases of the 2017
review. A portion of this material was presented [poster] at the Canadian Association on Gerontology 47th Annual Scientific and
Education Meeting, Vancouver, British Columbia, Canada, October 18-20, 2018.
Authors' Contributions
RW, AM, and JS contributed to the study conception and design. RW made significant contributions to all aspects of the study
(data collection, data analysis, and reporting) and led the writing of the first draft of the paper. JS supervised the project, contributed
to the development of data collection tools, evaluated the cApps (2015 review), assisted in the coordination of the study, and
contributed to the first draft of the paper and revisions of the manuscript. DC performed the 2015 search, screened the apps,
extracted extraction (2015/2017), evaluated cApps (2015/2017), and contributed to the first draft and paper revisions. AM
commented on/revised the manuscript critically for important intellectual content. All authors take responsibility for the integrity
of the data and the accuracy of the data analysis. All authors read and approved the final manuscript.
Conflicts of Interest
None declared.
Multimedia Appendix 1
Screenshots of the top-recommended communication apps reviewed in 2015 and 2017.
[PDF File (Adobe PDF File), 349 KB-Multimedia Appendix 1]
References
1. Ontario Long Term Care Association. Ontario Long Term Care Association. 2018. This is Long-term Care 2018 URL:
https://www.oltca.com/OLTCA/Documents/Reports/Thisislongtermcare2018.pdf [accessed 2020-01-26]
2. Guthrie DM, Declercq A, Finne-Soveri H, Fries BE, Hirdes JP. The health and well-being of older adults with dual sensory
impairment (DSI) in four countries. PLoS One 2016;11(5):e0155073 [FREE Full text] [doi: 10.1371/journal.pone.0155073]
[Medline: 27148963]
3. Small J, Chan SM, Drance E, Globerman J, Hulko W, O'Connor D, et al. Verbal and nonverbal indicators of quality of
communication between care staff and residents in ethnoculturally and linguistically diverse long-term care settings. J Cross
Cult Gerontol 2015 Sep;30(3):285-304. [doi: 10.1007/s10823-015-9269-6] [Medline: 26260486]
4. Brownie S, Nancarrow S. Effects of person-centered care on residents and staff in aged-care facilities: a systematic review.
Clin Interv Aging 2013;8:1-10 [FREE Full text] [doi: 10.2147/CIA.S38589] [Medline: 23319855]
5. Constand MK, MacDermid JC, Dal Bello-Haas V, Law M. Scoping review of patient-centered care approaches in healthcare.
BMC Health Serv Res 2014 Jun 19;14:271 [FREE Full text] [doi: 10.1186/1472-6963-14-271] [Medline: 24947822]
6. Orange JB, Ryan EB, Meredith SD, MacLean MJ. Application of the communication enhancement model for long-term
care residents with Alzheimer s disease. Top Lang Disord 1995;15(2):20-35. [doi: 10.1097/00011363-199502000-00004]
7. Wilson R, Rochon E, Mihailidis A, Leonard C. Quantitative analysis of formal caregivers' use of communication strategies
while assisting individuals with moderate and severe Alzheimer's disease during oral care. J Commun Disord
2013;46(3):249-263. [doi: 10.1016/j.jcomdis.2013.01.004] [Medline: 23523100]
8. Wilson R, Rochon E, Mihailidis A, Leonard C. Examining success of communication strategies used by formal caregivers
assisting individuals with Alzheimer's disease during an activity of daily living. J Speech Lang Hear Res 2012
Apr;55(2):328-341. [doi: 10.1044/1092-4388(2011/10-0206)] [Medline: 22199204]
9. Alzheimer Society of Canada. 2017. Person Centred Language Guidelines URL: https://alzheimer.ca/sites/default/files/
2017-11/Person_Centred_Language_Guidelines-e.pdf [accessed 2019-12-25]
10. Bourgeault IL, Atanackovic J, Rashid A, Parpia R. Relations between immigrant care workers and older persons in home
and long-term care. Can J Aging 2010 Mar;29(1):109-118. [doi: 10.1017/S0714980809990407] [Medline: 20202269]
11. Walsh K, Shutes I. Care relationships, quality of care and migrant workers caring for older people. Aging Soc
2013;33(3):393-420. [doi: 10.1017/s0144686x11001309]
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 20http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

12. Zallman L, Finnegan KE, Himmelstein DU, Touw S, Woolhandler S. Care for America's elderly and disabled people relies
on immigrant labor. Health Aff (Millwood) 2019 Jun;38(6):919-926. [doi: 10.1377/hlthaff.2018.05514] [Medline: 31158016]
13. Stone RI. The migrant direct care workforce: an international perspective. Generations 2016;40(1):99-105 [FREE Full text]
14. Panayiotou A, Gardner A, Williams S, Zucchi E, Mascitti-Meuter M, Goh AM, et al. Language translation apps in health
care settings: expert opinion. JMIR Mhealth Uhealth 2019 Apr 9;7(4):e11316 [FREE Full text] [doi: 10.2196/11316]
[Medline: 30964446]
15. Statistics Canada. Ottawa: Statistics Canada; 2007. A Portrait of Seniors Living in Canada 2006 URL: https://www150.
statcan.gc.ca/n1/en/pub/89-519-x/89-519-x2006001-eng.pdf?st=89AKaiVw [accessed 2019-12-26]
16. Estabrooks CA, Squires JE, Carleton HL, Cummings GG, Norton PG. Who is looking after mom and dad? Unregulated
workers in Canadian long-term care homes. Can J Aging 2015 Mar;34(1):47-59 [FREE Full text] [doi:
10.1017/S0714980814000506] [Medline: 25525838]
17. Tak SH, Benefield LE, Mahoney DF. Technology for long-term care. Res Gerontol Nurs 2010 Jan;3(1):61-72 [FREE Full
text] [doi: 10.3928/19404921-20091103-01] [Medline: 20128544]
18. Loi SM, Mazur A, Huppert D, Hoy B, Swan J, Lautenschlager NT. A pilot study using 'apps' as a novel strategy for the
management of challenging behaviors seen in people living in residential care. Int Psychogeriatr 2017 Apr;29(4):637-643.
[doi: 10.1017/S1041610216002039] [Medline: 27974056]
19. Sprangers S, Dijkstra K, Romijn-Luijten A. Communication skills training in a nursing home: effects of a brief intervention
on residents and nursing aides. Clin Interv Aging 2015;10:311-319 [FREE Full text] [doi: 10.2147/CIA.S73053] [Medline:
25653513]
20. Gerrish K, Chau R, Sobowale A, Birks E. Bridging the language barrier: the use of interpreters in primary care nursing.
Health Soc Care Community 2004 Sep;12(5):407-413. [doi: 10.1111/j.1365-2524.2004.00510.x] [Medline: 15373819]
21. Czaja SJ. Long-term care services and support systems for older adults: The role of technology. Am Psychol
2016;71(4):294-301. [doi: 10.1037/a0040258] [Medline: 27159436]
22. Fried-Oken M, Mooney A, Peters B. Supporting communication for patients with neurodegenerative disease.
NeuroRehabilitation 2015;37(1):69-87 [FREE Full text] [doi: 10.3233/NRE-151241] [Medline: 26409694]
23. Fisher CA, Feigenbaum K. Harnessing technology to promote patient-centered care. Nurs Manage 2015 Jan;46(1):14-5;
quiz 22. [doi: 10.1097/01.NUMA.0000459044.24554.af] [Medline: 25536350]
24. Goh AM, Loi SM, Westphal A, Lautenschlager NT. Person-centered care and engagement via technology of residents with
dementia in aged care facilities. Int Psychogeriatr 2017 Dec;29(12):2099-2103. [doi: 10.1017/S1041610217001375]
[Medline: 28784191]
25. Øvretveit J. Digital technologies supporting person-centered integrated care - a perspective. Int J Integr Care 2017 Sep
25;17(4):6. [doi: 10.5334/ijic.3051] [Medline: 29588629]
26. Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. Pharm Ther 2014 May;39(5):356-364
[FREE Full text] [Medline: 24883008]
27. Ariel. App store Insights from Appfigures. New York; 2015 Jan 13. App Stores Growth Accelerates In 2014 URL: https:/
/blog.appfigures.com/app-stores-growth-accelerates-in-2014/ [accessed 2019-12-26]
28. Dogtiev A. Business of Apps. United Kingdom; 2019 Sep 6. App Stores List (2019) URL: https://www.businessofapps.com/
guide/app-stores-list/ [accessed 2019-12-26]
29. Armstrong N, Nugent C, Moore G, Finlay D. Using smartphones to address the needs of persons with Alzheimer’s disease.
Ann Telecommun 2010;65(9-10):485-495. [doi: 10.1007/s12243-010-0165-3]
30. Elfaki AO, Alotaibi M. The role of M-health applications in the fight against Alzheimer's: current and future directions.
mHealth 2018;4:32 [FREE Full text] [doi: 10.21037/mhealth.2018.07.03] [Medline: 30225239]
31. Yousaf K, Mehmood Z, Saba T, Rehman A, Munshi A, Alharbey R, et al. Mobile-health applications for the efficient
delivery of health care facility to people with dementia (PwD) and support to their carers: a survey. Biomed Res Int
2019;2019:7151475 [FREE Full text] [doi: 10.1155/2019/7151475] [Medline: 31032361]
32. Yousaf K, Mehmood Z, Awan IA, Saba T, Alharbey R, Qadah T, et al. A comprehensive study of mobile-health based
assistive technology for the healthcare of dementia and Alzheimer's disease (AD). Health Care Manag Sci 2019 Jun 20.
[doi: 10.1007/s10729-019-09486-0] [Medline: 31218511]
33. Brown EL, Ruggiano N, Li J, Clarke PJ, Kay ES, Hristidis V. Smartphone-based health technologies for dementia care:
opportunities, challenges, and current practices. J Appl Gerontol 2019 Jan;38(1):73-91. [doi: 10.1177/0733464817723088]
[Medline: 28774215]
34. McNaughton D, Light J. The iPad and mobile technology revolution: benefits and challenges for individuals who require
augmentative and alternative communication. Augment Altern Commun 2013 Jun;29(2):107-116. [doi:
10.3109/07434618.2013.784930] [Medline: 23705813]
35. National Institute for Health and Care Excellence (NICE). National Institute for Health and Care Excellence (NICE). 2019
Mar. Evidence Standards Framework for Digital Health Technologies URL: https://www.nice.org.uk/Media/Default/About/
what-we-do/our-programmes/evidence-standards-framework/digital-evidence-standards-framework.pdf[accessed 2019-12-26]
36. Rosser BA, Eccleston C. Smartphone applications for pain management. J Telemed Telecare 2011;17(6):308-312. [doi:
10.1258/jtt.2011.101102] [Medline: 21844177]
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 21http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

37. Nasomyont T, Wisitpongphan N. A study on the relationship between search engine optimization factors and rank on google
search result page. Adv Mat Res 2014;931-932:1462-1466. [doi: 10.4028/www.scientific.net/amr.931-932.1462]
38. Stoyanov SR, Hides L, Kavanagh DJ, Zelenko O, Tjondronegoro D, Mani M. Mobile app rating scale: a new tool for
assessing the quality of health mobile apps. JMIR Mhealth Uhealth 2015 Mar 11;3(1):e27 [FREE Full text] [doi:
10.2196/mhealth.3422] [Medline: 25760773]
39. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred Reporting Items for Systematic Reviews and
Meta-Analyses: the PRISMA statement. PLoS Med 2009 Jul 21;6(7):e1000097 [FREE Full text] [doi:
10.1371/journal.pmed.1000097] [Medline: 19621072]
40. Beukelman DR. Residential long-term care. In: Blackstone SW, Beukelman DM, Yorkston KR, editors. Patient-Provider
Communication: Roles for Speech-Language Pathologists and Other Health Care Professionals. USA: Plural Publishing;
2015:247-270.
41. Medwetsky L. Hearing Loss Association of America. 2015. Mobile Device Apps for People With Hearing Loss URL:
https://www.hearingloss.org/wp-content/uploads/HLM_SeptOct2015_Medwetsky.pdf?pdf=2015-hlm-so-lmedwetsky
[accessed 2019-12-26]
42. Hopper T, Hinton P. Hearing loss among individuals with dementia: barriers and facilitators to care. Can J Speech-Lang
Pathol Audiol 2012;36(4):302-313 [FREE Full text]
43. Guthrie DM, Davidson JG, Williams N, Campos J, Hunter K, Mick P, et al. Combined impairments in vision, hearing and
cognition are associated with greater levels of functional and communication difficulties than cognitive impairment alone:
Analysis of interRAI data for home care and long-term care recipients in Ontario. PLoS One 2018;13(2):e0192971 [FREE
Full text] [doi: 10.1371/journal.pone.0192971] [Medline: 29447253]
44. Pichora-Fuller MK. Cognitive decline and hearing health care for older adults. Am J Audiol 2015 Jun;24(2):108-111. [doi:
10.1044/2015_AJA-14-0076] [Medline: 25856721]
45. Amieva H, Ouvrard C, Giulioli C, Meillon C, Rullier L, Dartigues J. Self-reported hearing loss, hearing aids, and cognitive
decline in elderly adults: a 25-year study. J Am Geriatr Soc 2015 Oct;63(10):2099-2104. [doi: 10.1111/jgs.13649] [Medline:
26480972]
46. McGilton KS, Höbler F, Campos J, Dupuis K, Labreche T, Guthrie DM, et al. Hearing and vision screening tools for
long-term care residents with dementia: protocol for a scoping review. BMJ Open 2016 Jul 26;6(7):e011945 [FREE Full
text] [doi: 10.1136/bmjopen-2016-011945] [Medline: 27466242]
47. Small J, Wilson R, Milhailidis A, Cochrane D. Promoting hearing and communication health in long-term residential care
through the use of communication apps. Can Acoust 2016;44(3) [FREE Full text] [doi: 10.1002/9781119264927.index]
48. Reis A, Pedrosa A, Dourado M, Reis C. Information and communication technologies in long-term and palliative care.
Procedia Technol 2013;9:1303-1312. [doi: 10.1016/j.protcy.2013.12.146]
49. Martínez-Alcalá CI, Pliego-Pastrana P, Rosales-Lagarde A, Lopez-Noguerola JS, Molina-Trinidad EM. Information and
communication technologies in the care of the elderly: systematic review of applications aimed at patients with dementia
and caregivers. JMIR Rehabil Assist Technol 2016 May 2;3(1):e6 [FREE Full text] [doi: 10.2196/rehab.5226] [Medline:
28582258]
50. Lancioni GE, Singh NN, O'Reilly MF, Sigafoos J, Renna C, Pinto K, et al. Persons with moderate Alzheimer's disease use
simple technology aids to manage daily activities and leisure occupation. Res Dev Disabil 2014 Sep;35(9):2117-2128. [doi:
10.1016/j.ridd.2014.05.002] [Medline: 24881006]
51. Lancioni GE, Singh NN, O'Reilly MF, Sigafoos J, D'Amico F, Sasanelli G, et al. Persons with Alzheimer's disease engage
in leisure and mild physical activity with the support of technology-aided programs. Res Dev Disabil 2015 Feb;37:55-63.
[doi: 10.1016/j.ridd.2014.11.004] [Medline: 25460220]
Abbreviations
AAC: augmentative and alternative communication
ADL: activities of daily living
ADRD: Alzheimer disease and related dementias
cApp: communication app
iOS: iPhone Operating System
LTRC: long-term residential care
MCT: mobile communication technology
PCC: person-centered communication
SLP: speech-language pathologist
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 22http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX

Edited by J Wang; submitted 21.11.19; peer-reviewed by B Sheng, K Meyer, B Davis; comments to author 20.12.19; revised version
received 02.01.20; accepted 02.01.20; published 08.04.20
Please cite as:
Wilson R, Cochrane D, Mihailidis A, Small J
Mobile Apps to Support Caregiver-Resident Communication in Long-Term Care: Systematic Search and Content Analysis
JMIR Aging 2020;3(1):e17136
URL: http://aging.jmir.org/2020/1/e17136/
doi: 10.2196/17136
PMID: 32267236
©Rozanne Wilson, Diana Cochrane, Alex Mihailidis, Jeff Small. Originally published in JMIR Aging (http://aging.jmir.org),
08.04.2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium,
provided the original work, first published in JMIR Aging, is properly cited. The complete bibliographic information, a link to
the original publication on http://aging.jmir.org, as well as this copyright and license information must be included.
JMIR Aging 2020 | vol. 3 | iss. 1 | e17136 | p. 23http://aging.jmir.org/2020/1/e17136/
(page number not for citation purposes)
Wilson et alJMIR AGING
XSL
•
FO
RenderX
