
VOL 63: APRIL • AVRIL 2017
|
Canadian Family Physician • Le Médecin de famille canadien
295
Praxis
An efcient tool for the primary
care management of menopause
Susan Goldstein MD CCFP FCFP NCMP
T
he Canadian population is aging. In 2014, women
aged 50 to 54 years comprised the largest age cohort
of women in Canada,
1
an age at which most women
begin the menopause transition. This might be accom-
panied by vasomotor symptoms (VMS), genitouri-
nary syndrome of menopause (GSM), mood and sleep
changes, joint pain, and more.
2
After the early termination of the Women’s Health
Initiative in 2002, menopausal hormone therapy (MHT)
became highly controversial because of reported
increases in the risk of breast cancer and cardiovascular
disease.
3
In response, interest in nonhormonal options
grew and many have been evaluated (eg, antidepressants,
gabapentin, pregabalin, clonidine, phytoestrogens). While
they were effective for mild VMS, these medications are
not particularly effective for moderate to severe VMS or
for some of the other menopause-related concerns.
4,5
New guidelines
Menopausal hormone therapy remains the most effec-
tive treatment of VMS, and is also indicated for GSM
(previously called vulvovaginal atrophy) and bone pro-
tection.
4,6,7
Recently, the Women’s Health Initiative data
have been reevaluated to better guide physicians in
patient selection, with risks being reevaluated and strat-
ified by age and time since menopause.
8
New guide-
lines have been created, with the consensus that MHT
is safest for those younger than 60 years and within
10 years of menopause
4,6
and might be continued for
some women after age 65.
9
This is clinically relevant, as
new evidence is emerging indicating that many women
continue to experience substantial symptoms well into
their 60s, with a mean duration of VMS of more than
7 years and extending beyond 11 years for many.
10
With
no fixed duration of treatment, the guidelines now state
that MHT should be individualized to account for each
patient’s unique risk-benefit profile.
4,6
This article is eligible for Mainpro+ certied
Self-Learning credits. To earn credits, go to
www.cfp.ca and click on the Mainpro+ link.
This article has been peer reviewed.
Can Fam Physician 2017;63:295-8
La traduction en français de cet article se trouve à
www.cfp.ca dans la table des matières du numéro
d’avril 2017 à la page e219.
Many primary care clinicians have had little experi-
ence treating menopausal patients. New guidelines and
position statements, including those from the Society of
Obstetricians and Gynaecologists of Canada,
4
the North
American Menopause Society,
7
and the International
Menopause Society,
6
help support health care providers
in caring for menopausal women. These statements by
leading organizations in mature women’s health include
recommendations that certain questions be asked of all
perimenopausal women.
4,6,7
However, existing meno-
pausal questionnaires, such as the Menopause-Specific
Quality of Life Questionnaire and Greene Climacteric
Scale, are lengthy and might not be ideal for use in the
primary care setting.
With the needs of busy primary care physicians in
mind, I have developed a quick menopausal screen-
ing questionnaire called the Menopause Quick 6 (MQ6)
(Figure 1).
4,6
This 6-question scale assesses menopausal
symptoms for which there are evidence-based treatment
options while providing a patient-centred assessment
to guide treatment choices. This short questionnaire,
written in lay language, can be used during any clinical
encounter, including a periodic health examination.
These 6 questions were selected because they elicit
helpful information that can guide management deci-
2,4,6,10-12
sions, as described in Table 1.
Putting the MQ6 into practice
The MQ6 was designed to be a quick and efficient tool
for primary care practice. The information elicited from
the 6 questions can guide evidence-based treatment
decisions, as set out in the algorithm in Figure 2.
5
As the algorithm specifies, when hormone therapy
is indicated and there are no contraindications to MHT,
then a transdermal preparation, which avoids first-pass
hepatic metabolism, is recommended for women with
comorbidities that increase cardiovascular risk, includ-
ing risk of venous thromboembolism or stroke (based
on observational data).
11
As the progestogen in the MHT regimen provides
endometrial protection, patients who have undergone
a hysterectomy require only estrogen therapy. When
endometrial protection is required, the use of either
estrogen-progestogen therapy or a tissue-selective
estrogen complex is recommended.
4
A tissue-selective
estrogen complex recently approved for use in Canada
combines conjugated equine estrogen with a selective

296
Canadian Family Physician
•
Le Médecin de famille canadien
|
VOL 63: APRIL • AVRIL 2017
Praxis
estrogen receptor modulator (bazedoxifene), the latter
component providing endometrial protection while
eliminating the need for a progestogen.
In the first year after menopause begins, women
will often bleed when taking a continuous MHT regi-
men, so a cyclic regimen is preferred.
11
Cyclic regimens
usually include a steady dose of an estrogen for days
1 to 25 or 1 to 31 of the month, accompanied by a
progestogen for 12 to 14 days of the month, resulting in
withdrawal bleeding. Continuous regimens use steady
daily doses of an estrogen and progestogen.
13
Of note, we are now treating with lower-dose regi-
mens of MHT, which do not always provide sufficient
treatment of the local symptoms of GSM. For adequate
treatment of local symptoms, the addition of vaginal
estrogen therapy should be considered.
Figure 1. The Menopause Quick 6 questionnaire: If a patient answers yes to any of questions 1 to 4, she might be
a candidate for treatment, and further exploration and assessment is warranted. The Society of Obstetricians and
Gynaecologists of Canada and International Menopause Society guidelines recommend that questions 2 to 6 be
asked of all perimenopausal women.
4,6
Any changes
in your
periods?
Are you
having any
hot ˜ashes?
Any vaginal
dryness or
pain, or sexual
concerns?
Any bladder
How is your
How is
issues or
sleep?
your mood?
incontinence?
Table 1. How to use the information elicited by questions that comprise the Menopause Quick 6
QUESTION INTERPRETATION
Q1: Any changes in your periods? Menstrual irregularities signal imminent menopause. A recent study found that when VMS start
before the cessation of menses, they can be expected to last longer (median 11.8 y) than VMS
that start after the LMP (3.4 y).
10
Further, when prescribing MHT for women who are still cycling
irregularly or within 1 y of their LMP, a cyclic hormone regimen should be used.
11
If the LMP was
more than 1 y ago, continuous regimens can be offered. For all women with cessation of menses
younger than 45 y, MHT is recommended
Q2: Are you having any hot Up to 80% of menopausal women experience VMS. When these are mild, many lifestyle and
ashes? nonhormonal interventions can be effective. Moderate to severe VMS are treated most
effectively by hormone therapy
4,6
Q3: Any vaginal dryness or pain, The term vulvovaginal atrophy has been replaced by genitourinary syndrome of menopause,
or any sexual concerns? reecting the changes to the vulva, vagina, and urinary tract and to sexual functioning owing
to the menopausal drop in estrogen. Many women are reluctant to talk about their vaginal or
Q4: Any bladder issues or
sexual concerns, bladder issues, or incontinence, yet these can have a substantial negative effect
incontinence?
on quality of life. We have effective treatments for these symptoms, so we must ask
Q5: How is your sleep? Sleep disturbances are common during menopause and are most often attributed to hot
ashes.
2
Poor sleep can exacerbate mood and anxiety issues and contribute to cognitive
complaints and even weight gain
Q6: How is your mood? Menopause is a high-risk time for rst-episode or recurrent depression.
12
In addition, anxiety
and irritability peak during perimenopause. Both SSRIs and SNRIs have been shown to be
effective for these mood disorders while having a benecial effect on VMS. Women who remain
symptomatic despite these medications might benet from hormonal augmentation
LMP—last menstrual period, MHT—menopausal hormone therapy, SNRI—serotonin-norepinephrine reuptake inhibitor, SSRI—selective serotonin reuptake
inhibitor, VMS—vasomotor symptoms.
VOL 63: APRIL • AVRIL 2017
|
Canadian Family Physician • Le Médecin de famille canadien
297
Praxis
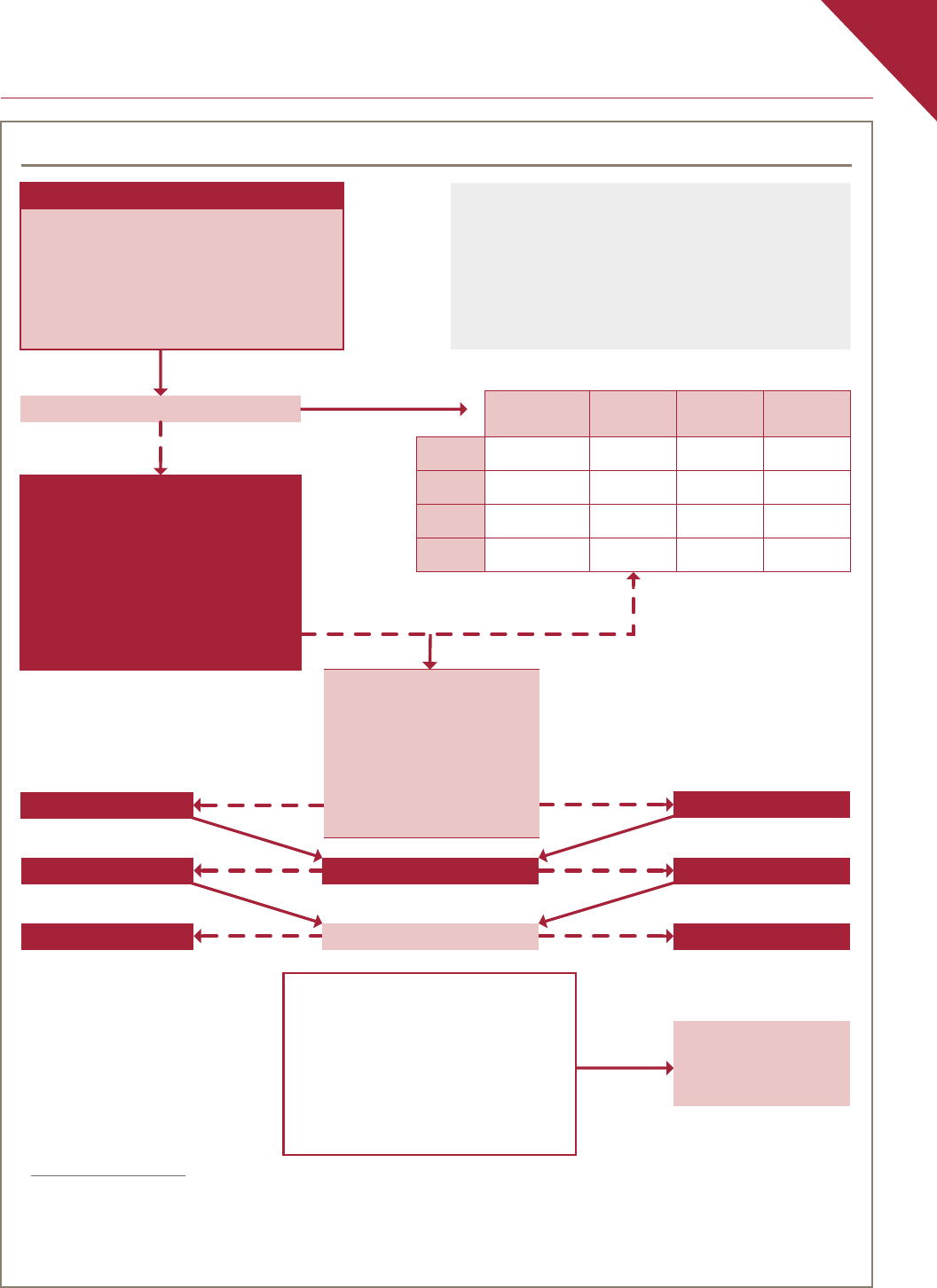
Figure 2. Evidence-based algorithm for management of menopausal symptoms
• Active thromboembolic diagnosis
• Acute CVD
YES
• Recent cerebrovascular accident
• Pregnancy
NO
Any estrogen
Td estrogen preferred
Comorbidities?
• Diabetes mellitus
• Hypertension
• Smoking
• Obesity
• High lipid levels or CVD risk
• Gallstones
YES
NO
NO
NO
Hysterectomy?
YES
YES
EPT or TSEC
ET
Cyclic regimen
LMP > 1 y ago? Continuous regimen
GSM symptoms?
• Vaginal dryness, pain or dyspareunia,
or urinary symptoms
Consider adding
AND
additional vaginal ET
Lower dose of estrogen to be prescribed:
(cream, tablet, or ring)
˜ 0.625 mg of oral CEE, 1.0 mg of
oral estradiol, or 50 µg of Td estradiol
CBT—cognitive-behavioural therapy, CEE—conjugated equine estrogen, CVD—cardiovascular disease, EPT—estrogen-progestogen therapy, ET—estrogen therapy,
GSM—genitourinary syndrome of menopause, LMP—last menstrual period, MHT—menopausal hormone therapy, MQ6—Menopause Quick 6, OAB—overactive
bladder, SNRI—serotonin-norepinephrine reuptake inhibitor, SSRI—selective serotonin reuptake inhibitor, Td—transdermal, TSEC—tissue-selective estrogen
complex, VMS—vasomotor symptoms.
*In this table, + indicates some evidence of efÿcacy, ++ indicates good evidence of efÿcacy, +++ indicates strong evidence of efÿcacy, and +/- suggests the
treatment might improve or worsen symptoms. Data from the North American Menopause Society.
5
MQ6
1. Menstrual pattern
2. VMS
3. Vaginal pain or dryness, or sexual concerns
4. Urinary incontinence or OAB
5. Sleep issues
6. Mood issues
NO
MHT indicated?
YES
Contraindications to MHT
• Unexplained vaginal bleeding
• Known or suspected breast cancer
• Acute liver disease
The MQ6 was developed as a brief screening tool to
identify the presence of menopause-related symptoms that
are amenable to therapy and for which there are approved
treatments. The MQ6 can be used either as a questionnaire
by patients while waiting for their appointments or as a
verbal screening tool by health care practitioners during a
medical encounter or periodic health examination
Nonhormonal management of symptoms
Gabapentin or
pregabalin
SSRI or
SNRI
Clonidine
CBT or
hypnosis
VMS* ++ ++ + +
GSM
Sleep
+++ +/-
Mood
+++

298
Canadian Family Physician
•
Le Médecin de famille canadien
|
VOL 63: APRIL • AVRIL 2 017
Praxis
Conclusion
Primary care clinicians are increasingly using measurement-
based care and integrating it into their electronic med-
ical record systems. The MQ6 can help fill a gap for
measurement-based care in mature women’s health. It
takes about 2 minutes to use the MQ6 questionnaire
with a perimenopausal patient, making it an efficient tool
for busy primary care clinicians.
Using the MQ6 ensures that clinicians are asking the
right questions in a standardized way. The accompa-
nying algorithm, guided by the answers to the MQ6, is
based on the latest evidence-based guidelines and can
facilitate clinical decisions in an area that has a con-
troversial and sometimes confusing history. From the
patient perspective, using these tools can help patients
engage to discuss sensitive issues and it reassures them
they are being cared for in a holistic manner.
Dr Goldstein is a family physician practising in Toronto, Ont, and Assistant
Professor in the Department of Family and Community Medicine at the
University of Toronto.
Acknowledgment
I thank Dr Wendy Wolfman, Mr Mike Hill, and Ms Christina Clark for their
contributions to this article.
Competing interests
Dr Goldstein has received honoraria for advisory board participation and
consultant fees from Pfizer and Merck.
References
1. Statistics Canada. Table 051-0001. Estimates of population, by age group and sex
for July 1, Canada, provinces and territories. Ottawa, ON: Statistics Canada; 2016.
Available from: www5.statcan.gc.ca/cansim/a26?lang=eng&retrLang=eng&id
=0510001&&pattern=&stByVal=1&p1=1&p2=31&tabMode=dataTable&csid=.
Accessed 2017 Feb 23.
2. Dennerstein L, Dudley EC, Hopper JL, Guthrie JR, Burger HG. A prospective
population-based study of menopausal symptoms. Obstet Gynecol 2000;96(3):351-8.
3. Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML,
et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal
women: principal results from the Women’s Health Initiative randomized controlled
trial. JAMA 2002;288(3):321-33.
4. Reid R, Abramson BL, Blake J, Desindes S, Dodin S, Johnston S, et al. Managing
menopause. J Obstet Gynaecol Can 2014;36(9):830-8.
5. North American Menopause Society. Nonhormonal management of menopause-
associated vasomotor symptoms: 2015 position statement of the North American
Menopause Society. Menopause 2015;22(11):1155-72.
6. Baber RJ, Panay N, Fenton A; IMS Writing Group. 2016 IMS recommenda-
tions on women’s midlife health and menopause hormone therapy. Climacteric
2016;19(2):109-50. Epub 2016 Feb 12.
7. Shifren JL, Gass ML; NAMS Recommendations for Clinical Care of Midlife Women
Working Group. The North American Menopause Society recommendations for
clinical care of midlife women. Menopause 2014;21(10):1038-62.
8. Manson JE, Chlebowski RT, Stefanick ML, Aragaki AK, Rossouw JE, Prentice RL,
et al. Menopausal hormone therapy and health outcomes during the intervention
and extended poststopping phases of the Women’s Health Initiative randomized
trials. JAMA 2013;310(13):1353-68.
9. North American Menopause Society. The North American Menopause Society
statement on continuing use of systemic hormone therapy after age 65. Menopause
2015;22(7):693.
10. Avis NE, Crawford SL, Greendale G, Bromberger JT, Everson-Rose SA, Gold EB,
et al. Duration of menopausal vasomotor symptoms over the menopause transition.
JAMA Intern Med 2015;175(4):531-9.
11. Panay N, Hamoda H, Arya R, Savvas M; British Menopause Society and Women’s
Health Concern. The 2013 British Menopause Society and Women’s Health Concern
recommendations on hormone replacement therapy. Menopause Int 2013;19(2):
59-68. Epub 2013 May 23.
12. Soares CN. Can depression be a menopause-associated risk? BMC Med 2010;8:79.
13. Brown TER. Practical issues in hormone therapy management. Can Pharm J
2010;143(Suppl 2):S12-3.e1.
