
School Employees
Benefits Board (SEBB)
Program
Standard PPO Plan
4018486
INTRODUCTION
Premera Blue Cross is an Independent Licensee of the Blue Cross Blue Shield Association. The benefits,
limitations, exclusions and other coverage provisions in this booklet are subject to the terms of our contract with
the Group. This booklet is a part of that contract, which is on file in the Group's office and at Premera Blue Cross.
This booklet replaces any other benefit booklet you may have received. The Group has delegated authority to
Premera Blue Cross to use its expertise and judgment as part of the routine operation of the plan to reasonably
apply the terms of the contract for making decisions as they apply to benefits and claims situations. This does not
prevent you from exercising rights you may have under applicable state or federal law to appeal, have
independent review of our judgment and decisions, or bring a civil lawsuit challenging to any eligibility or claims
determinations under the contract, including our exercise of our judgment and expertise.
If any provision of this Plan is superseded by state or federal law, the Plan will comply with the applicable
law as it relates to those provisions.
Group Name:
Washington State Healthcare Authority For The School Employees Benefits Board
Program
Effective Date:
January 1, 2024
Group Number:
4018486
Plan:
Standard PPO
Certificate Form Number:
40184860124B
40184860124B

Discrimination is Against the Law
Premera Blue Cross (Premera) complies with applicable Federal civil rights laws and does not discriminate on the basis of race,
color, national origin, age, disability, or sex. Premera does not exclude people or treat them differently because of race, c olor,
national origin, age, disability, sex, gender identity, or sexual orientation. Premera provides free aids and services to people with
disabilities to communicate effectively with us, such as qualified sign language interpreters and written information i n other
formats (large print, audio, accessible electronic formats, other formats). Premera provides free language services to people
whose primary language is not English, such as qualified interpreters and information written in other languages. If you need
these services, contact the Civil Rights Coordinator. If you believe that Premera has failed to provide these services or
discriminated in another way on the basis of race, color, national origin, age, disability, or sex, you can file a grievance with: Civil
Rights Coordinator ─ Complaints and Appeals, PO Box 91102, Seattle, WA 98111, Toll free: 855-332-4535, Fax: 425-918-5592, TRS:
711, Email AppealsDepartmentInquiries@Premera.com. You can file a grievance in person or by mail, fax, or email. If you need help
filing a grievance, the Civil Rights Coordinator is available to help you. You can also file a civil rights complaint with the U.S.
Department of Health and Human Services, Office for Civil Rights, electronically through the Office for Civil Rights Complaint
Portal, available at https://ocrportal.hhs.gov/ocr/portal/lobby.jsf, or by mail or phone at: U.S. Department of Health and Human
Services, 200 Independence Ave SW, Room 509F, HHH Building, Washington, D.C. 20201, 1-800-368-1019, 800-537-7697 (TDD).
Complaint forms are available at http://www.hhs.gov/ocr/office/file/index.html.
Language Assistance
ATENCIÓN: si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al 800-807-7310 (TRS:
711).
注意:如果您使用繁體中文,您可以免費獲得語言援助服務。請致電
800-807-7310
(
TRS
:
711
)。
CHÚ Ý: N
ế
u b
ạ
n nói Ti
ế
ng Vi
ệ
t, có các d
ị
ch v
ụ
h
ỗ
tr
ợ
ngôn ng
ữ
mi
ễ
n phí dành cho b
ạ
n. G
ọ
i s
ố
800-807-7310 (TRS: 711).
주의: 한국어를 사용하시는 경우, 언어 지원 서비스를 무료로 이용하실 수 있습니다.
800-807-
7310 (TRS: 711)
번으로 전화해 주십시오.
ВНИМАНИЕ: Если вы говорите на русском языке, то вам доступны бесплатные услуги перевода. Звоните 800-807-7310
(служба коммутируемых сообщений: 711).
PAUNAWA: Kung nagsasalita ka ng Tagalog, maaari kang gumamit ng mga serbisyo ng tulong sa wika nang walang bayad.
Tumawag sa 800-807-7310 (TRS: 711).
УВАГА! Якщо ви розмовляєте українською мовою, ви можете звернутися до безкоштовної служби
мовної підтримки. Телефонуйте за номером 800-807-7310 (служба комутованих повідомлень:
711).
,
800-807-7310 (TRS: 711)
注意事項:日本語を話される場合、無料の言語支援をご利用いただけます。
800-807-7310
(
TRS:711
)
まで、お電話にてご連絡ください。
ማስታወሻ: የሚናገሩት ቋንቋ ኣማርኛ ከሆነ የትርጉም እርዳታ ድርጅቶች፣ በነጻ ሊያግዝዎት ተዘጋጀተዋል ወደ ሚከተለው ቁጥር ይደውሉ
800-807-7310
(በስልክ ማገናኛ አገልግሎት:
711
).
XIYYEEFFANNAA: Afaan dubbattu Oroomiffa, tajaajila gargaarsa afaanii, kanfaltiidhaan ala, ni argama. Bilbilaa 800-807-7310 (TRS:
711).
7310
807
800
711
800-807-
7310 (TRS: 711)
ACHTUNG: Wenn Sie Deutsch sprechen, stehen Ihnen kostenlos sprachliche Hilfsdienstleistungen zur Verfügung.
Rufnummer: 800-807-7310 (TRS: 711).

:
,
,
, .
800-807-
7310 (TRS: 711).
ATANSYON: Si w pale Kreyòl Ayisyen, gen sèvis èd pou lang ki disponib gratis pou ou. Rele 800-807-7310 (TRS: 711).
ATTENTION: Si vous parlez français, des services d'aide linguistique vous sont proposés gratuitement. Appelez le 800-807-7310 (SRT :
711).
UWAGA: Jeżeli mówisz po polsku, możesz skorzystać z bezpłatnej pomocy językowej. Zadzwoń pod numer 800-807-7310 (TRS:
711).
ATENÇÃO: Se fala português, encontram-se disponíveis serviços linguísticos, grátis. Ligue para 800-807-7310 (TRS: 711).
ATTENZIONE: In caso la lingua parlata sia l'italiano, sono disponibili servizi di assistenza linguistica gratuiti. Chiamare il numero
800-807-7310 (TRS: 711).
هجوت
7310 (TRS: 711)-807-800
HOW TO USE THIS BOOKLET
This booklet will help you get the most out of your benefits. Every section contains important information, but the
ones below may be particularly useful:
• Summary Of Your Costs – A quick overview of what the plan covers and your costs
• How Providers Affect Your Costs — how using in-network providers will cut your costs
• Important Plan Information – Explains the allowed amount and gives you details on the deductible, copays,
coinsurance, and the out-of-pocket maximum.
• Covered Services – details about what's covered
• Prior Authorization – Describes the plan's prior authorization and emergency admission notification
requirements.
• Exclusions — services that are either limited or not covered under this plan
• Medical Plan Eligibility And Enrollment – eligibility requirements for this plan
• How Do I File A Claim? — step-by-step instructions for claims submissions
• Complaints And Appeals — processes to follow if you want to file a complaint or an appeal
• Definitions — terms that have specific meanings under this plan. Example: “You” and “your” refer to
members under this plan. “We,” “us” and “our” refer to Premera Blue Cross in Washington and Premera Blue
Cross Blue Shield of Alaska in Alaska.
FOR MORE INFORMATION
You'll find our contact information on the back cover of this booklet. Please call or write customer service for help
with:
• Questions about benefits or claims
• Questions or complaints about care you receive
• Changes of address or other personal information
You can also get benefit, eligibility and claim information through our Interactive Voice Response system when
you call.
Online information about your plan is at your fingertips whenever you need it
You can use our website to:
• Locate a health care provider near you
• Get details about the types of expenses you're responsible for and this plan's benefit maximums
• Check the status of your claims
• Visit our health information resource to learn about diseases, medications, and more
TABLE OF CONTENTS
CONTACT US........................................................... (SEE BACK COVER OF THIS BOOKLET)
SUMMARY OF YOUR COSTS ............................................................................................................ 1
HOW PROVIDERS AFFECT YOUR COSTS ...................................................................................... 13
In-Network Providers .................................................................................................................. 13
Continuity of Care ....................................................................................................................... 13
Non-Participating ........................................................................................................................ 14
Balance Billing Protection ............................................................................................................ 15
Benefits For Out-Of-Network Or Non-Contracted Providers ........................................................... 15
IMPORTANT PLAN INFORMATION ................................................................................................. 15
Copayments (Copays) ................................................................................................................ 16
Split Copay For Office Visits ........................................................................................................ 16
Calendar Year Deductible ........................................................................................................... 16
Coinsurance ............................................................................................................................... 17
Out-Of-Pocket Maximum ............................................................................................................. 17
Allowed Amount.......................................................................................................................... 18
COVERED SERVICES ..................................................................................................................... 18
Acupuncture ......................................................................................................................... 19
Allergy Testing and Treatment ............................................................................................... 19
Ambulance ........................................................................................................................... 19
Blood Products And Services ................................................................................................ 20
Cellular Immunotherapy And Gene Therapy ........................................................................... 20
Chemotherapy And Radiation Therapy................................................................................... 20
Clinical Trials ........................................................................................................................ 20
Dental Injury and Facility Anesthesia...................................................................................... 21
Diagnostic X-Ray, Lab And Imaging ....................................................................................... 21
Dialysis ................................................................................................................................ 22
Emergency Room ................................................................................................................. 23
Foot Care ............................................................................................................................. 23
Gender Affirming Care .......................................................................................................... 23
Hearing Care ........................................................................................................................ 23
Hearing Hardware................................................................................................................. 24
Home Health Care ................................................................................................................ 24
Home Medical Equipment (HME), Orthotics, Prosthetics And Supplies ..................................... 25
Hospice Care ....................................................................................................................... 26
Hospital................................................................................................................................ 27
Infusion Therapy ................................................................................................................... 28
Massage Therapy ................................................................................................................. 28
Mastectomy and Breast Reconstruction ................................................................................. 28
Maternity Care ...................................................................................................................... 28
Medical Foods ...................................................................................................................... 29
Medical Transportation.......................................................................................................... 29
Medical Transportation – State Restricted Care ...................................................................... 30
Mental Health Care ............................................................................................................... 31
Neurodevelopmental Therapy (Habilitation) ............................................................................ 33
Newborn Care ...................................................................................................................... 33
Orthognathic Surgery (Jaw Augmentation Or Reduction) ......................................................... 34
Prescription Drug .................................................................................................................. 34
Preventive Care .................................................................................................................... 39
Professional Visits And Services ............................................................................................ 41
Psychological and Neuropsychological Testing ....................................................................... 42
Rehabilitation Therapy .......................................................................................................... 42
Skilled Nursing Facility Care .................................................................................................. 43
Spinal and Other Manipulations ............................................................................................. 43
Substance Use Disorder ....................................................................................................... 43
Surgery ................................................................................................................................ 44
Surgical Center Care – Outpatient ......................................................................................... 44
Temporomandibular Joint Disorders (TMJ) Care ..................................................................... 44
Therapeutic Injections ........................................................................................................... 45
Transplants .......................................................................................................................... 45
Urgent Care ......................................................................................................................... 46
Virtual Care .......................................................................................................................... 47
Weight Management ............................................................................................................. 47
WHAT DO I DO IF I'M OUTSIDE WASHINGTON AND ALASKA? ...................................................... 48
Out-Of-Area Care ....................................................................................................................... 48
CARE MANAGEMENT ..................................................................................................................... 50
Prior-Authorization ...................................................................................................................... 50
How Prior-Authorization Works .............................................................................................. 50
Prior-Authorization for Benefit Coverage ................................................................................ 50
Exceptions To Prior Authorization For Benefit Coverage.......................................................... 51
Prior-Authorization For Out-Of-Network Provider Coverage ..................................................... 51
Exceptions to Prior-Authorization For Out-Of-Network Providers .............................................. 51
Clinical Review ........................................................................................................................... 52
Personal Health Support Programs .............................................................................................. 52
Chronic Condition Management................................................................................................... 52
EXCLUSIONS .................................................................................................................................. 53
WHAT IF I HAVE OTHER COVERAGE? ........................................................................................... 56
Coordinating Benefits With Other Health Care Plans ..................................................................... 56
COB Definitions .................................................................................................................... 57
Primary And Secondary Rules ............................................................................................... 57
COB's Effect On Benefits ...................................................................................................... 58
Subrogation And Reimbursement ................................................................................................ 59
Uninsured And Underinsured Motorist/Personal Injury Protection Coverage ................................... 60
HOW DO I FILE A CLAIM?............................................................................................................... 74
Timely Filing ............................................................................................................................... 75
COMPLAINTS AND APPEALS......................................................................................................... 75
What You Can Appeal................................................................................................................. 76
Appeal Levels............................................................................................................................. 76
How To Submit An Appeal........................................................................................................... 76
If We Need More Time ............................................................................................................... 78
How To Ask For An External Review............................................................................................ 78
Additional Information About Your Coverage ................................................................................ 79
OTHER INFORMATION ABOUT THIS PLAN .................................................................................... 80
Conformity With The Law ............................................................................................................ 80
Entire Contract ........................................................................................................................... 80
Evidence Of Medical Necessity.................................................................................................... 80
The Group And You .................................................................................................................... 80
Healthcare Providers - Independent Contractors ........................................................................... 80
Intentionally False Or Misleading Statements ............................................................................... 80
Member Cooperation .................................................................................................................. 81
Newborn’s and Mother’s Health Protection Act ............................................................................. 81
Notice Of Information Use And Disclosure .................................................................................... 81
Notice Of Other Coverage ........................................................................................................... 81
Notices....................................................................................................................................... 81
Right Of Recovery ...................................................................................................................... 82
Right To And Payment Of Benefits............................................................................................... 82
Venue ........................................................................................................................................ 82
Women's Health and Cancer Rights Act of 1998 ........................................................................... 82
Workers’ Compensation Insurance .............................................................................................. 82
DEFINITIONS................................................................................................................................... 83
1 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
SUMMARY OF YOUR COSTS
This section shows a summary table of the care covered by your plan. It also explains the amounts you pay.
This section does not go into all the details of your coverage. See Covered Services to learn more.
First, here is a quick look at how this plan works. Your costs are subject to all of the following.
• Networks. To help control the cost of your care, this plan uses Premera's Heritage Prime network in
Washington. You may be able to save money if you use an in-network provider. For more network details, see
How Providers Affect Your Costs.
• Allowed amount. This is the most this plan allows for a covered service. See Important Plan Information for
details. For some covered services, you have to pay part of the allowed amount. This is called your cost
share. This plan's cost shares are explained below. You will find the amounts in the summary table.
• Copays. These are set dollar amounts you pay at the time you get some services. If the amount billed is less
than the copay, you pay only the amount billed. Copays apply to the out-of-pocket maximum unless stated
otherwise in the summary table. The deductible does not apply to most services that require a copay. Any
exceptions are shown in the table.
This plan has a different copay for office visits with specialists than with non-specialists. To find out which
providers get which copays, see How Providers Affect Your Costs.
In-Network Providers
Non-specialist professional visit copay
$25
Specialist professional visit copay
$50
• Deductible. The total allowed amount you pay in each year before this plan starts to make payments for your
covered healthcare costs. You pay down each deductible separately with each claim that applies to it.
In-Network Providers
Out-of-Network Providers
Individual deductible
$1,250
$2,000
Family deductible (not shown in the
summary table)
$3,125
$5,000
• Coinsurance. For some healthcare, you pay a percentage of the allowed amount, and the plan pays the rest.
This booklet calls your percentage “coinsurance.” You pay less coinsurance for many benefits when you use
an in-network provider. Your coinsurance is shown in the summary table.
In-Network Providers
Out-of-Network Providers
Coinsurance
20%
50%
• Out-of-pocket maximum (not shown in the summary table). This is the most you pay each calendar year for
any deductibles, copays and coinsurance. Not all the amounts you have to pay count toward the out-of-pocket
maximum. See Important Plan Information for details.
In-Network Providers
Out-of-Network Providers
Individual out-of-pocket maximum
$5,000
None
Family out-of-pocket maximum
$10,000
None
• Prior Authorization. Some services must be approved in advance before you get them, in order to be covered.
See Prior Authorization for details about the types of services and time limits. Some services have special
rules.
This plan complies with state and federal regulations about diabetes medical treatment coverage. See the
Preventive Care, Prescription Drug, Home Medical Equipment (HME), Orthotics, Prosthetics And Supplies,
and Foot Care benefits.
2 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
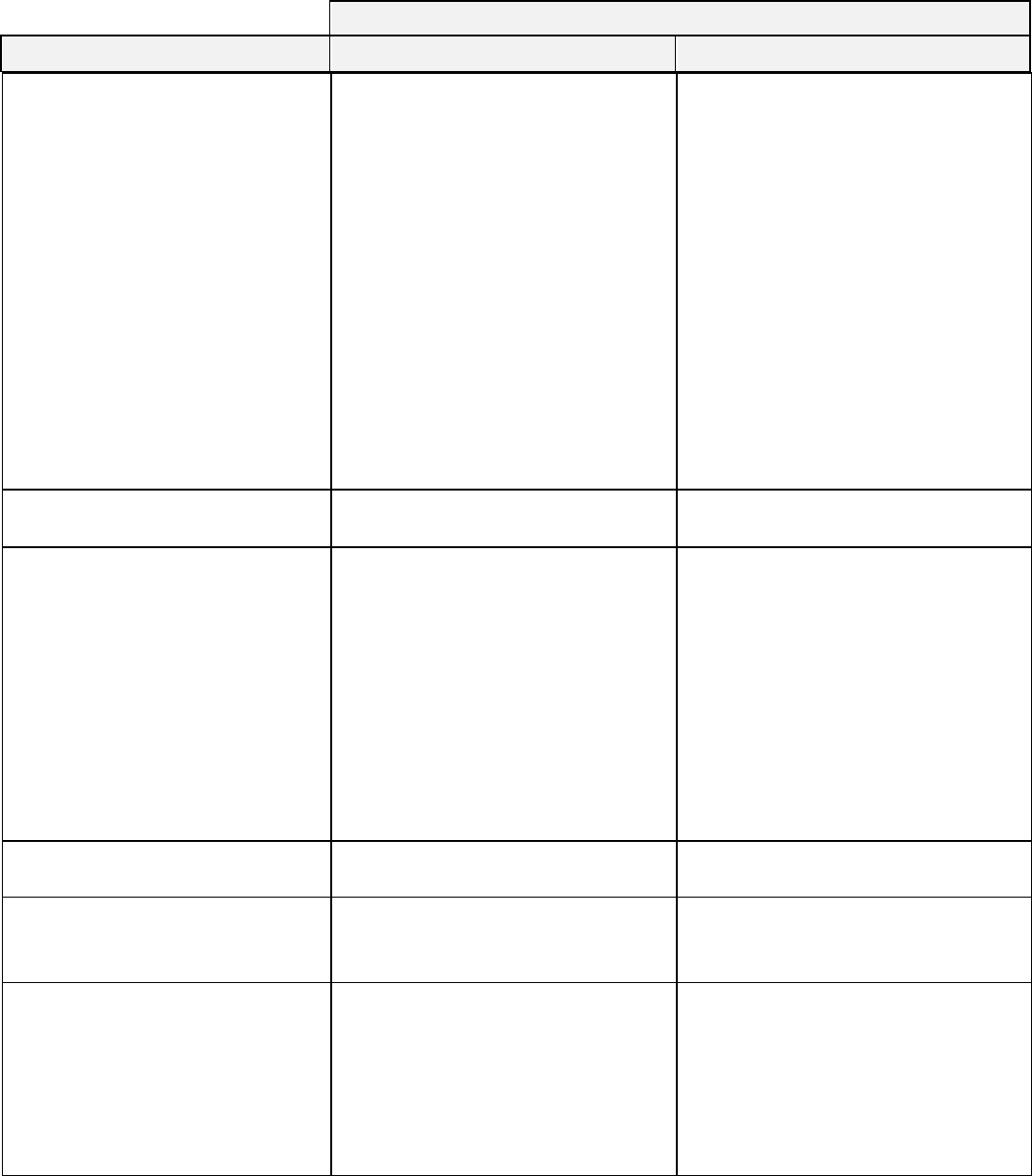
SUMMARY TABLE
The summary table below shows plan limits and what you pay (your cost shares) for covered services.
Facility in the table below means hospitals or other medical institutions. Professional means doctors, nurses,
and other people who give you your care. When you see the term “No charge” in the table below, this means
that you do not have to pay any deductible, copay or coinsurance for covered services and the provider can not
bill you any amount. No cost shares means that although you do not pay any deductible, copay or coinsurance
for covered services, the provider can bill you for amounts over the allowed amount. A non-participating provider
can bill you for amounts over the allowed amount except for emergency services, covered air ambulance
services, or as prohibited by law.

YOUR SHARE OF THE ALLOWED AMOUNT
BENEFIT
IN-NETWORK PROVIDERS
OUT-OF-NETWORK PROVIDERS
3 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Acupuncture
calendar year visit limit: 24 visits
Substance use disorder-related: no
limit
$25 copay per visit, deductible waived
Deductible, then 50% coinsurance
Allergy Testing And Treatment
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Ambulance
Deductible, then 20% coinsurance
Deductible, then 20% coinsurance
Blood Products and Services
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Cellular Immunotherapy And
Gene Therapy
Covered as any other in-network
service
Covered as any other out-of-network
service
Chemotherapy and Radiation
Therapy
Professional and facility services
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Clinical Trials
Covers routine patient care during
the trial
You may have additional costs for
other services such as x-rays, lab,
prescription drugs, and hospital
facility charges. See those covered
services for details.
Covered as any other service
Covered as any other service
Dental Injury and Facility
Anesthesia
• Dental Anesthesia (up to age 19
when medically necessary)
• Inpatient facility care, and all
other professional services
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Outpatient surgery center
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Anesthesiologist
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Dental Injury
• Office visit exams to determine
treatment needed
$50 copay per visit, deductible waived
Deductible, then 50% coinsurance
• Treatment
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Diagnostic X-Ray, Lab And
Imaging for medical conditions or
symptoms
Tests, lab, imaging and scans
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Diagnostic and supplemental breast
exams
No charge
Deductible, then 50% coinsurance
Dialysis
For permanent kidney failure. See
the Dialysis benefit for details.
• During Medicare's waiting period
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• After Medicare's waiting period
No charge
No cost-shares

YOUR SHARE OF THE ALLOWED AMOUNT
BENEFIT
IN-NETWORK PROVIDERS
OUT-OF-NETWORK PROVIDERS
4 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Emergency Room
• Facility charges
You may have additional costs
for other services. Examples are
X-rays or lab tests. See those
covered services for details.
The copay is waived if you are
admitted as an inpatient through
the emergency room. The copay
is waived if you are transferred
and admitted to a different
hospital directly from the
emergency room.
$150 copay per visit, then deductible,
then 20% coinsurance
$150 copay per visit, then deductible,
then 20% coinsurance
• Professional services
Deductible, then 20% coinsurance
Deductible, then 20% coinsurance
Foot Care
such as trimming nails or corns,
when medically necessary due to a
medical condition
• In an office or clinic
$25 or $50 copay per visit, deductible
waived
Deductible, then 50% coinsurance
• All other settings
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Gender Affirming Care
• Office and clinic visits
$25 or $50 copay per visit, deductible
waived
Deductible, then 50% coinsurance
• Other professional services
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Inpatient facility care
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Hearing Care
For hearing loss, often due to age
or noise exposure.
• Hearing Exams
Limit each calendar year:1
exam/test
No charge
Deductible, then 50% coinsurance
• Hearing Hardware
Limit of $3,000 per ear every 36
months
No charge
No cost-shares
Home Health Care
calendar year visit limit: None
• Home visits
• Prescription drugs billed by the
home health agency
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance

YOUR SHARE OF THE ALLOWED AMOUNT
BENEFIT
IN-NETWORK PROVIDERS
OUT-OF-NETWORK PROVIDERS
5 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Home Medical Equipment (HME),
Orthotics, Prosthetics And
Supplies
• Sales tax for covered items
• Foot orthotics and therapeutic
shoes; calendar year limit: $300
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
except diabetes related
• Medical vision hardware
Hospice Care
Lifetime limit for terminal illness: 6
months
Lifetime limit for non-terminal
illness: none
Inpatient stay limit: 30 days
Home visits: Unlimited
Respite care: 240 hours lifetime
max
• Inpatient facility care
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Home and respite care
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Prescription drugs billed by the
hospice
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Hospital
• Inpatient Care
• Professional
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Facility
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Outpatient Care
• Professional
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Facility
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Infusion Therapy
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Massage therapy
calendar year limit: 24 visits
$25 copay per visit, deductible waived
Deductible, then 50% coinsurance
Mastectomy and Breast
Reconstruction
• Office and clinic visits
$25 or $50 copay per visit, deductible
waived
Deductible, then 50% coinsurance
• Surgery and other professional
services
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Inpatient facility care
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance

YOUR SHARE OF THE ALLOWED AMOUNT
BENEFIT
IN-NETWORK PROVIDERS
OUT-OF-NETWORK PROVIDERS
6 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Maternity Care
Care during pregnancy, childbirth
and after the baby is born. See the
Preventive Care benefit for routine
exams and tests during pregnancy.
• Professional care
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Inpatient hospital, birthing
centers and short-stay hospitals
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Abortion
No charge
Deductible, then 50% coinsurance
Medical Foods
includes phenylketonuria (PKU)
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Medical Transportation
Travel and lodging are covered up
to the IRS limitations
• For Transplants: $7,500 overall
limit, per transplants
Deductible, then 0% coinsurance
In-network deductible, then 0%
coinsurance
• For Cellular Immunotherapy
and Gene Therapy: $7,500 per
episode of care
No charge
No cost-shares
Special criteria are required for
travel benefits to be provided.
Please see the benefit coverage for
details.
Medical Transportation – State
Restricted Care
Benefits are limited to members
residing in states where laws
restrict access to care. Travel and
lodging are covered up to the IRS
limitations. Prior approval required.
• To/from provider for abortion
services
No charge
No charge
• To/from provider for medically
necessary gender affirming care
services
No charge
No charge
• Calendar year limit: $4,000
Special criteria are required for
travel benefits to be provided. See
the benefit for coverage details.
Mental Health Care
• Office and clinic visits
$25 copay per visit, deductible waived
Deductible, then 50% coinsurance
• Other professional services
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Inpatient and residential facility
care
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Outpatient facility care
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance

YOUR SHARE OF THE ALLOWED AMOUNT
BENEFIT
IN-NETWORK PROVIDERS
OUT-OF-NETWORK PROVIDERS
7 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Neurodevelopmental Therapy
(Habilitation)
See the Mental Health Care
benefit for therapies for mental
conditions such as autism.
• Outpatient care
calendar year visit limit: 45 visits
• Office and clinic visits
$50 copay per visit, deductible waived
Deductible, then 50% coinsurance
• Other outpatient services
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Inpatient care
calendar year day limit: 45 days
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Newborn Care
• Inpatient care
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Office and clinic visits
$25 or $50 copay per visit, deductible
waived
Deductible, then 50% coinsurance
• Other outpatient services
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Orthognathic Surgery (Jaw
Augmentation or Reduction)
lifetime limit: None
• Office and clinic visits
$25 or $50 copay per visit, deductible
waived
Deductible, then 50% coinsurance
• Surgery and other professional
care
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Outpatient surgery facility care
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Inpatient hospital care
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Prescription Drug Deductible
Separate from medical deductible
In-Network Pharmacy
Out-Of-Network Pharmacy
• Generic drugs
Waived
Waived
• Individual deductible for brand-
name and specialty drugs
$250
$250 (separate from in-network drug
deductible)
• Family deductible for brand-
name and specialty drugs
$750
$750 (separate from in-network drug
deductible)
Covered Drugs*
In-Network Retail Pharmacy
Out-Of-Network Retail Pharmacy
• Preferred Generic drugs
$9 copay
$9 copay
plus 40% coinsurance
• Preferred brand name drugs
30% coinsurance
70% coinsurance
• Non-preferred generic and brand
name drugs
50% coinsurance
90% coinsurance

YOUR SHARE OF THE ALLOWED AMOUNT
BENEFIT
IN-NETWORK PROVIDERS
OUT-OF-NETWORK PROVIDERS
8 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
In-Network Mail-Order Pharmacy
Out-Of-Network Mail-Order
Pharmacy
• Preferred Generic drugs
$18 copay
Not covered
• Preferred brand name drugs
30% coinsurance
Not covered
• Non-preferred generic and brand
name drugs
50% coinsurance
Not covered
*Your cost shares for covered
prescription insulin drugs will not
exceed $35 per 30-day supply of
the drug. The deductible does not
apply. Cost shares for covered
prescription insulin drugs apply
toward the deductible.
Specialty Drugs (per prescription
or refill). You must use a specialty
pharmacy for these drugs to be
covered.
In-Network Mail-Order Pharmacy
Out-Of-Network Mail-Order
Pharmacy
• Preferred specialty drugs
40% coinsurance
Not covered
• Non-preferred specialty drugs
50% coinsurance
Not covered
Exceptions
In-Network Retail or In-Network
Mail Order Pharmacy
Out-Of-Network Retail Pharmacy
• Needles and syringes purchased
with diabetic drugs
No charge
No cost-shares
• Certain prescription drugs and
generic over-the-counter drugs to
break a nicotine habit
No charge
Same as out-of-network retail
• Drugs on the Affordable Care
Act's preventive drug list
No charge
Same as out-of-network retail
• Oral chemotherapy drugs
No charge
No cost-shares
• Female contraceptive drugs,
devices and supplies
(prescription and over-the-
counter). Includes emergency
contraceptives.
No charge
Same as out-of-network retail
• Male contraceptive drugs,
devices and supplies
(prescription and over-the-
counter).
No charge
Same as out-of-network retail

YOUR SHARE OF THE ALLOWED AMOUNT
BENEFIT
IN-NETWORK PROVIDERS
OUT-OF-NETWORK PROVIDERS
9 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Preventive Care
(Limits on how often services are
covered and who services are
recommended for may apply.)
• Preventive exams, including
vision and oral health screening
for members under 19, diabetes
and depression screening
No charge
Not covered
• Immunizations in the provider's
office
No charge
Not covered
• Flu shots and other seasonal
immunizations at a pharmacy or
mass immunizer location
No charge
No cost-shares
• Travel immunizations at a travel
clinic or county health
department
No charge
No cost-shares
• Health education and training
(outpatient)
No charge
Not covered
• Nicotine habit-breaking programs
No charge
Not covered
• Fall prevention for members 65
and older
No charge
Not covered
• Nutritional counseling and
therapy
No charge
Deductible, then 50% coinsurance
• Pregnant member's care
(includes breast-feeding support
and post-partum depression
screening)
No charge
Deductible, then 50% coinsurance
• Screening tests (includes
prostate and cervical cancer
screening)
No charge
Deductible, then 50% coinsurance
• Screening mammograms
No charge
Deductible, then 50% coinsurance
• Colorectal cancer screening
No charge
Deductible, then 50% coinsurance
• Contraceptive and sterilization.
No charge
Deductible, then 50% coinsurance
YOUR SHARE OF THE ALLOWED AMOUNT
BENEFIT
IN-NETWORK PROVIDERS
OUT-OF-NETWORK PROVIDERS
10 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Professional Visits and Services
You may have extra costs for other
services like lab tests and facility
charges. Also see Allergy Testing
And Treatment and Therapeutic
Injections.
• Office and clinic visits, including
real-time visits using online and
telephonic methods with a
provider who also maintains a
physical location
$25 or $50 copay per visit, deductible
waived
Deductible, then 50% coinsurance
• Telemedicine with Traditional
Providers (General Medical)
$25 or $50 copay per visit, deductible
waived
Deductible, then 50% coinsurance
• Electronic visits (e-visits)
$25 or $50 copay per visit, deductible
waived
Not covered
• Other professional services
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Psychological and
Neuropsychological Testing
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Rehabilitation Therapy
Cardiac or pulmonary rehabilitation
programs, or similar programs for
cancer or other chronic conditions
are not subject to a benefit limit.
• Outpatient Care
calendar year visit limit: 45 visits
• Office and clinic visits
$50 copay per visit, deductible waived
Deductible, then 50% coinsurance
• Other outpatient services
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Inpatient Care
calendar year day limit: 45 days
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Skilled Nursing Facility Care
calendar year day limit: None
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Spinal and Other Manipulations
calendar year visit limit: 24 visits
$25 copay per visit, deductible waived
Deductible, then 50% coinsurance
Substance Use Disorder
• Office and clinic visits
$25 copay per visit, deductible waived
Deductible, then 50% coinsurance
• Other professional services
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Inpatient care and residential
facility care
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Outpatient facility care
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance

YOUR SHARE OF THE ALLOWED AMOUNT
BENEFIT
IN-NETWORK PROVIDERS
OUT-OF-NETWORK PROVIDERS
11 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Surgery
(includes professional services,
anesthesia and blood transfusions)
See the Hospital and Surgical
Center Care - Outpatient benefits
for facility charges.
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Vasectomy
No charge
Deductible, then 50% coinsurance
Surgical Center Care – Outpatient
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Temporomandibular Joint
Disorders (TMJ) Care
• Office and clinic visits
$25 or $50 copay per visit, deductible
waived
Deductible, then 50% coinsurance
• Other professional services
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Inpatient facility care
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Therapeutic Injections
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
Transplants
(Includes donor search and
donation costs)
• Inpatient facility care
Deductible, then 20% coinsurance
Not covered*
• Office and clinic visits
$25 or $50 copay per visit, deductible
waived
Not covered*
• Surgery and other professional
services
Deductible, then 20% coinsurance
Not covered*
*All approved transplant centers
covered at the in-network level
Please see Medical
Transportation for travel and
lodging benefits.
Urgent Care
Services at an urgent care center.
See Diagnostic X-Ray, Lab And
Imaging for tests received while at
the center. Your deductible and
coinsurance apply to facility
charges.
• Freestanding urgent care centers
Deductible, then 20% coinsurance
Deductible, then 50% coinsurance
• Urgent care centers attached to
or part of a hospital
$150 copay per visit, then deductible,
then 20% coinsurance
$150 copay per visit, then deductible,
then 20% coinsurance

YOUR SHARE OF THE ALLOWED AMOUNT
BENEFIT
IN-NETWORK PROVIDERS
OUT-OF-NETWORK PROVIDERS
12 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Virtual Care
Access to medical care using virtual
methods like secure chat, text,
voice or video chat.
Real-time visits via online or
telephonic methods with your doctor
or other provider who also
maintains a physical location, are
covered under other benefits of this
plan.
The same copay applies to both
specialists and non-specialists.
• Virtual general
medical/dermatology visits
$5 copay, deductible waived
Not applicable
• Virtual behavioral/mental health
$25 copay, deductible waived
Not applicable
• Virtual substance use disorder
visit
$25 copay, deductible waived
Not applicable
Weight Management
• Non-surgical weight management
As any other covered service
As any other covered service
• Surgical weight loss treatment
(Bariatric Surgery)
Deductible, then 20% coinsurance
Not covered
See the Weight Management
benefit for additional benefit
information.
13 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
HOW PROVIDERS AFFECT YOUR COSTS
This plan's benefits and your out-of-pocket expenses depend on the providers you see. In this section you’ll find
out how the providers you see can affect this plan's benefits and your costs.
This plan makes available to you sufficient numbers and types of providers to give you access to all covered
services in compliance with applicable Washington state regulations governing access to providers. Our provider
networks include hospitals, physicians, and a variety of other types of providers.
This plan does not require use or selection of a primary care provider or require referrals for specialty care.
Members may self-refer to providers, including obstetricians, gynecologists and pediatricians, to receive care, and
may do so without prior authorization.
In-Network Providers
This plan is a Preferred Provider Plan (PPO). This means that the plan provides you benefits for covered
services from providers of your choice. Its benefits are designed to provide lower out-of-pocket expenses when
you receive care from in-network providers. There are some exceptions, which are explained below.
In-Network providers are:
• Providers in the Heritage Prime network in Washington. For accessing care in Clark County, Washington, you
also have access to providers through the BlueCard
®
Program.
• Providers in Alaska that have signed contracts with Premera Blue Cross Blue Shield of Alaska.
• For care outside the service area (see Definitions), providers in the local Blue Cross and/or Blue Shield
Licensee's network shown below. (These Licensees are called “Host Blues” in this booklet.) See Out-Of-Area
Care later in the booklet for more details.
• Wyoming: The Host Blue's Traditional (Participating) network
• All Other States: The Host Blue's PPO (Preferred) network
In-Network pharmacies are available nationwide.
In-Network providers provide medical care to members at negotiated fees. These fees are the allowed amounts
for in-network providers. When you receive covered services from an in-network provider, your medical bills will
be reimbursed at a higher percentage (the in-network benefit level). This means lower cost shares for you, as
shown in the Summary Of Your Costs. In-Network providers will not charge you more than the allowed amount
for covered services. This means that your portion of the charges for covered services will be lower.
Your choice of a particular provider may affect your out-of-pocket costs because different providers may have
different allowed amounts even though they all have an agreement with us or with the same Host Blue. You’ll
never have to pay more than your share of the allowed amount for covered services when you use in-network
providers.
A list of in-network providers is in our Heritage Prime provider directory. You can access the directory at any time
on our website at www.premera.com/sebb. You may also ask for a copy of the directory by calling customer
service. The providers are listed by geographical area, specialty and in alphabetical order to help you select a
provider that is right for you. You can also call the BlueCard provider line to locate an in-network provider. The
numbers are on the back cover of this booklet and on your Premera Blue Cross ID card.
We update this directory regularly, but the listings can change. Before you get care, we suggest that you call us
for current information or to make sure that your provider, their office location or their provider group is in the
Heritage Prime network.
Contracted Health Care Benefit Managers
The list of Premera’s contracted Health Care Benefit Managers (HCBM) and the services they manage are
available at partners-vendors and changes to these contracts or services are reflected on the website within 30
business days.
Continuity of Care
How Continuity of Care Works If a primary care provider contract is terminated without cause, continuing care
will be provided according to the details included in the member's notice of the contract termination. Additionally,
14 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
you may qualify for continuing care from non-primary care providers for Continuity of Care (COC) under certain
circumstances when a provider leaves your health plan’s network or your employer transitions to a new carrier.
This will depend on your medical condition at the time the change occurs. COC is a process that provides you
with short-term, temporary coverage at in-network levels for care received by a non-participating provider.
COC applies in these situations:
• The contract with your provider ends
• The benefits covered for your provider change in a way that results in a loss of coverage
• The contract between your company and us ends and that results in a loss of coverage with your provider
How you qualify for Continuity of Care You may qualify if you are in an "active relationship" or treatment with
your provider. This means that you have had three or more visits with the provider within the past 12 months and
you meet one or more of these conditions with respect to a terminated provider or facility :
• Undergoing a course of treatment for a serious and complex condition
• Undergoing a course of institutional or inpatient care
• Are scheduled for a non-elective surgery, including receipt of postoperative care
• Are pregnant and undergoing a course of treatment for the pregnancy
• Are receiving treatment for a terminal illness
We will notify you at least 30 days prior to your provider’s termination date. When a termination for cause
provides us less than 30 days notice, we will make a good faith effort to assure that a written notice is provided to
you immediately.
You can request continuity of care by contacting customer service. The contact information is on the back cover
of this booklet.
If you are approved for continuity of care, you will get continuing care from the terminating provider until the
earliest of the following:
• The 90
th
day after we notified you that your provider's contract ended
• The day after you complete the active course of treatment entitling you to continuity of care
If you are pregnant, and become eligible for continuity of care, you can continue with your provider throughout
your pregnancy, plus 8 weeks of postpartum care.
Continuity of care does not apply if your provider:
• No longer holds an active license
• Relocates out of the service area
• Goes on leave of absence
• Is unable to provide continuity of care because of other reasons
• Does not meet standards of quality of care
When continuity of care ends, non-emergent care from the provider is no longer covered. If we deny your request
for continuity of care, you may appeal the denial. See Complaints and Appeals.
Non-Participating Providers
Non-participating providers are either (1) providers that are not in one of the networks (Out-Of-Network) shown
above or (2) providers that do not have a contract with us (Non-Contracted). Except as stated in Benefits For
Out-Of-Network Or Non-Contracted Providers, or in a few specific benefits, services from these providers are
not covered.
• Out-of-Network Some providers in Washington have a contract with but are not in the Heritage Prime network.
In cases where this plan covers services from these providers, they will not bill you for any amount above the
allowed amount for a covered service. The same is true for a provider that is in a different network of the local
Host Blue plan.
• Non-Contracted Providers There are also providers who do not have a contract with us, Premera Blue Cross
Blue Shield of Alaska or the local Host Blue at all. These providers are called "non-contracted" providers in this
booklet. You may also be required to submit the claim yourself. See How Do I File A Claim? for details.
15 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Balance Billing Protection
Non-participating providers have the right to charge you more than the allowed amount for a covered service. This
is called "surprise billing" or "balance billing." However, [Washington state and] federal law protects you from
balance billing for:
Emergency Services from a nonparticipating hospital or facility or from a nonparticipating provider at the hospital
or facility.
Emergency services includes certain post-stabilization services you may get after you are in stable condition.
These include covered services provided as part of outpatient observation or during an inpatient or outpatient stay
related to the emergency visit, regardless of which department of the hospital you are in.
Non-emergency services from a nonparticipating provider at an in-network hospital or outpatient surgery
center. If a non-emergency service is not covered under the in-network benefits and terms of coverage under
your health plan, then the federal and state law regarding balance billing do not apply for these services.
Air Ambulance
Your cost sharing for non-participating air ambulance services shall be no more than if the services were provided
by an in-network provider. The cost sharing amount shall be counted towards the in-network deductible and the
in-network out of pocket maximum amount. Cost sharing shall be based upon the lesser of the qualifying payment
amount (as defined under federal law) or the billed amount.
For the above services, you will pay no more than the plan's in-network cost shares. See the Summary of Your
Costs. Premera Blue Cross will work with the nonparticipating provider to resolve any issues about the amount
paid. Premera will also send the plan's payments to the provider directly.
Please Note: The surprise billing protection does not apply to any other service from a non-contracted provider.
If the service is not listed above, you must pay any amounts over the plan’s allowed amount for the service
Amounts you pay over the allowed amount don’t count toward any applicable calendar year deductible,
coinsurance or out-of-pocket maximum.
Benefits For Out-Of-Network Or Non-Contracted Providers
The following covered services and supplies provided by out-of-network or non-contracted providers will always
be covered:
• Emergency services for an emergency medical condition. See the Definitions section for definitions of these
terms. This plan provides worldwide coverage for emergency services.
The benefits of this plan will be provided for covered emergency services without the need for any prior
authorization and without regard as to whether the health care provider furnishing the services has a contract
with us. Emergency services furnished by a non-participating provider will be reimbursed in compliance with
applicable laws.
• Services from certain categories of providers to which provider contracts are not offered. These types of
providers are not listed in the provider directory.
• Facility and hospital-based provider services received from a hospital that has a provider contract with Premera
Blue Cross.
• Covered services received from providers located outside the United States, the Commonwealth of Puerto Rico
and the U.S. Virgin Islands.
If a covered service is not available from an in-network provider, you can receive benefits for services provided by
an out-of-network or non-contracted provider. However, you or your out-of-network provider must request this
before you get the care. See Prior authorization to find out how to do this.
IMPORTANT PLAN INFORMATION
This section of your booklet explains the types of expenses you must pay for covered services before the benefits
of this plan are provided. (These are called “cost shares” in this booklet.) To prevent unexpected out-of-pocket
expenses, it’s important for you to understand what you’re responsible for.
The allowed amount is also explained.
You'll find the dollar amounts for these expenses and when they apply in the Summary Of Your Costs.
16 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
COPAYMENTS (COPAYS)
Copayments (“copays”) are fixed up-front dollar amounts that you’re required to pay for certain covered services.
Your provider of care may ask that you pay the copay at the time of service. If the amount billed is less than the
copay, you only pay the amount billed. Your copay amounts are shown in the Summary Of Your Costs.
SPLIT COPAY FOR OFFICE VISITS
This plan has two Professional Visit Copay amounts for in-network providers' office and home visits. When you
see one of the types of in-network providers shown below, you pay the non-specialist copay shown in the
Summary Of Your Costs for each office or home visit.
• Family practice physician
• General practice physician
• Internist
• Gynecologist
• Naturopath
• Advanced registered nurse practitioner (ARNP)
• Obstetrician
• Pediatrician
• Physician assistant
• Chiropractor
• Acupuncturist
Certain services don’t require a copay. However, the Professional Visit Copay may apply if you have a
consultation with the provider or receive other services. Separate copays will apply if you see more than one in-
network provider on the same day. But only one copay per provider, per day will apply. If you receive multiple
services from the same provider in the same visit and the copay amounts are different, then the highest copay will
apply.
For all other types of in-network providers covered by benefits subject to a professional visit copay, you pay the
specialist copay shown in the Summary Of Your Costs for each visit.
CALENDAR YEAR DEDUCTIBLE
A calendar year deductible is the amount of expense you must incur in each calendar year for covered services
and supplies before this plan makes a payment for most covered services. The amount credited toward the
calendar year deductible for any covered service or supply won’t exceed the allowed amount See the Allowed
Amount subsection below in this booklet.
While some benefits have dollar maximums, others have different kinds of maximums, such as a maximum
number of visits or days of care that can be covered. We don't count allowed amounts that apply to your
individual in-network or out-of-network calendar year deductibles toward dollar benefit maximums. But if you
receive services or supplies covered by a benefit that has any other kind of maximum, we do count the services
or supplies that apply to either of your individual calendar year deductibles toward that maximum.
The plan has separate deductibles for in-network and out-of-network providers. It could happen that you
satisfy one of these deductibles before the other. If this happens, you still have to pay cost-shares that
apply to the second deductible until it, too, is met.
Note: Each calendar year deductible accrues toward its applicable out-of-pocket maximum, if any.
Individual Deductible
An “Individual Deductible” is the amount each member must incur and satisfy before certain benefits of this plan
are provided.
Family Deductible
In addition to the individual deductible, we also keep track of the expenses applied to the family deductible which
are incurred by all enrolled family members combined. When the total equals a set maximum, called the “Family
Deductible,” we will consider the individual deductible of every enrolled family member to be met for the year.
17 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Only the amounts used to satisfy each enrolled family member's individual deductible will count toward the family
deductible.
Please note: No enrolled family member will be required to satisfy more than the individual deductible amount .
What Doesn't Apply To The Calendar Year Deductible?
Amounts that don't accrue toward this plan's calendar year deductible are:
• Amounts that exceed the allowed amount
• Charges for excluded services
• The penalty for not asking for prior authorization when the plan requires it. See Prior Authorization in the
Care Management section of this booklet.
• The difference in cost between a brand name drug and an equivalent generic drug when the plan requires the
generic drug to be dispensed in place of the brand name drug.
• Copays
• The coinsurance for in-network pharmacies stated in the Summary Of Your Costs
COINSURANCE
“Coinsurance” is a defined percentage of allowed amounts for covered services and supplies you receive. It's the
percentage you’re responsible for, not including copays and the calendar year deductible, when the plan provides
benefits at less than 100% of the allowed amount. You will find your coinsurance in the Summary Of Your
Costs.
OUT-OF-POCKET MAXIMUM
The “individual out-of-pocket maximum” is the maximum amount, made up of the cost shares below, that each
individual could pay each calendar year for certain covered services and supplies. Refer to the Summary Of
Your Costs for the amount of out-of-pocket maximums you're responsible for.
Once the out-of-pocket maximum has been satisfied, the benefits of this plan will be provided at 100% of
allowed amounts for the remainder of that calendar year for covered services that are subject to the
maximum.
Cost shares that apply to the out-of-pocket maximum are:
• Your coinsurance
• The calendar year deductibles
Once the family deductible is met, your individual deductible will be satisfied. However, you must still pay any
other cost shares shown in the Summary Of Your Costs until your individual out-of-pocket maximum is
reached.
• Copays
• The difference in cost between a brand name drug and an equivalent generic drug when the plan requires the
generic drug to be dispensed in place of the brand name drug.
There are some exceptions. Expenses that do not apply to the out-of-pocket maximum are:
• Charges above the allowed amount
• Charges not covered by the plan
• Copays for exams covered under the Hearing Exams benefit
• The penalty for not requesting prior authorization when needed. See Prior Authorization in the Care
Management section of this booklet.
In addition to the individual out-of-pocket maximum, we also keep track of the expenses applied to the family out-
of-pocket maximum which are incurred by all enrolled family members combined. When this total equals a set
maximum, called the “Family Out-of-Pocket Maximum,” we will consider the individual out-of-pocket maximum of
every enrolled family member to be met for that calendar year. Only the amounts used to satisfy each enrolled
family member’s individual out-of-pocket maximum will count toward the family out-of-pocket maximum.
Please note: In order to satisfy the in-network out-of-pocket amount, no enrolled family member has to pay more
than the individual out-of-pocket maximum.
18 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
ALLOWED AMOUNT
This plan provides benefits based on the allowed amount for covered services. We reserve the right to determine
the amount allowed for any given service or supply. The allowed amount is described below. There are different
rules for certain services as described below. These rules are shown below the general rules.
General Rules
• Providers In Washington and Alaska Who Have Agreements With Us
For any given service or supply, the amount these providers have agreed to accept as payment in full pursuant
to the applicable agreement between us and the provider. These providers agree to seek payment from us
when they furnish covered services to you. You’ll be responsible only for any applicable calendar year
deductibles, copays, coinsurance, charges in excess of the stated benefit maximums and charges for services
and supplies not covered under this plan.
Your liability for any applicable calendar year deductibles, coinsurance, copays and amounts applied toward
benefit maximums will be calculated on the basis of the allowed amount.
• Providers Outside The Service Area Who Have Agreements With Other Blue Cross Blue Shield
Licensees
For covered services and supplies received outside the service area, allowed amounts are determined as
stated in the What Do I Do If I’m Outside Washington And Alaska? section (Out-Of-Area Care) in this
booklet.
• Providers Who Don’t Have Agreements With Us Or Another Blue Cross Blue Shield Licensee
Except as stated below, the allowed amount for providers in the service area that don't have a contract with us
is the least of the three amounts shown below. The allowed amount for providers outside Washington or
Alaska that don't have a contract with us or the local Blue Cross and/or Blue Shield Licensee is also the least of
the three amounts shown below.
• An amount that is no less than the lowest amount the plan pays for the same or similar service from a
comparable provider that has a contracting agreement with us
• 125% of the fee schedule determined by the Centers for Medicare and Medicaid Services (Medicare), if
available
• The provider’s billed charges. Note: Ground ambulances are always paid based on billed charges.
If applicable law requires a different allowed amount than the least of the three amounts above, this plan will
comply with that law.
Non-Emergency Services Protected From Balance Billing
For these services, the allowed amount is calculated consistent with the requirements of federal or Washington
state law.
Emergency Services
The allowed amount for non-participating providers will be calculated consistent with the requirements of federal
or Washington state law. You do not have to pay amounts over the allowed amount for emergency services
delivered by non-participating providers or facilities.
Note: Non-participating ground ambulances are always paid based on billed charges.
If you have questions about this information, please call us at the number listed on your Premera Blue Cross ID
card.
Air Ambulance
The allowed amount for non-participating air ambulance providers will be calculated consistent with the
requirements of federal law.
COVERED SERVICES
This section of your booklet describes the services and supplies that the plan covers. Benefits are available for a
service or supply described in this section when it meets all of these requirements:
• It must be furnished in connection with either the prevention or diagnosis and treatment of a covered illness,
disease or injury.
19 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• It must be medically necessary (see the
Definitions
section in this booklet) and must be furnished in a
medically necessary setting.
• It must not be excluded from coverage under this plan.
• The expense for it must be incurred while you’re covered under this plan.
• It must be furnished by a “provider” (see the
Definitions
section in this booklet) who’s performing services
within the scope of their license or certification.
• It must meet the standards set in our medical and payment policies. The plan uses policies to administer the
terms of the plan. Medical policies are generally used to further define medical necessity or investigational
status for specific procedures, drugs, biologic agents, devices, level of care or services. Payment policies
define our provider billing and payment rules. Our policies are based on accepted clinical practice guidelines
and industry standards accepted by organizations like the American Medical Association (AMA), other
professional societies and the Center for Medicare and Medicaid Services (CMS). Our policies are available to
you and your provider at www.premera.com/sebb or by calling customer service.
Benefits for some types of services and supplies may be limited or excluded under this plan. Refer to the actual
benefit provisions throughout this section and the Exclusions section for a complete description of covered
services and supplies, limitations and exclusions. You will find limits on days or visits and dollar limits in the
Summary Of Your Costs.
The Summary Of Your Costs also explains your cost share under each benefit.
Acupuncture
The technique of inserting thin needles through the skin at specific points on body to help control pain and other
symptoms. Services must be provided by a certified or licensed acupuncturist.
This benefit covers acupuncture to:
• Relieve pain
• Provide anesthesia for surgery
• Treat a covered illness, injury, or condition
See the Summary of Your Costs for benefit limitations.
Note: Acupuncture services when provided for substance use disorder conditions do not apply to the
Acupuncture benefit visit limits.
Allergy Testing and Treatment
Skin and blood tests used to diagnose what substances a person is allergic to, and treatment for allergies.
Services must be provided by a certified or licensed allergy specialist.
This benefit covers:
• Testing
• Allergy shots
• Serums
Ambulance
This benefit covers:
• Transport to the nearest facility that can treat your condition
• Medical care you get during the trip
• Transport from one medical facility to another as needed for your condition
• Transport to your home when medically necessary
These services are only covered when:
• Any other type of transport would put your health or safety at risk
• The service is from a licensed ambulance
• It is for the member who needs transport
20 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Air or sea emergency medical transportation is covered when:
• Transport takes you to the nearest available facility that can treat your condition
• The above requirements for ambulance services are met
• Geographic restraints prevent ground transport
• Ground emergency transportation would put your health or safety at risk
Ambulance services that are not for an emergency must be medically necessary and need prior authorization.
See Prior Authorization for details.
Blood Products And Services
• Blood components and services, like blood transfusions, which are provided by a certified or licensed
healthcare provider.
• Blood products and services that either help with prevention or diagnosis and treatment of an illness, disease,
or injury.
Cellular Immunotherapy And Gene Therapy
Treatment which uses your body’s own immune system or genes to treat disease.
These therapies are fairly new, and their use is evolving. They must meet three criteria in order to be covered:
• Prescribed by a provider
• Meet Premera’s medical policy (See www.premera.com/sebb or call customer service), and
• Approved by Premera before they can happen (See Prior Authorization)
This benefit covers:
Medically necessary cellular immunotherapy and gene therapy, like Chimeric Antigen Receptor T-Cell (CAR-T).
If you travel more than 50 miles for these therapies, keep all receipts. You can be reimbursed for some expenses,
up to $7,500 per episode of care. See Medical Transportation.
See Prior Authorization for more information on getting prior approval for services.
Chemotherapy And Radiation Therapy
Treatment which uses powerful chemicals (chemotherapy) or high-energy beams (radiation) to shrink or kill
cancer cells.
Chemotherapy and radiation must be prescribed by a doctor and approved by Premera to be covered. See Prior
Authorization.
This benefit covers:
• Outpatient chemotherapy and radiation therapy
• Supplies, solutions and drugs used during chemotherapy or radiation visit
• Tooth extractions to prepare your jaw for radiation therapy
For chemotherapy drugs you get from a pharmacy, see Prescription Drug. Some services need to be pre-
approved before you get them. See Prior Authorization for details.
Clinical Trials
A qualified clinical trial (see Definitions) is a scientific study that tests and improves treatments of cancer and
other life-threatening conditions.
This benefit covers qualified clinical trial medical services and drugs that are already covered under this plan.
The clinical trial must be suitable for your health condition. You also have to be enrolled in the trial at the time of
treatment.
Benefits are based on the type of service you get. For example, if you have an office visit, it's covered under
Professional Visits And Services and if you have a lab test, it's covered under Diagnostic X-Ray, Lab And
Imaging.
21 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
This benefit doesn't cover:
• Costs for treatment that are not primarily for the care of the patient (such as lab tests performed just to collect
information for the trial)
• The drug, device or services being tested
• Travel costs to and from the clinical trial
• Housing, meals, or other nonclinical expenses
• A service that isn't consistent with established standards of care for a certain condition
• Services, supplies or drugs that would not be charged to you if there were no coverage.
• Services provided to you in a clinical trial that are fully paid for by another source
• Services that are not routine costs normally covered under this plan
Dental Injury and Facility Anesthesia
This benefit will only be provided for the dental services listed below.
Dental Anesthesia
Anesthesia and facility care done outside of the dentist’s office for medically necessary dental care
This benefit covers:
• Hospital or other facility care
• General anesthesia provided by an anesthesia professional other than the dentist or the physician performing
the dental care
This benefit is covered for any one of the following reasons:
• The member is under age 19 and failed patient management in the dental office
• The member has a disability, medical or mental health condition making it unsafe to have care in a dental office
• The severity and extent of the dental care prevents care in a dental office
Dental Injury
Treatment of dental injuries to teeth, gum and jaw.
This benefit covers:
• Exams
• Consultations
• Dental treatment
• Oral surgery
This benefit is covered on sound and natural teeth that:
• Do not have decay
• Do not have a large number of restorations such as crowns or bridge work
• Do not have gum disease or any condition that would make them weak
Care is covered within 12 months of the injury. If more time is needed, please ask your doctor to contact
customer service.
Benefits are based on the type of service you get. For example, if you have an office visit, it's covered under
Professional Visits And Services, and if you have a lab test it's covered under Diagnostic X-ray, Lab and
Imaging.
This benefit does not cover injuries from biting or chewing, including injuries from a foreign object in food.
Diagnostic X-Ray, Lab And Imaging
Diagnostic x-ray, lab and imaging services are medical tests that help find or identify diseases.
For more information about what services are covered as preventive see Preventive Care. A typical test can
result in multiple charges for things like an office visit, test, and anesthesia. You may receive separate bills for
22 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
each charge. Some tests need to be approved before you receive them. See Prior Authorization for details.
Covered services include:
• Bone density screening for osteoporosis
• Cardiac testing
• Pulmonary function testing
• Diagnostic imaging and scans such as x-rays
• Lab services
• Mammograms (including 3-D mammograms) for a medical condition
• Neurological and neuromuscular tests
• Pathology tests
• Echocardiograms
• Ultrasounds
• Diagnosis and treatment of the underlying medical conditions that may cause infertility
• Computed Tomography (CT) scan
• Nuclear cardiology
• Magnetic Resonance Imaging (MRI)
• Magnetic Resonance Angiography (MRA)
• Positron Emission Tomography (PET) scan
Diagnostic breast examination for the purpose of this Diagnostic X-Ray, Lab, And Imaging benefit means a
medically necessary and appropriate examination of the breast, including an examination using diagnostic
mammography breast magnetic resonance imaging, or breast ultrasound, that is used to evaluate an abnormality:
• seen or suspected from a screening examination for breast cancer; or
• detected by another means of examination
Supplemental breast examination for the purpose of this Diagnostic X-Ray, Lab, And Imaging benefit means a
medically necessary and appropriate examination of the breast, including an examination using breast magnetic
resonance imaging or breast ultrasound, that is:
• used to screen for breast cancer when there is no abnormality seen or suspected; and
• based on personal or family medical history, or additional factors that may increase the member's risk or
breast cancer
For additional details see the following benefits:
• Emergency Room
• Hospital
• Maternity Care
• Preventive Care
• Genetic testing may be covered in some cases. Call customer service before seeking testing since it may
require prior authorization. Please note that biomarker testing is covered. When prescribed by an in-network
provider, Prior Authorization is not required for members with state 3 or 4 cancer, or for members with
recurrent, relapsed, refractory, or metastatic cancer.
Dialysis
When you have end-stage renal disease (ESRD) you may be eligible to enroll in Medicare. If eligible, it is
recommended to enroll in Medicare as soon as possible. When you enroll in Medicare, this plan and Medicare
will coordinate benefits. In most cases, this means that you will have little or no out-of-pocket expenses.
As soon as you are enrolled in Medicare Part B, Premera Blue Cross will pay your Medicare Part B premiums.
Premera Blue Cross will continue to pay these premiums for as long as you are enrolled in this plan and eligible
for Medicare due to ESRD.
23 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Medicare has a waiting period, generally the first 90 days after dialysis starts. Benefits are different for dialysis
during Medicare's waiting period than after the waiting period ends. See the Summary Of Your Costs.
When covered dialysis services are provided by an out-of-network provider in a county in Washington state where
no in-network providers are available, the in-network cost shares will apply.If the dialysis services are provided by
a non-contracted provider and you do not enroll in Medicare, then you will owe the difference between the non-
contracted provider's billed charges and the payment we will make for the covered services.
Emergency Room
This benefit covers:
• Emergency room and provider services
• Equipment, supplies and drugs used in the emergency room
• Services and exams used for stabilizing an emergency medical condition, including mental health, or substance
use disorder.
• Diagnostic tests performed with other emergency services
• Medically necessary detoxification
You need to let us know if you are admitted to the hospital from the emergency room as soon as possible. See
Prior Authorization for details.
Foot Care
This benefit covers:
• Medically necessary foot care
• Treatment of corns and calluses
• Treatment of certain toenail conditions
This benefit does not cover routine foot care, such as trimming nails or removing corns and calluses that do not
need care from a provider.
Gender Affirming Care
Benefits for medically necessary gender affirming care services are subject to the same cost shares that you
would pay for inpatient or outpatient treatment for other covered medical conditions, for all ages. To find the
amounts you are responsible for, see the Summary of Your Costs earlier in this booklet.
Benefits are provided for all gender affirming care surgical services which meet the Premera medical policy,
including facility and anesthesia charges related to the surgery. Our medical policies are available from customer
service, or at www.premera.com/sebb.
Benefits for gynecological, urologic and genital surgery for covered medical and surgical conditions, other than as
part of gender affirming care surgery, are covered under the surgical benefits applicable to those conditions.
Note: Coverage of prescription drugs, and mental health treatment associated with gender affirming surgery, are
eligible under the general plan provisions for prescription drugs and behavioral health, subject to the applicable
plan limitations and exclusions.
For members residing in states where laws prohibit access to medically necessary gender affirming care services,
travel to a provider in another state may be covered. Please see Medical Transportation – State-Restricted
Care for details.
Hearing Care
Hearing Exams
Hearing exam services include:
• Examination of the inner and exterior of the ear
• Observation and evaluation of hearing, such as whispered voice and tuning fork tests
• Case history and recommendations
• Hearing testing services, including the use of calibrated equipment.
24 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
The Hearing Exams benefit doesn’t cover hearing hardware or fitting examinations for hearing hardware.
Hearing Hardware
To receive your hearing hardware benefit:
• You must be examined by a licensed physician (M.D. or D.O.) or audiologist (CCC-A or CCC-MSPA) before
obtaining hearing aids
• You must purchase a hearing aid device
Benefits are provided for the following:
• Hearing aids (monaural or binaural) prescribed as a result of an exam
• Ear molds
• The hearing aid instruments
• Hearing aid rental while the primary unit is being repaired
• The initial batteries, cords and other necessary ancillary equipment
• A warranty, when provided by the manufacturer
• A follow-up consultation within 30 days following delivery of the hearing aids with either the prescribing
physician or audiologist
• Repairs, servicing, and alteration of hearing aid equipment purchased under this benefit
This benefit doesn't cover:
• Hearing aids purchased before your effective date of coverage under this plan
• Batteries or other ancillary equipment other than that obtained upon purchase of the hearing aids
• Hearing aids that exceed the specifications prescribed for correction of hearing loss
• Expenses incurred after your coverage under this plan ends unless hearing aids were ordered before that date
and were delivered within 90 days after the date your coverage ended
• Charges in excess of this benefit. These expenses are also not eligible for coverage under other benefits of
this plan.
Home Health Care
General Home Health Care
General Home Health Care is short-term care performed at your home. These occasional visits are done by a
medical professional that’s employed through a home health agency that is state-licensed or Medicare-certified.
Care is covered when a provider states in writing that care is needed in your home.
The following are covered under the Home Health Care benefit:
• Home visits and short-term nursing care
• Home medical equipment, supplies and devices
• Prescription drugs given by the home health care agency
• Therapy, such as physical, occupational or speech therapy to help regain function
Only the following employees of a home health agency are covered:
• A registered nurse
• A licensed practical nurse
• A licensed physical or occupational therapist
• A certified speech therapist
• A certified respiratory therapist
• A home health aide directly supervised by one of the above listed providers
• A social worker
25 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Skilled Hourly Nursing
Skilled Hourly Nursing is also covered under the Home Health Care benefit. Skilled Hourly Nursing is medically
intensive care at home that is provided by a licensed nurse.
Home health care can be a substitute for hospitalization or inpatient care if hospitalization or inpatient care is
medically necessary and such home care:
• can be provided at equal or lesser cost;
• is the most cost-effective setting and appropriate
• is with your consent and recommended by your attending physician or licensed health care provider that such
care will adequately meet your needs
You must have a written plan of care from your doctor and requires prior authorization by the plan. See Prior
Authorization. This type of care is not subject to any visit limit shown in the Summary of Your Costs.
The Home Health Care benefit does not cover:
• Over-the-counter drugs, solutions and nutritional supplements
• Private duty or 24-hour nursing care. Private duty nursing is the independent hiring of a nurse by a family or
member to provide care without oversight by a home health agency. The care may be skilled, supportive or
respite in nature.
• Non-medical services, such as housekeeping
• Services that bring you food, such as Meals on Wheels, or advice about food
Home Medical Equipment (HME), Orthotics, Prosthetics And Supplies
This benefit covers:
Home medical equipment (HME), fitting expenses and sales tax. This plan also covers rental of HME, not to
exceed the purchase price.
Covered items include:
• Wheelchairs
• Hospital beds
• Traction equipment
• Ventilators
• Diabetic equipment, such as an insulin pump
Medical Supplies such as:
• Dressings
• Braces
• Splints
• Rib belts
• Crutches
• Blood glucose monitor and supplies
• Supplies for an insulin pump
Medical Vision Hardware to correct vision due to the following medical eye conditions:
• Corneal ulcer
• Bullous keratopathy
• Recurrent erosion of cornea
• Tear film insufficiency
• Aphakia
• Sjogren’s disease
• Congenital cataract
26 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• Corneal abrasion
• Keratoconus
• Progressive high (degenerative) myopia
• Irregular astigmatism
• Aniridia
• Aniseikonia
• Anisometropia
• Corneal disorders
• Pathological myopia
• Post-traumatic eye disorders
External Prosthetics and Orthotic Devices used to:
• Replace absent body limb and/or
• Replace broken or failing body organ
Orthopedic Shoes and Shoe Inserts
Orthopedic shoes for the treatment of complications from diabetes or other medical disorders that cause foot
problems.
You must have a written order for the items. Your provider must state your condition and estimate the period of its
need. Not all equipment or supplies are covered. Some items need prior authorization from us. See Prior
Authorization.
This benefit does not cover:
• Hypodermic needles, lancets, test strips, testing agents and alcohol swabs. These services are covered under
Prescription Drug.
• Supplies or equipment not primarily intended for medical use
• Special or extra-cost convenience features
• Items such as exercise equipment and weights
• Over bed tables, elevators, vision aids, and telephone alert systems
• Over-the-counter orthotic braces and/or cranial banding
• Non-wearable external defibrillators, trusses and ultrasonic nebulizers
• Blood pressure cuffs/monitors (even if prescribed by a physician)
• Enuresis alarm
• Compression stockings which do not require a prescription
• Physical changes to your house or personal vehicle
• Orthopedic shoes used for sport, recreation or similar activity
• Penile prostheses
• Routine eye care
• Prosthetics, intraocular lenses, equipment or devices which require surgery. These items are covered under
the Surgery benefit.
Hospice Care
To be covered, hospice care must be part of a written plan of care prescribed, periodically reviewed, and
approved by a physician (M.D. or D.O.).
The plan provides benefits for covered services furnished and billed by a hospice that is Medicare-certified or is
licensed or certified by the state it operates in. See the Summary Of Your Costs for limits.
Covered employees of a hospice are a registered nurse; a licensed practical nurse; a licensed physical therapist
or occupational therapist; a certified respiratory therapist; a speech therapist certified by the American Speech,
Language, and Hearing Association; a home health aide directly supervised by one of the above providers
27 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
(performing services prescribed in the plan of care to achieve the desired medical results); and a social work er.
The Hospice Care benefit covers:
• Hospice care for a terminally ill member, for up to 6 months. Benefits may be provided for up to an additional 6
months of care when needed. The initial 6-month period starts on the first day of covered hospice care.
• Palliative care for a member who has a serious or life-threatening condition that is not terminal. Coverage of
palliative care can be extended based on the member's specific condition. Coverage includes expanded
access to home-based care and care coordination.
• End of life counseling provided by the hospice agency. For end of life counseling provided by any other
providers, please see the Mental Health benefit.
Covered services are:
• In-home intermittent hospice visits by one or more of the hospice employees above.
• Respite care to relieve anyone who lives with and cares for the terminally ill member.
• Inpatient hospice care This benefit provides for inpatient services and supplies used while you’re a hospice
inpatient, such as solutions, medications or dressings, when ordered by the attending physician.
• Insulin and Other Hospice Provider Prescribed Drugs Benefits are provided for prescription drugs and
insulin furnished and billed by a hospice.
This benefit doesn’t cover:
• Over-the-counter drugs, solutions and nutritional supplements
• Services provided to someone other than the ill or injured member
• Services of family members or volunteers
• Services, supplies or providers not in the written plan of care or not named as covered in this benefit
• Non-medical services, such as spiritual, bereavement, legal or financial counseling
• Normal living expenses, such as food, clothing, transportation, and household supplies; housekeeping services
other than those of a home health aide as prescribed by the plan of care
For additional information regarding hospice care, please call Customer Service at the number shown on
the back cover of this booklet.
Hospital
This benefit covers:
• Inpatient room and board
• Providers services
• Intensive care or special care units
• Operating rooms, procedure rooms and recovery rooms
• Surgical supplies and anesthesia
• Drugs, blood, medical equipment and oxygen for use in the hospital
• X-ray, lab and testing billed by the hospital
Even though you stay at an in-network hospital, you may get care from doctors or other providers who do not
have a network contract at all. In that case, you will not have to pay any amounts over the allowed amount for
covered services.
You pay out-of-network cost shares if you get care from a provider not in your network. You will not be balanced
billed for certain services provided by a non-participating provider. See How Providers Affect Your Costs for
details.
We must approve all planned inpatient stays before you enter the hospital. See Prior Authorization for details.
This benefit does not cover:
• Hospital stays that are only for testing, unless the tests cannot be done without inpatient hospital facilities, or
your condition makes inpatient care medically necessary
• Any days of inpatient care beyond what is medically necessary to treat the condition
28 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Infusion Therapy
Fluids infused into the vein through a needle or catheter as part of your course of treatment.
Infusion examples include:
• Drug therapy
• Pain management
• Total or partial parenteral nutrition (TPN or PPN)
This benefit covers:
• Outpatient facility and professional services
• Professional services provided in an office or home
• Prescription drugs, supplies and solutions used during infusion therapy
This benefit does not cover over-the-counter:
• Drugs and solutions
• Nutritional supplements
Massage Therapy
Benefits are provided for medically necessary massage therapy received to treat a covered illness, injury or
condition. Benefits must be from a licensed or certified provider performing within the scope of their license or
certification, as allowed by law. Please see the Summary Of Your Costs for benefit limit information.
See the Rehabilitation Therapy benefit for information on coverage of physical and other rehabilitation therapies.
Mastectomy and Breast Reconstruction
Benefits are provided for mastectomy necessary due to disease, illness or injury.
This benefit covers:
• Reconstruction of the breast on which mastectomy was performed
• Surgery and reconstruction of the other breast to produce a similar appearance
• Physical complications of all stages of mastectomy, including lymphedema treatment and supplies
• Inpatient care
Planned hospital admissions require prior authorization, see Prior Authorization for details.
Maternity Care
Benefits for pregnancy and childbirth are provided on the same basis as any other condition for all members.
The Maternity Care benefit includes coverage for abortion.
Facility Care
This benefit covers inpatient hospital, birthing center, outpatient hospital and emergency room services, including
post-delivery care as determined necessary by the attending provider, in consultation with the mother, based on
accepted medical practice.
This benefit also covers medically necessary supplies related to home births.
Professional Care
This benefit covers:
• Prenatal care, including diagnostic and screening procedures, and genetic counseling for prenatal diagnosis of
congenital disorders of the fetus.
• Delivery, including cesarean section, in a medical facility, or delivery in the home
• Postpartum care consistent with accepted medical practice that’s ordered by the attending provider, in
consultation with the mother. Postpartum care includes services of the attending provider, a home health
agency and/or registered nurse.

29 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Note: Attending provider as used in this benefit means a provider such as a physician (M.D. or D.O.), a
physician’s assistant, a certified nurse midwife (C.N.M.), a licensed midwife or an advanced registered nurse
practitioner (A.R.N.P.). If the attending provider bills a global fee that includes prenatal, delivery and/or
postpartum services received on multiple dates of service, this plan will cover those services as it would any other
surgery. See the Surgery benefit for details on surgery coverage.
See the Preventive Care benefit for preventive care during and after pregnancy.
This benefit covers medically necessary donor human milk obtained from a milk bank for inpatient use when
ordered by licensed healthcare provider.
For members residing in states where laws prohibit access to abortion services, travel to a provider in another
state may be covered. See Medical Transportation – State-Restricted Care for details.
Medical Foods
Medical foods are foods that are specially prepared to be consumed or given directly into the stomach by feeding
tube under strict supervision of a doctor. They provide most of a person’s nutrition. They are designed to treat a
specific problem that can be detected using medical tests.
This benefit covers:
• Dietary replacement to treat inborn errors of metabolism (example phenylketonuria (PKU))
• Medically necessary elemental formula for eosinophilic gastrointestinal associated disorder
• Other severe conditions when your body cannot take in nutrient from food in the small intestine (malabsorption)
disorder
• Disorders where you cannot swallow due to a blockage or a muscular problem and need to be fed through a
tube
Medical foods must be prescribed and supervised by doctors or other health care providers.
This benefit does not cover:
• Oral nutrition or supplements not used to treat inborn errors of metabolism or any of the above listed conditions
• Specialized infant formulas
• Lactose-free foods
Medical Transportation
This plan provides benefits for travel and lodging only for certain covered services as described below. Prior
authorization is also required.
• Travel related to the covered transplants named in the Transplants benefit. Benefits are provided for travel of
the member getting the transplant and one companion. The plan also covers lodging for members when the
member is not in the hospital and for their companion. The member getting the transplant must live more than
50 miles from the transplant facility unless treatment protocols require the member to remain closer to the
transplant center.
• Travel for cellular immunotherapy and gene therapy. Benefits are provided for travel for the member and one
companion to a designated provider outside the service area, when a designated provider is not available
within the service area. See Cellular Immunotherapy and Gene Therapy.
See the Summary of Your Costs for any travel benefit limitations.
Benefits are provided for:
• Air transportation expenses between the member’s home and the medical facility where services will be
provided. Air travel expenses cover unrestricted coach class, flexible and fully refundable round-trip airfare from
a licensed commercial carrier.
• Ferry transportation from the member’s home community
• Lodging expenses at commercial establishments, including hotels and motels, between home and the medical
facility where the service will be provided.
• Mileage expenses for the member’s personal automobile
30 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• Ground transportation, car rental, taxicab fares and parking fees, for the member and a companion (when
covered) between the hotel and the medical facility where services will be provided.
Travel and lodging costs are subject to the IRS limits in place on the date you had the expense. The per-day limits
and requirements can change if IRS regulations change. Please go to the IRS website, www.irs.gov, for details.
This summary is not and should not be assumed to be tax advice.
Companion Travel
A companion needed for the member’s health and safety is covered. For a child under age 19 a second
companion is covered only if medically necessary.
Reimbursement of Travel Claims
You must pay for all travel expenses yourself and submit a Claim Reimbursement Form. A separate claim form is
needed for each patient and each commercial carrier or transportation service used. You can get Claim
Reimbursement Forms on our website at www.premera.com/sebb. You can also call us for a copy of the form.
You must attach the following documents to the Claim Reimbursement Form:
• A copy of the detailed itinerary as issued by the transportation carrier, travel agency or online travel website.
The itinerary must identify the names of the passengers, the dates of travel and total cost of travel, and the
origination and final destination points.
• Receipts for all covered travel expenses
Credit card statements or other payment receipts are not acceptable forms of documentation.
This benefit does not cover:
• Charges and fees for booking changes
• Cancellation fees
• First class airline fees
• International travel
• Lodging at any establishment that is not commercial
• Meals
• Personal care items
• Pet care, other than for service animals
• Phone service and long-distance calls
• Reimbursement for mileage rewards or frequent flier coupons
• Reimbursement for travel before contacting us and receiving prior authorization
• Travel for medical procedures not listed above
• Travel in a mobile home, RV, or travel trailer
• Travel to providers outside the network or that have not been designated by Premera to perform the services
• Travel insurance
Medical Transportation – State-Restricted Care
This plan provides benefits for travel and lodging for [abortion] [and] [medically necessary gender affirming care]
services when the member resides in a state where laws restrict access to these covered services. Prior approval
is required. Please call customer service to verify if you are eligible for this benefit and to obtain prior approval.
See the Summary of Your Costs for any travel benefit limitations.
Benefits are provided for:
• Air transportation expenses between the member’s home and the location where services will be provided. Air
travel expenses cover unrestricted coach class, flexible, and fully refundable round-trip airfare from a licensed
commercial carrier.
• Ferry transportation from the member’s home community
• Lodging expenses at commercial establishments, including hotels and motels, between home and the medical
31 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
facility where the service will be provided.
• Mileage expenses for the member’s personal automobile
• Ground transportation, car rental, taxicab fares and parking fees, for the member and a companion (when
covered) between the hotel and the location where services will be provided.
Travel and lodging costs are subject to the IRS limits in place on the date of the expense. The mileage limits and
requirements can change if IRS regulations change. Please go to the IRS website, www.irs.gov, for details. This
summary is not and should not be considered to be tax advice.
Companion Travel
One companion needed for the member’s health and safety is covered only if medically necessary. For medically
necessary care, a second companion is covered for a child under age 19.
Reimbursement of Travel Claims
You must pay for all travel expenses yourself and submit a Claim Reimbursement Form.
A separate Claim Reimbursement Form is needed for each patient and each commercial carrier or transportation
service used. You can get Claim Reimbursement Forms on our website at www.premera.com. You can also call
us for a copy of the form.
You must attach the following documents to the Claim Reimbursement Form:
• A copy of the detailed itinerary as issued by the transportation carrier, travel agency or online travel web site.
The itinerary must identify the names of the passengers, the dates of travel and total cost of travel, and the
origination and final destination points.
• Receipts for all covered travel expenses
Credit card statements or other payment receipts are not acceptable forms of documentation.
This benefit does not cover:
• Charges and fees for booking changes
• Cancellation fees
• First class airline fees
• International travel
• Lodging at any establishment that is not commercial
• Meals
• Personal care items
• Pet care, other than for service animals
• Phone service and long-distance calls
• Reimbursement for mileage rewards or frequent flier coupons
• Reimbursement for travel before contacting us and receiving prior approval
• Travel for medical procedures not listed above
• Travel in a mobile home, RV, or travel trailer
• Travel insurance
• Reimbursement for companion travel and lodging, except for medical necessity or safety of the patient
Mental Health Care
Benefits for mental health services to manage or lessen the effects of a psychiatric condition are provided as
stated below.
Services must be consistent with published practices that are based on evidence when available or follow clinical
guidelines or a consensus of expert opinion published by national mental health professional organizations or
other reputable sources. If no such published practices apply, services must be consistent with community
standards of practice.

32 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Covered mental health services are:
• Inpatient care
• Outpatient therapeutic visits. "Outpatient therapeutic visit" (outpatient visit) means a clinical treatment session
with a mental health provider of a duration consistent with relevant professional standards as defined in the
Current Procedural Terminology manual, published by the American Medical Association. Outpatient
therapeutic visits can include real-time visits via telephone, online chat or text, or other electronic methods with
your doctor or other provider who also maintains a physical location.
• Treatment of eating disorders (such as anorexia nervosa, bulimia or any similar condition)
• Physical, speech or occupational therapy provided for treatment of psychiatric conditions, such as autism
spectrum disorders.
• Applied behavioral analysis (ABA) therapy for members with one of the following:
• Autistic disorder
• Autism spectrum disorder
• Asperger's disorder
• Childhood disintegrative disorder
• Pervasive developmental disorder
• Rett's disorder
Covered ABA therapy includes treatment or direct therapy for identified members and/or family members. Also
covered are an initial evaluation and assessment, treatment review and planning, supervision of therapy
assistants, and communication and coordination with other providers or school staff as needed. Delivery of all
ABA services for a member may be managed by a BCBA or one of the licensed providers below, who is called
a Program Manager. Covered ABA services are limited to activities that are considered to be behavior
assessments or interventions using applied behavioral analysis techniques. ABA therapy must be provided by:
• A licensed physician (M.D. or D.O.) who is a psychiatrist, developmental pediatrician or pediatric neurologist
• A licensed psychiatric nurse practitioner (NP), advanced nurse practitioner (ANP) or advanced registered
nurse practitioner (ARNP)
• A licensed occupational or speech therapist
• A licensed psychologist (Ph.D.)
• A licensed community mental health agency or behavioral health agency that is also state-certified to provide
ABA therapy.
• A Board-Certified Behavior Analyst (BCBA). This means a provider who is state-licensed if the State
licenses behavior analysts (Washington does). If the state does not require a license, the provider must be
certified by the Behavior Analyst Certification Board. BCBAs are only covered for ABA therapy that is within
the scope of their license or board certification.
• A therapy assistant/behavioral technician/paraprofessional, when their services are supervised and billed by
a licensed provider or a BCBA.
Mental health services other than ABA therapy must be furnished by one of the following types of providers to be
covered:
• Hospital
• State-Licensed Community Mental Health Agency
• Licensed physician (M.D. or D.O.)
• Licensed psychologist (Ph.D.)
• A state hospital operated and maintained by the state of Washington for the care of the mentally ill
• Any other provider listed under the definition of “provider” (see the Definitions section in this booklet) who is
licensed or certified by the state in which the care is provided, and who is providing care within the scope of
their license.
• Behavioral health facilities that are accredited by the Joint Commission, the Commission on Accreditation of
Rehabilitation Facilities (CARF), or the Council on Accreditation (COA), only when the state does not require
licensure for the specific level of care.
33 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• Washington state-licensed Behavioral Health Agency
When medically appropriate, services may be provided in your home.
For psychological and neuropsychological testing and evaluation benefit information, see the Psychological and
Neuropsychological Testing benefit.
For substance use disorder benefit information, see the Substance Use Disorder benefit.
For prescription drug benefit information, see the Prescription Drug benefit.
The Mental Health Care benefit doesn’t cover:
• Psychological treatment of sexual dysfunctions
• Outward bound, wilderness, camping or tall ship programs or activities
• Mental health evaluations for purposes other than evaluating the presence of or planning treatment for covered
mental health disorders, including, but not limited to, custody evaluations, competency evaluation, forensic
evaluations, vocational, educational or academic placement evaluations.
Neurodevelopmental Therapy (Habilitation)
Benefits are provided for the treatment of neurodevelopmental disabilities. The following inpatient and outpatient
neurodevelopmental therapy services must be medically necessary to restore and improve function, or to
maintain function where significant physical deterioration would occur without the therapy. This benefit includes
physical, speech, and occupational therapy assessments and evaluations related to treatment of covered
neurodevelopmental therapy.
Physical, speech and occupational therapy provided for treatment of psychiatric conditions, such as autism
spectrum disorders, are covered under the Mental Health Care benefit.
Inpatient Care Inpatient facility services must be furnished and billed by a hospital or by a rehabilitation facility
that meets our clinical standards and will only be covered when services can’t be done in a less intensive setting.
Outpatient Care Benefits for outpatient physical, speech and occupational therapy are subject to all of the
following provisions:
• The member must not be confined in a hospital or other medical facility
• Services must be furnished and billed by a hospital, rehabilitation facility that meets our clinical standards,
physician, physical, occupational or speech therapist, chiropractor, massage practitioner or naturopath
A “visit” is a session of treatment for each type of therapy. Each type of therapy combined accrues toward the
visit maximum described in the Summary Of Your Costs. Multiple therapy sessions on the same day will be
counted as one visit, unless provided by different health care providers.
The plan won’t provide this benefit and the Rehabilitation Therapy benefit for the same condition. Once a
calendar year maximum has been exhausted under one of these benefits, no further coverage is available.
For massage therapy coverage, please see the Massage Therapy benefit.
This benefit doesn’t cover:
• Recreational, vocational, or educational therapy; exercise or maintenance-level programs
• Social or cultural therapy
• Treatment that isn’t actively engaged in by the ill, injured or impaired member
• Gym or swim therapy
• Custodial care
Newborn Care
Newborn children are covered automatically for the first 3 weeks from birth when the mother is eligible to receive
obstetrical care benefits under this plan. To continue benefits beyond the 3-week period, see the dependent
eligibility and enrollment guidelines outlined in the Medical Plan Eligibility And Enrollment section.
If the mother isn’t eligible to receive obstetrical care benefits under this plan, the newborn isn’t automatically
covered for the first 3 weeks. For newborn enrollment information, see the Medical Plan Eligibility And
Enrollment section.
34 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
You must add your newly adopted child to your health plan for enrollment in this plan. This is not automatic. If
adding the child increases the premium, the required forms must be received no later than 60 days after the date
of the birth, adoption, or the date the legal obligation is assumed for total or partial support in anticipation of
adoption. See the Medical Plan Eligibility And Enrollment section.
Benefits are provided on the same basis as any other care, subject to the child's own cost shares, if any, and
other provisions as specified in this plan. Services must be consistent with accepted medical practice and
ordered by the attending provider in consultation with the mother.
Hospital Care
The Newborn Care benefit covers hospital nursery care as determined necessary by the attending provider, in
consultation with the mother, based on accepted medical practice. Also covered are any required readmissions
to a hospital and outpatient or emergency room services for medically necessary treatment of an illness or injury.
Professional Care
Benefits for services received in a provider’s office are subject to the terms of the Professional Visits And
Services benefit. Well-baby exams in the provider's office are covered under the Preventive Care benefit. This
benefit covers:
• Inpatient newborn care, including newborn exams
• Follow-up care consistent with accepted medical practice that’s ordered by the attending provider, in
consultation with the mother. Follow-up care includes services of the attending provider, a home health agency
and/or a registered nurse.
• Circumcision
Note: Attending provider as used in this benefit means a provider such as a physician (MD or DO), a physician’s
assistant, a certified nurse midwife (CNM), a licensed midwife or an advanced registered nurse practitioner
(ARNP).
This benefit doesn’t cover immunizations and outpatient well-baby exams. See the Preventive Care
benefit for coverage of immunizations and outpatient well-baby exams.
Orthognathic Surgery (Jaw Augmentation Or Reduction)
When medical necessity criteria are met, benefits for procedures to lengthen or shorten the jaw (orthognathic
surgery) are provided. Covered orthognathic services include surgery for repair of a dependent child's congenital
(apparent at birth) deformities determined to be medically necessary. These procedures are not covered under
other benefits of this plan.
Prescription Drug
What’s Covered
This benefit only covers drugs that are approved by the US Food and Drug Administration (FDA) that you get from
a licensed pharmacy for take-home use. Covered drugs include the drugs and items listed below. All drugs and
other items must be medically necessary.
Essentials Drug List This plan uses a specific list of covered drugs, sometimes referred to as a “formulary.”
This list, called the Essentials drug list, includes preferred generic drugs, preferred brand-name drugs and non-
preferred drugs. However, the Essentials drug list does not cover some of the drugs in certain drug classes. An
example is proton pump inhibitors. Except for drugs and items listed under Exclusions below in this benefit, the
Essentials drug list covers at least 1 drug in every drug class. (A drug class is a group of drugs that may work in
the same way, have a similar chemical structure, or may be used to treat the same conditions or group of
conditions.)
Drugs not included in the Essentials drug list are not covered by this plan.
Please call customer service or visit our website for more information or to find out if a certain drug is covered. If
your drug is not covered, please work with your provider to find an alternative drug in that drug class that the plan
does cover.
See Question 1 in Questions And Answers About Your Pharmacy Benefits below in this benefit to find out
how to ask for coverage of a drug that is not in the Essentials drug list.

35 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Diabetic Drugs
Shots You Give Yourself
• Prescribed drugs for shots that you give yourself, such as insulin
• Needles, syringes, alcohol swabs, test strips, testing agents and lancets.
Nicotine Habit-Breaking Drugs Prescription brand and generic drugs to help you break a nicotine habit.
Generic over-the-counter drugs are also covered.
Oral Chemotherapy This benefit covers drugs you can take by mouth that can be used to kill cancer cells or slow
their growth. This benefit only covers the drugs that you get from a pharmacy.
Glucagon and Allergy Emergency Kits
Prescription Vitamins
Specialty drugs These drugs treat complex or rare health problems. An example is rheumatoid arthritis.
Specialty drugs also need special handling, storage, administration or patient monitoring. They are high cost and
can be shots you give yourself.
Human growth hormone Human growth hormone is covered only for medical conditions that affect growth. It is
not covered when the cause of short stature is unknown. Human growth hormone is a specialty drug. It is not
covered under other benefits of this plan.
Contraceptives
All FDA-approved prescription and over-the-counter oral contraceptive drugs, supplies and devices. See
Prescription Drug in the Summary Of Your Costs. You must buy over-the-counter supplies and devices at the
pharmacy counter. For details on how to submit a claim, see the How Do I File a Claim? section. For shots or
devices from your provider, see Preventive Care.
Preventive Drugs Required By The Affordable Care Act hat your provider prescribes. Some preventive drugs
have limits on how often you and/or who should get them. The limits are often based on your age or gender. After
one of these limits is reached, these drugs are not covered in full and you may have to pay more out-of-pocket
costs.
Off-Label Uses The US Food and Drug Administration (FDA) approves prescription drugs for specific health
conditions or symptoms. Some drugs are prescribed for uses other than those the FDA has approved. The plan
covers such drugs if the use is recognized as effective in standard drug reference guides put out by the American
Hospital Formulary Service, the American Medical Association, the US Pharmacopoeia, or other reference guides
also recognized by the Federal Secretary of the US Health and Human Services department or the Insurance
Commissioner.
Drug uses that are not recognized by one of the above standard drug reference guides can be covered if they are
recognized by the Secretary of the US Health and Human Services department or by the majority of relevant,
peer-reviewed medical literature. For more details, see the definition of “prescription drug” in the Definitions
section of this booklet.
Compound Medications To be covered, these must contain at least one covered prescription drug
GETTING PRESCRIPTIONS FILLED
It is always a good idea to show your Premera Blue Cross ID card when you go to the pharmacy.
See question 6 of Questions And Answers About Your Pharmacy Benefits for exceptions to the
supply limits shown in this table.
Pharmacy
Supply Limit
Instructions
In-Network Retail or
In-Network Specialty
Pharmacies
30 days
Pay the cost share in the Summary Of Your Costs at the
pharmacy
Out-Of-Network
Retail Pharmacies
30 days
• Pay the full cost of the drug at the pharmacy.
• Send Premera a claim. See How Do I File A Claim? in
this booklet for instructions.

36 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
In-Network Mail-
Order Pharmacy
(Out-of-network
mail-order
pharmacies are not
covered)
90 days
• Allow 2 weeks for your prescription to be filled.
• Ask your provider to prescribe up to a 90-day supply of the
drug you need.
• Send your prescriptions and a pharmacy mail-order form to
the mail-order pharmacy. You can download the form from
our website or call us for a copy. Our website and phone
numbers are on the back cover of this booklet.
Exclusions
This benefit does not cover:
• Over-the-counter drugs and supplies, even if you have a prescription, that are not listed as covered above. For
example, the plan does not cover vitamins, food and dietary supplements (such as baby formula or protein
powder), or herbal or naturopathic medicines.
• Drugs used to improve your looks, such as drugs to increase hair growth
• Drugs for experimental or investigational use. (See Definitions.)
• Blood or blood derivatives. See the Blood Products And Services benefit for coverage.
• More refills than the number prescribed, or any refill dispensed more than one year after the prescriber's
original order
• Drugs for use while you are in a health care facility or provider’s office, or take-home drugs dispensed and
billed by a health care facility. The exceptions are for specialty drugs.
• Replacement of lost or stolen items
• Solutions and drugs that you get through a shot or through an intravenous needle, a catheter or a feeding tube.
(The exception is a shot you give yourself.) See the Infusion Therapy benefit.
• Drugs to treat sexual dysfunction
• Drugs to manage your weight
• Medical equipment and supplies that are not listed as covered above. See the Home Medical Equipment
(HME), Orthotics, Prosthetics And Supplies benefit for coverage.
• Immunization agents and vaccines. See the Preventive Care benefit.
• Drugs for fertility treatment or assisted reproduction procedures.
Your Prescription Drug Rights
You have the right to safe and effective pharmacy services. You also have the right to know what drugs are
covered under your plan and the limits that apply. If you have a question or concern about your prescription drug
benefits, please contact us (the health carrier) at the customer service phone number shown on the back cover of
this booklet or visit our website at www.premera.com/sebb. If you would like to know more about your rights, or
if you have concerns about your plan, you may contact the Washington State Office of Insurance Commissioner
at 1-800-562-6900 or www.insurance.wa.gov. If you have a concern about the pharmacists or pharmacies
serving you, please contact the Washington State Department of Health at 360-236-4700 www.doh.wa.gov, or
HSQACS@doh.wa.gov.
Questions and Answers About Your Pharmacy Benefits
1. Does this plan exclude certain drugs my health care provider may prescribe, or encourage
substitution for some drugs?
Essentials Drug List
This benefit makes use of our Essentials drug list, sometimes referred to as a “formulary.”
Our Pharmacy and Therapeutics Committee makes the decisions about the drug list. This committee
includes doctors and pharmacists from the community. The committee review medical studies, scientific
papers and reports and other information on drugs and their uses to choose safe and effective drugs for the
list.
The Essentials drug list includes preferred generic drugs, preferred brand name drugs, preferred specialty
drugs, and certain non-preferred generic, brand name and specialty drugs. (Preferred brand name drugs are
brand name drugs that are only made by one drug company.) The Essentials drug list covers at least 1 drug
37 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
in every drug class but does not cover all the drugs in some drug classes. Use the RX Search tool on our
website or call customer service for a full list of drugs on the Essentials drug list.
This plan also doesn’t cover certain categories of drugs. These are listed under Exclusions earlier in this
benefit.
Certain drugs need prior authorization. See Prior Authorization for more detail.
Generic Drug Substitution
This plan encourages the use of appropriate generic drugs (as defined below). When available and
indicated by the prescriber, a generic drug will be dispensed in place of a brand name drug. If your
prescriber does not want to substitute a generic for the brand name drug, you pay only the applicable brand
name cost shares. See the Summary Of Your Costs for the amount you pay. However, if the prescriber
allows you to take the generic drug instead of the brand-name drug, and you buy the brand name drug
anyway, you will have to pay the difference in price between the brand name drug and the generic equivalent
along with the applicable brand name cost-share. Please ask your pharmacist about the higher costs you
will pay if you select a brand name drug. Important note: If the generic drug is not effective, you may
request a review for medical necessity and consideration to waive the difference in cost between the brand
name drug and the generic equivalent. You will still be responsible for paying the applicable brand name
drug cost-share.
A “generic drug” is a prescription drug manufactured and distributed after the brand name drug patent of the
innovator company has expired. Generic drugs have obtained an AB rating from the U.S. Food and Drug
Administration (FDA). The FDA considers them to be therapeutically equivalent to the brand name product.
For the purposes of this plan, classification of a particular drug as a generic is based on generic product
availability and cost as compared to the reference brand name drug.
This benefit also covers “biological products.” Examples are serums and antitoxins. Generic substitution
does not apply to biological products.
Exceptions You or your provider may ask that the plan cover a drug or a dose that is not on the Essentials
drug list. The drug may be covered if 1 of 3 things is true:
• You cannot tolerate the drugs that are on the Essentials drug list
• All covered drugs in any tier of the Essentials drug list will be (or have been) either ineffective or not as
effective as the drug that is not on the list
• The dosage you need is not available in the drugs on the Essentials drug list.
If your request to cover a drug not on the Essentials drug list is approved, the plan will cover the drug. If your
request is not approved, the plan will not cover the drug.
Exception Process The request can be made in writing, electronically or by phone. Your provider must give
us a written or oral statement that confirms the need for the requested drug to treat your condition and states
that the criteria above are met. We have the right to ask for medical records that relate to the request.
Within 5 calendar days after we get the information we need from your provider, we will let you or your
provider know in writing if your request is approved.
If Your Request Is Urgent We will respond to your request within 48 hours after we get the information we
need from your provider if 1 of the following is true:
• Your health problem may put your life or health in serious danger.
• You have already started taking the drug.
The provider must confirm that 1 of the 2 situations above is true. The provider must also explain the harm
that would come to you if we did not respond to the request within 48 hours.
2. When can my plan change the pharmacy drug list? If a change occurs, will I have to pay more to use
a drug I had been using?
Our Pharmacy and Therapeutics Committee reviews the pharmacy drug list frequently throughout the year.
It can decide to make a drug preferred or non-preferred at any point in the year. The committee may also
add or remove a drug from the Essentials drug list during the year. These changes can happen if new drugs
appear on the market or new medical studies or other clinical information warrant the change.
If you’re taking a drug that’s changed from preferred to non-preferred status, we’ll notify you before the
change. We will also tell you if a drug you are taking is going to be removed from the Essentials drug list.
The amount you pay for a drug is based on whether the generic, brand name or specialty drug is preferred or
38 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
non-preferred on the date it is dispensed. Whether the pharmacy is in the network or not on the date the
drug is dispensed is also a factor.
3. What should I do if I want a change from limitations, exclusions, substitutions or cost increases for
drugs specified in this plan?
The limitations and exclusions applicable to your prescription drug benefit, including categories of drugs for
which no benefits are provided, are part of this plan’s overall benefit design, and can’t be changed. The
plan's rules about substitution of generic drugs are described above in question 1.
You can appeal any decision you disagree with. See the Complaints And Appeals section in this booklet,
or call our customer service department at the telephone numbers listed on the back cover of this booklet for
information on how to initiate an appeal.
4. How much do I have to pay to get a prescription filled?
You will find the amounts you pay for covered drugs in the Summary Of Your Costs.
5. Do I have to use certain pharmacies to pay the least out of my own pocket under this plan?
Yes. You receive the highest level of benefits when you have your prescriptions filled by in-network
pharmacies. The majority of retail pharmacies in Washington are part of our pharmacy network. Your
benefit covers prescription drugs dispensed from an out-of-network pharmacy, but at a higher out-of-pocket
cost to you as explained above.
Our mail order program offers lower cost shares and lets you buy larger supplies of your medications, but
you must use our in-network mail order pharmacy.
You can find an in-network pharmacy near you by consulting your provider directory, or calling the Pharmacy
Locator Line at the toll-free telephone number found on the back of your ID card.
Specialty drugs are covered only when you get them from specialty pharmacies. Specialty pharmacies are
pharmacies that focus on the delivery and clinical management of specialty drugs. See the Summary Of
Your Costs for more information.
6. How many days’ supply of most medications can I get without paying another copay or other
repeating charge?
The dispensing limits (or days’ supply) for drugs dispensed at retail pharmacies and through the mail-order
pharmacy benefit are described in the Getting Prescriptions Filled table above.
Benefits for refills will be provided only when you have used 75% of a supply of a single medication. The
75% is calculated based on both of the following:
• The number of units and days' supply dispensed on the last refill
• The total units or days' supply dispensed for the same medication in the 180 days immediately before the
last refill. This rule does not apply when the member has purchased more than a 180-day supply of
contraceptive drugs at one time.
Exceptions to the supply limit are allowed as required by law:
• A pharmacist can approve an early refill of a prescription for eye drops or eye ointment in some cases. If
you must pay a copay for the drug, the full copay is required for the early refill.
• A different supply can be allowed so that a new drug can be refilled at the same time as drugs that you are
already taking. We will pro-rate the cost shares to the exact number of days early that the refill is
dispensed. For example, a drug with a $10 copay for a 30-day supply would have a per-day copay of 33
cents. If the member needed a 20-day supply of the drug, we would then multiply the 33 cents by 20.
• You can ask for up to a 12-month supply of contraceptive drugs. If you have a copay for the drug, you
must pay one copay for each 30-day supply from a retail pharmacy or one copay for each 90-day supply
from the in-network mail-order pharmacy.
The plan can also cover more than the 30-day or 90-day supply limit if the drug maker’s packaging does not
let the exact amount be dispensed. If you must pay a copay for the drug, you pay one copay for each 30-day
supply from a retail pharmacy or one copay for each 90-day supply from the in-network mail-order pharmacy.
7. What other pharmacy services does my health plan cover?
This benefit is limited to covered prescription drugs and specified supplies and devices dispensed by a
licensed pharmacy. Other services, such as consultations with a pharmacist, diabetic education or medical
equipment, are covered by the medical benefits of this plan, and are described elsewhere in this booklet.
39 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Drug Discount Programs
Premera Blue Cross may receive rebates from its pharmacy benefit manager or other vendors. Such rebates are
Premera Blue Cross's property. These rebates are retained by Premera Blue Cross and may be taken into
account in setting subscription charges or may be credited to administrative charges and are not reflected in your
allowed amount. The allowed amount is not adjusted to reflect rebates received as part of Drug Discount
Programs.
In addition, the allowed amount that your payment for drugs is based on may be higher than the price Premera
Blue Cross pays its pharmacy benefit manager or other vendors for those drugs. The difference constitutes
Premera Blue Cross property. Premera Blue Cross is entitled to retain and shall retain the difference and may
apply it to the cost of Premera Blue Cross's operations. If your drug benefit includes a copay, coinsurance
calculated on a percentage basis, or a deductible, the amount you pay and yo ur account calculations are based
on the allowed amount. The allowed amount is not adjusted to reflect discounts received as part of Drug Discount
Programs.
Preventive Care
This plan pays for preventive care as shown in the Summary Of Your Costs. Below is a summary of preventive
care services.
Preventive Exams
• Routine adult and well-child exams. Includes exams for school, sports and jobs
• Review of oral health for members under 19
• Vision screening for members under 19
• Depression screening
Immunizations
• Shots in a provider’s office
• Flu shots, nasal spray flu vaccine (FluMist), whooping cough and other seasonal shots at a pharmacy or
other community center
• Shots needed for foreign travel at the county health department or a travel clinic
Screening Tests
Routine lab tests and imaging, this includes women’s preventive services as recommended by the HRSA
women’s preventive services guidelines and others such as:
• Mammograms (includes 3D mammograms)
• X-rays
• Pap smears
• Prostate-specific antigen tests
• BRCA genetic tests for members at risk for certain breast cancers.
Pregnant Member’s Care
• Breastfeeding support and counseling
• Purchase of standard electric breast pumps
• Rental of hospital-grade breast pumps if medically necessary
• Screening for postpartum depression
Colorectal Cancer Screening
For members who are 50 or older or who are under age 50 and at high risk for colo rectal cancer. Includes:
• Barium enema
• Colonoscopy, sigmoidoscopy, fecal immunochemical test (FIT) and fecal occult blood tests. The plan also
covers a consultation before the colonoscopy and anesthesia your doctor thinks is medically necessary.
• If polyps are found during a screening procedure, removing them and lab tests on them are also covered as
preventive.
40 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• Colonoscopies as follow-up to positive non-invasive stool based screening tests.
Diabetes Preventive Program
• Weight Management Programs consisting of 31 lessons over a 12 month timeframe provided to non-
Medicare members who are age eighteen (18) and older and have a BMI>25.
Eligibility for the weight management programs is based on medication claims for:
• Metformin only (no additional diabetes medications); or
• Blood pressure medication and a cholesterol medication; or
• Any weight loss medication
Members are not eligible if they are pregnant or are diagnosed with diabetes mellitus.
Please see the Chronic Condition Management for additional diabetes benefit information.
Diabetes Screening
Health Education and Training
Outpatient programs and classes to help you manage pain or cope with covered conditions like heart disease,
diabetes, or asthma. The program or class must have our approval.
Nicotine Habit-Breaking Programs
Programs to stop smoking, chewing tobacco or taking snuff. Information regarding available nicotine habit-
breaking programs can be obtained by contacting your provider.
Nutritional Counseling and Therapy
Office visits to discuss a healthy diet and eating habits and help you manage weight. The plan covers
screening and counseling for:
• Members at risk for health conditions that are affected by diet and nutrition
• Weight loss for children age 6 and older who are considered obese and for adults with a body mass index
of 30 kg/meter squared or higher. This includes intensive behavioral interventions with more than one
type of activity to help you set and achieve weight loss goals.
Fall Prevention
Risk assessments and advice on how to prevent falls for members who are age 65 or older and have a history
of falling or have mobility issues
Pre-exposure (PrEP) for members at high risk for HIV infection.
Contraceptive
• Birth control devices, shots and implants. The plan will cover up to a 12-month supply of contraceptive pills.
See Prescription Drug for coverage of prescription and over-the-counter drugs and devices.
• Emergency contraceptives (“plan B”)
• Tubal ligation. When tubal ligation is done as a secondary procedure, only the charge for the procedure
itself is covered under this benefit. The related services, such as anesthesia, are covered as part of the
primary procedure. See Hospital and Surgery.
About Preventive Care
Preventive care is a set of evidence-based services. These services are based on guidelines required under
state or federal law. The guidelines come from:
• Services that the United States Preventive Services Task Force (USPSTF) has given an A or B rating
• Immunizations that the Centers for Disease Control and Prevention recommends
• Screening and other care for women, babies, children and teens that the Health Resources and Services
Administration recommends.
• Services that meet the standards in Washington state law.
Please go to this government website for more information:
https://www.healthcare.gov/coverage/preventive-care-benefits/
41 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
The agencies above may also change their guidelines from time to time. If this happens, the plan will comply with
the changes.
Some preventive services and tests have limits on how often you should get them. The limits are often based on
your age or gender. For some services, the number of visits covered as preventive depends on your medical
needs. After one of these limits is reached, these services are not covered in full and you may have to pay more
out-of-pocket costs.
Some of the covered services your provider does during a routine exam may not be preventive at all. The plan
would cover them under other benefits. They would not be covered in full.
For example:
During your preventive exam, your provider may find a problem that needs further tests or screening for a proper
diagnosis to be made. Or, if you have a chronic disease, your provider may check your condition with tests.
These types of tests help to diagnose or monitor your illness and would not be covered under the Preventive
Care benefit. You would have to pay the cost share under the plan benefit that covers the service or test.
The Preventive Care benefit does not cover:
• Take-home drugs or over-the-counter items. See Prescription Drug.
• Routine newborn exams while the child is in the hospital after birth. See Newborn Care.
• Routine or other dental care
• Services related to tubal ligation when it is done as a secondary procedure. The charge for the procedure itself
is covered under this benefit, but the related services, such as anesthesia, are covered as part of the primary
procedure. See the Hospital and Surgery benefits.
• Routine vision and hearing exams
• Gym fees or exercise classes or programs
• Services or tests for a specific illness, injury or set of symptoms. Please see the plan's other benefits.
• Physical exams for basic life or disability insurance
• Work-related disability or medical disability exams
• Purchase of hospital-grade breast pumps
• Vasectomy. See Surgery.
For additional information regarding preventive care services or programs above, please call Customer
Service at the number shown on the back cover of this booklet.
Professional Visits And Services
Benefits are provided for the examination, diagnosis and treatment of an illness or injury when such services are
performed on an inpatient or outpatient basis, including your home. Benefits are also provided for the following
professional services when provided by a qualified provider:
• Second opinions for any covered medical diagnosis or treatment plan
• Biofeedback for migraines and other conditions for which biofeedback is not deemed experimental or
investigational (see Definitions)
• Repair of a dependent child’s congenital anomaly
• Consultations with a pharmacist
• Real-time visits via online and telephonic methods with your doctor or other provider who also maintains a
physical location
For surgical procedures performed in a provider’s office, surgical suite or other facility benefit information, see the
Surgery benefit.
For professional diagnostic services benefit information, see the Diagnostic X-Ray, Lab And Imaging benefit.
For home health or hospice care benefit information, see the Home Health Care and Hospice Care benefits.
For preventive or routine services, see the Preventive Care benefit.
For diagnosis and treatment of psychiatric conditions benefit information, see the Mental Health Care benefit.
42 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
For diagnosis and treatment of temporomandibular joint (TMJ) disorders benefit information, please see the
Temporomandibular Joint Disorders (TMJ) Care benefit.
Electronic Visits
This benefit will cover electronic visits (e-visits) from in-network providers when all the requirements below are
met. This benefit is only provided when three things are true:
• Premera Blue Cross has approved the physician for e-visits. Not all physicians have agreed to or have the
software capabilities to provide e-visits.
• The member has previously been treated in the approved physician's office and has established a patient -
physician relationship with that physician.
• The e-visit is medically necessary for a covered illness or injury.
An e-visit is a structured, secure online consultation between the approved physician and the member. Each
approved physician will determine which conditions and circumstances are appropriate for e-visits in their
practice.
Please call customer service at the number shown on the back cover of this booklet for help in finding a physician
approved to provide e-visits.
The Professional Visits And Services benefit doesn't cover:
• Hair analysis or non-prescription drugs or medicines, such as herbal, naturopathic or homeopathic medicines or
devices
• EEG biofeedback or neurofeedback services
• Rehabilitation that is not part of a cardiac or pulmonary rehabilitation program. Please see Rehabilitation
Therapy.
Psychological and Neuropsychological Testing
Covered services are psychological and neuropsychological testing, including interpretation and report
preparation, necessary to prescribe an appropriate treatment plan. This includes later re-testing to make sure the
treatment is achieving the desired medical results. Physical, speech or occupational therapy assessments and
evaluations for rehabilitation are provided under the Rehabilitation Therapy benefit.
See the Neurodevelopmental (Habilitation) Therapy benefit for physical, speech or occupational therapy
assessments and evaluations related to neurodevelopmental disabilities.
Rehabilitation Therapy
This plan covers rehabilitation therapy. Benefits must be provided by a licensed physical therapist, occupational
therapist, speech language pathologist or a licensed qualified provider.
Rehabilitation therapy is therapy that helps get a part of the body back to normal health or function. It includes
therapy to 1) restore or improve a function that was lost because of an accidental injury, illness or surgery; or 2) to
treat disorders caused by a physical congenital anomaly.
Services provided for treatment of a mental health condition are provided under the Mental Health Care benefit.
Cardiac rehabilitation, pulmonary rehabilitation and chronic pain care are covered as any other medical condition
and do not accrue to rehabilitation therapy limits.
Limits listed in the Summary Of Your Costs do not apply to rehabilitation related to treatment of cancer, such as
for breast cancer rehabilitation therapy.
Inpatient Care
Inpatient rehabilitation care is covered when medically necessary and provided in a specialized inpatient
rehabilitation center, which may be part of a hospital. If you are already an inpatient, this benefit will start when
your care becomes mainly rehabilitative and you are transferred to an inpatient rehabilitation center. This benefit
only covers care you receive within 24 months from the onset of the injury or illness or from the date of the
surgery that made rehabilitation necessary.
43 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
You must get prior authorization from us before you get treatment in an inpatient rehabilitation center. See Prior
Authorization for details.
Outpatient Care
This benefit covers the following types of medically necessary outpatient therapy:
• Physical, speech, hearing and occupational therapies. Physical, speech, and occupational assessments and
evaluations related to rehabilitation are also covered.
• Cochlear implants
• Home medical equipment, medical supplies and devices
This benefit does not cover:
• Treatment that the ill, injured or impaired member does not actively take part in.
• Inpatient rehabilitation received more than 24 months from the date of onset of the member’s injury or illness or
from the date of the member’s surgery that made the rehabilitation necessary.
• Therapy for flat feet except to help you recover from surgery to correct flat feet.
Skilled Nursing Facility Care
This benefit includes:
• Room and board
• Skilled nursing services
• Supplies and drugs
• Skilled nursing care during some stages of recovery
• Skilled rehabilitation provided by physical, occupational or speech therapists while in a skilled nursing facility
• Short or long term stay immediately following a hospitalization
• Active supervision by your provider while in the skilled nursing facility
We must approve all planned skilled nursing facility stays before you enter a skilled nursing facility. See Prior
Authorization for details.
This benefit does not cover:
• Acute nursing care
• Skilled nursing facility stay not immediately following hospitalization or inpatient stay
• Skilled nursing care outside of a hospital or skilled nursing facility
• Care or stay provided at a facility that is not qualified per our standards
Spinal and Other Manipulations
This benefit covers medically necessary manipulations to treat a covered illness, injury or condition.
Rehabilitation therapy, such as massage or physical therapy, provided with manipulations is covered under the
Massage Therapy, Rehabilitation Therapy and Neurodevelopmental (Habilitation) Therapy benefits.
See the Summary of Your Costs for benefit limitations.
Substance Use Disorder
This benefit covers inpatient and outpatient substance use disorder conditions treatment and supporting services.
Covered services include services provided by a state-approved treatment program or other licensed or certified
provider. Covered outpatient visits can include real-time visits via telephone, online chat or text, or other electronic
methods with your doctor or other provider who also maintains a physical location.
The current edition of the Patient Placement Criteria for the Treatment of Substance Related Disorders as
published by the American Society of Addiction Medicine is used to determine if substance use disorder
conditions treatment is medically necessary.
Note: Medically necessary detoxification is covered in any medically necessary setting. Detoxification in the
hospital is covered under the Emergency Room and Hospital benefits. Acupuncture services when provided for
44 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
substance use disorder conditions do not apply to the Acupuncture benefit visit limits .
The Substance Use Disorder benefit doesn’t cover:
• Halfway houses, quarterway houses, recovery houses, and other sober living residences
Surgery
This benefit covers surgical services (including injections) that are not named as covered under other benefits,
when performed on an inpatient or outpatient basis, in such locations as a hospital, ambulatory surgical facility,
surgical suite or provider’s office. Also covered under this benefit are:
• Anesthesia or sedation and postoperative care as medically necessary.
• Cornea transplantation, skin grafts, repair of a dependent child’s congenital anomaly, and the transfusion of
blood or blood derivatives.
• Colonoscopy and other scope insertion procedures are also covered under this benefit unless they qualify as
preventive services as described in the Preventive Care benefit.
• Surgery that is medically necessary to correct the cause of infertility. This does not include assisted
reproduction techniques or sterilization reversal.
• Repair of a defect that is the direct result of an injury, providing such repair is started within 12 months of the
date of the injury.
• Correction of functional disorders upon our review and approval.
For organ, bone marrow or stem cell transplant procedure benefit information, see the Transplants benefit.
For services to change gender, see the Gender Affirming Care benefit.
For members residing in states where laws prohibit access to medically necessary gender affirming care, travel to
a provider in another state may be covered. See Medical Transportation – State-Restricted Care for details.
This benefit does not cover removal of excess skin or fat related to either weight loss surgery or the use of drugs
for weight loss.
Surgical Center Care – Outpatient
Benefits are provided for services and supplies furnished by an outpatient surgical center.
Temporomandibular Joint Disorders (TMJ) Care
TMJ disorders are covered on the same basis as any other condition.
TMJ disorders include those conditions that have some of the following symptoms:
• Muscle pain linked with TMJ
• Headaches linked with the TMJ
• Arthritic problems linked with the TMJ
• Clicking or locking in the jawbone joint
• An abnormal range of motion or limited motion of the jawbone joint
This benefit covers:
• Exams
• Consultations
• Treatment
Some services may be covered under other benefits sections of this plan with different or additional cost share,
such as:
• X-rays. See Diagnostic X-Ray, Lab And Imaging
• Surgery. See Surgery
• Hospital. See Hospital
Some surgeries need to be pre-approved before you get them. See Prior Authorization for details.
45 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
“Medical Services” for the purpose of this TMJ benefit are those that meet all of the following requirements:
• Reasonable and appropriate for the treatment of a disorder of the temporomandibular joint, under all the factual
circumstances of the case
• Effective for the control or elimination of one or more of the following, caused by a disorder of the
temporomandibular joint: pain, infection, disease, difficulty in speaking, or difficulty in chewing or swallowing
food
• Recognized as effective, according to the professional standards of good medical practice
• Not experimental or investigational, according to the criteria stated under the "Definitions" section, or primarily
for cosmetic purposes
Therapeutic Injections
This benefit covers:
• Shots given in the provider’s office
• Supplies used during the visit, such as serums, needles and syringes
• Three teaching doses for self-injectable specialty drugs
This benefit does not cover:
• Immunizations. See Preventive Care)
• Self-injectable drugs. See Prescription Drug)
• Infusion therapy. See Infusion Therapy)
• Allergy shots. See Allergy Testing and Treatment)
Transplants
The Transplants benefit is not subject to a separate benefit maximum other than the maximum for travel and
lodging described below. This benefit covers medical services only if provided by in-network providers or
“Approved Transplant Centers.” See the transplant benefit requirements later in this benefit for more information
about approved transplant centers.
Covered Transplants
Organ transplants and bone marrow/stem cell reinfusion procedures must not be considered experimental or
investigational for the treatment of your condition. See the Definitions section in this booklet for the definition of
“experimental/investigational services.” We reserve the right to base coverage on all of the following:
• Organ transplants and bone marrow/stem cell reinfusion procedures must meet our criteria for coverage. We
review the medical indications for the transplant, documented effectiveness of the procedure to treat the
condition, and failure of medical alternatives.
The types of organ transplants and bone marrow/stem cell reinfusion procedures that currently meet our criteria
for coverage are:
• Heart
• Heart/double lung
• Single lung
• Double lung
• Liver
• Kidney
• Pancreas
• Pancreas with kidney
• Bone marrow (autologous and allogeneic)
• Stem cell (autologous and allogeneic)
Note: For the purposes of this plan, the term “transplant” doesn't include cornea transplantation, skin grafts or
the transplant of blood or blood derivatives other than bone marrow or stem cells. These procedures are
covered on the same basis as any other covered surgical procedure. See the Surgery benefit.
• Your medical condition must meet our written standards.
46 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• The transplant or reinfusion must be furnished in an approved transplant center. (An “approved transplant
center” is a hospital or other provider that's developed expertise in performing organ transplants, or bone
marrow or stem cell reinfusion, and meets the other approval standards we use.) We have agreements with
approved transplant centers in Washington and Alaska, and we have access to a special network of approved
transplant centers around the country. Whenever medically possible, we'll direct you to an approved transplant
center that we've contracted with for transplant services.
Of course, if none of our centers or the approved transplant centers can provide the type of transplant you
need, this benefit will cover a transplant center that meets the written approval standards we follow.
Recipient Costs
This benefit covers transplant and reinfusion-related expenses, including the preparation regiment for a bone
marrow or stem cell reinfusion. Also covered are anti-rejection drugs administered by the transplant center during
the inpatient or outpatient stay in which the transplant was performed.
Donor Costs
Covered donor services include selection, removal (harvesting) and evaluation of the donor organ, bone marrow
or stem cell; transportation of donor organ, bone marrow and stem cells, including the surgical and harvesting
teams; donor acquisition costs such as testing and typing expenses; and storage costs for bone marrow and stem
cells for a period of up to 12 months.
Travel And Lodging
Benefits are provided for certain travel expenses related to services provided by an approved transplant provider.
See Medical Transportation for details.
The Transplants benefit doesn’t cover:
• Organ, bone marrow and stem cell transplants, including any direct or indirect complications and aftereffects
thereof, that are not specifically stated under this benefit.
• Services and supplies that are payable by any government, foundation or charitable grant. This includes
services performed on potential or actual living donors and recipients, and on cadavers.
• Donor costs for an organ transplant or bone marrow or stem cell reinfusion that isn’t covered under this benefit,
or for a recipient who isn’t a member
• Donor costs for which benefits are available under other group or individual coverage
• Non-human or mechanical organs, unless we determine they aren’t “experimental/investigational services .” See
the Definitions section in this booklet
• Personal care items
• Planned storage of blood for more than 12 months against the possibility it might be used at some point in the
future
Urgent Care
This benefit covers services, such as:
Exams and treatment of:
• Minor sprains
• Cuts
• Ear, nose and throat infections
• Fever
Some services done during the urgent care visit may be covered under other benefits of this plan with different or
additional cost shares, such as:
• X-rays and lab work
• Shots or therapeutic injections
• Office surgeries
Urgent care centers can be part of a hospital or not. See the Summary of Your Costs for information about each
type of center you may visit.
47 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Virtual Care
Virtual care uses interactive audio and video technology or using store and forward technology in real-time
communication between the member at the originating site and the provider for diagnoses, consultation, or
treatment. Services must meet the following requirements:
• Covered service under this plan
• Originating site: Hospital, Rural health clinic, federally qualified health center, physician’s or other health care
provider office, community mental health center, skilled nursing facility, home, or renal dialysis center, except
an independent renal dialysis center
• If the service is provided through store and forward technology, there must be an associated office visit
between the member and the referring provider.
• Is Medically Necessary
This does not include services such as facsimile, email communication and SMS messages (texts) or services
that are not HIPAA compliant and secured. See the Summary Of Your Costs for the types of virtual visits
covered by this benefit.
Weight Management
Non-Surgical Weight Management
Benefits for non-surgical weight management are covered on the same basis as any other covered condition,
subject to the applicable benefits, limitations and exclusions.
Non-surgical weight management benefits include, but aren’t limited to, coverage of the following outpatient
medical services:
• Behavioral health visits
• Nutritional/dietician visits
• Physical therapy visits
• Physician visits
• Related lab and diagnostic services
For specific benefit information, please see the Mental Health Care, Preventive Care, Rehabilitation Therapy,
Professional Visits And Services, and Diagnostic Services benefits.
Surgical Weight Loss Treatment
Benefits for surgical treatment of morbid obesity are covered the same as any other in-network covered condition
subject to the criteria listed below, applicable benefits, limitations and exclusions.
This benefit will be provided only when covered services are furnished by in-network providers.
Weight loss surgery requires pre-approval. See Prior Authorization later in this booklet.
Coverage is available for bariatric procedures listed as medically necessary, when conservative measures have
proven ineffective. Examples of conservative measures include but aren’t limited to covered services under the
Non-Surgical Weight Management benefit, diet and exercise programs.
To qualify for surgical weight loss treatment, the member must meet the three criteria stated in the Claims
Administrator’s medical policy on bariatric surgery. Please see the Bariatric Surgery medical policy at
www.premera.com. A summary of the criteria is shown below:
• The member must be diagnosed as one of the following:
• A body mass index (BMI) greater than 40 kg/m2; or
• A BMI of 35 kg/m2 or more with at least ONE of the following conditions:
• Established Coronary Heart Disease, such as:
o History of angina pectoris (stable or unstable)
o History of angioplasty
o History of coronary artery surgery
o History of myocardial infarction
48 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• Other Atherosclerotic Disease, such as:
o Abdominal aortic aneurysm
o Hypertension that is uncontrolled or resistant to treatment (medically refractory) with a blood
pressure (BP) greater than 140/90 despite optimal medical management (attempted medical
management must have included at least 2 medications of different classes).
o Peripheral arterial disease
o Symptomatic carotid artery disease
• Type 2 Diabetes, uncontrolled by pharmacotherapy
• Obstructive sleep apnea, as documented by a sleep study (polysomnography), that is uncontrolled by
medical management (eg, CPAP or oral appliance).
• And participation in a physician administered weight reduction program lasting at least three continuous
months (over a 90 day period of time) within the 12 month period before surgery is considered.
• Evidence of active participation documented in the medical record includes:
o Weight
o Current dietary program (eg, MediFast, OptiFast)
o Physical activity (eg, exercise/work-out program)
• Or documentation of participation in a structured weight reduction program such as Weight Watchers or
Jenny Craig is an acceptable alternative if done in conjuction with physician supervision
You must also have a mental health evaluation and clearance by a licensed mental health provider to rule out any
mental health disorders that would be a contraindication to bariatric surgery, rule out inability to provide informed
consent, and rule out inability to comply with pre- and post-surgical requirements
For specific surgical treatment benefit information, please see the Hospital, Surgical Center Care-Outpatient and
Surgery benefits.
The Weight Management benefit does not cover:
• Procedures or treatments that are experimental and investigational (please see the Definitions section in this
booklet)
• Liposuction or surgical removal of excess skin unless medically necessary
• Over-the-counter medications for weight loss
• Liquid diet or fasting programs
• Other food replacement and nutritional supplements
• Membership in diet programs
• Exercise programs and health clubs
• Wiring of the jaw
• Weight management drugs
WHAT DO I DO IF I'M OUTSIDE WASHINGTON AND ALASKA?
OUT-OF-AREA CARE
As a member of the Blue Cross Blue Shield Association (“BCBSA”), Premera Blue Cross has arrangements with
other Blue Cross and Blue Shield Licensees (“Host Blues”) for care in Clark County, Washington and outside
Washington and Alaska. These arrangements are called “Inter-Plan Arrangements.” Our Inter-Plan
Arrangements help you get covered services from providers within the geographic area of a Host Blue.
The BlueCard
®
Program is the Inter-Plan Arrangement that applies to most claims from Host Blues' in-network
providers. The Host Blue is responsible for its in-network providers and handles all interactions with them. Other
Inter-Plan Arrangements apply to providers that are not in the Host Blues' networks (non-contracted providers).
This Out-Of-Area Care section explains how the plan pays both types of providers.
Receiving services through these Inter-Plan Arrangements does not change what the plan covers, benefit levels,
or any stated eligibility requirements. Please call us if your care needs prior authorization.
We process claims for the Prescription Drug benefit directly, not through an Inter-Plan Arrangement.
49 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
BlueCard Program
Except for copays, we will base the amount you must pay for claims from Host Blues’ in-network providers on the
lower of:
• The provider’s billed charges for your covered services; or
• The allowed amount that the Host Blue made available to us.
Often, the allowed amount is a discount that reflects an actual price that the Host Blue pays to the provider.
Sometimes it is an estimated price that takes into account a special arrangement with a single provider or a group
of providers. In other cases, it may be an average price, based on a discount that results in expected average
savings for services from similar types of providers.
Host Blues may use a number of factors to set estimated or average prices. These may include settlements,
incentive payments, and other credits or charges. Host Blues may also need to adjust their prices to correct their
estimates of past prices. However, we will not apply any further adjustments to the price of a claim that has
already been paid.
Clark County Providers Services in Clark County, Washington are processed through the BlueCard Program.
Some providers in Clark County do have contracts with us. These providers will submit claims directly to us, and
benefits will be based on our allowed amount for the covered service or supply.
Value-Based Programs You might have a provider that participates in a Host Blue's value-based program (VBP).
Value-based programs focus on meeting standards for treatment outcomes, cost and quality, and for coordinating
care when you are seeing more than one provider. The Host Blue may pay VBP providers for meeting the above
standards. If the Host Blue includes charges for these payments in the allowed amount for a claim, you would
pay a part of these charges if a deductible or coinsurance applies to the claim. If the VBP pays the provider for
coordinating your care with other providers, you will not be billed for it.
Taxes, Surcharges and Fees
A law or regulation may require a surcharge, tax or other fee be added to the price of a covered service. If that
happens, we will add that surcharge, tax or fee to the allowed amount for the claim.
Non-Contracted Providers
It could happen that you receive covered services from providers in Clark County, Washington and outside
Washington and Alaska that do not have a contract with the Host Blue. In most cases, we will base the amount
you pay for such services on either our allowed amount for these providers or the pricing requirements under
applicable law. See Allowed Amount in
Important Plan Information
in this booklet for details on allowed
amounts.
In these situations, you may owe the difference between the amount that the non-contracted provider bills and the
payment the plan makes for the covered services as set forth above.
Blue Cross Blue Shield Global
®
Core
If you are outside the United States, Puerto Rico, and the U.S. Virgin Islands (the “BlueCard service area”), you
may be able to take advantage of Blue Cross Blue Shield Global Core. Blue Cross Blue Shield Global Core is
unlike the BlueCard Program in the BlueCard service area in some ways. For instance, although Blue Cross Blue
Shield Global Core helps you access a provider network, you will most likely have to pay the provider and send us
the claim yourself in order for the plan to reimburse you. See How Do I File A Claim? for more information.
However, if you need hospital inpatient care, the service center can often direct you to hospitals that will not
require you to pay in full at the time of service. In such cases, these hospitals also send in the claim for you.
If you need to find a doctor or hospital outside the BlueCard service area, need help submitting claims or have
other questions, please call the service center at 1-800-810-BLUE (2583). The center is open 24 hours a day,
seven days a week. You can also call collect at 1-804-673-1177.
More Questions
If you have questions or need to find out more about the BlueCard Program, please call our customer service
department. To find a provider, go to www.premera.com/sebb or call 1-800-810-BLUE (2583). You can also
get Blue Cross Blue Shield Global Core information by calling the toll-free phone number.
50 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
CARE MANAGEMENT
Care Management services work to help ensure that you receive appropriate and cost-effective medical care.
Your role in the Care Management process is simple, but important, as explained below.
You must be eligible on the dates of service and services must be medically necessary. We encourage you to
call customer service to verify that you meet the required criteria for claims payment.
PRIOR AUTHORIZATION
You must get Premera's approval for some services before the service is performed. This process is called prior
authorization.
There are two different types of prior authorization required:
1. Prior Authorization For Benefit Coverage You must get prior authorization for certain types of medical
services, equipment, and for most inpatient facility stays. This is so that Premera can confirm that these
services are medically necessary and covered by the plan.
2. Prior Authorization For In-Network Cost shares For Out-Of-Network Providers You must get prior
authorization in order for an out-of-network provider to be covered at the plan’s in-network benefit level, except
for emergency services. See Exceptions To Prior Authorization For Out-of-Network Providers below for
more information.
How Prior Authorization Works
We will make a decision on a request for services that require prior authorization in writing within 5 calendar days
of receipt of all information necessary to make the decision. The response will let you know whether the services
are authorized or not, including the reasons why. If you disagree with the decision, you can ask for an appeal.
See Complaints and Appeals.
If your life or health would be in serious jeopardy if you did not receive treatment right away, you may ask for an
expedited review. We will respond in writing as soon as possible, but no more than 48 hours after we get all the
information we need to make a decision.
Our prior authorization will be valid for 90 calendar days. This 90-day period depends on your continued coverage
under the plan. If you do not receive the services within that time, you will have to ask us for another prior
authorization.
Prior Authorization for Benefit Coverage
Medical Services, Supplies or Equipment
The plan has a list of services, equipment, and facility types that must have prior authorization before you receive
the service or are admitted as an inpatient at the facility. Please contact your in-network provider or Premera
customer service before you receive a service to find out if your service requires prior authorization.
• In-network providers or facilities are required to request prior authorization for the service.
• Out-of-network and out-of-area providers and facilities will not request prior authorization for the service.
You have to ask Premera to prior authorize the service.
If you do not ask for prior authorization, and the plan covers the service, you will have to pay a penalty.
The amount is 50% of the allowed amount. However, you will not have to pay more than $1,500 per
occurrence in penalties. In addition, you also have to pay your cost-share.
Prescription Drugs
The plan has a specific list of prescription drugs that must have prior authorization before you get them at a
pharmacy. The E4 drug list is on our website at premera.com/sebb. Your provider can ask for a prior
authorization by faxing an accurately completed prior authorization form to us. This form is also on the pharmacy
section of our website.
If your provider does not get prior authorization, when you go to the pharmacy to get your prescription, the
pharmacy will tell you that you need it. You or your pharmacy should inform your provider of the need for prior
authorization. Your provider can fax us an accurately completed prior authorization form for review.
The plan may cover a small supply of the drug to allow more time for the prior authorization. The cost shares
51 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
shown in the Summary Of Your Costs will apply. In-Network pharmacies will find out if an emergency fill is
covered for your drug. The authorized amount of the emergency fill will be no more than the prescribed amount,
up to a seven-day supply or the minimum packaging size available at the time the emergency fill is dispensed.
See the process for emergency fills on our website at premera.com/sebb.
If an emergency fill is not allowed for your drug, you can still buy the drug before it is prior authorized, but you
must pay the full cost. If the drug is authorized after you bought it, you can send us a claim for reimbursement.
Reimbursement will be based on the allowed amount. See How Do I File A Claim? for details.
Sometimes, benefits for some prescription drugs may be limited to one or more of the following:
• A set number of days’ supply or a specific drug or drug dosage appropriate for a usual course of treatment.
• Certain drugs for a specific diagnosis
• Certain drugs from certain pharmacies, or you may need to get a prescription drug from an appropriate
medical specialist or a specific provider
• Step therapy, meaning you must try a generic drug or a specified brand name drug first
• Drug synchronization, meaning the coordination of medication refills for a patient taking two or more
medications for a chronic condition such that the patient's medications are refilled on the same schedule for
a given time period. Cost shares are adjusted if the fill is less than the standard refill amount in compliance
with state law.
These limits are based on medical standards, the drug maker’s advice, and your specific case. They are also
based on FDA guidelines and medical articles and papers.
Exceptions To Prior Authorization For Benefit Coverage
The following services do not require prior authorization for benefit coverage, but they do have separate
requirements:
• Emergency services and hospital admissions, including emergency drug or alcohol detox in a hospital.
• Childbirth admission to a hospital, or admissions for newborns who need emergency medical care at birth.
Emergency and childbirth hospital admissions do not require prior authorization, but you must notify us as soon
as reasonably possible.
Prior Authorization For Out-Of-Network Provider Coverage
Generally, non-emergent care by out-of-network providers is covered at a lower benefit level. However, you may
ask for a prior authorization to cover the out-of-network provider at the in-network benefit level if the services are
medically necessary and are only available from an out-of-network provider. You or the out-of-network provider
must ask for prior authorization before you receive the services.
Note: It is your responsibility to get prior authorization for any services that require it when you see a
provider that is out-of-network. If you do not get a prior authorization, the services will not be covered at
the in-network benefit level.
The prior authorization request for an out-of-network provider must include the following:
• A statement explaining how the provider has unique skills or provides unique services that are medically
necessary for your care, and that are not reasonably available from an in-network provider, and
• Medical records needed to support the request.
If the out-of-network services are authorized, the plan will cover the service at the in-network benefit level.
However, in addition to the cost shares, you may pay any amounts over the allowed amount if the
provider does not have a contract with us or the local Blue Cross and/or Blue Shield Licensee. Amounts
over the allowed amount do not count toward your plan deductible and out-of-pocket maximum.
Exceptions to Prior Authorization For Out-Of-Network Providers
Out-of-network providers can be covered at the in-network benefit level without prior authorization for emergency
services and hospital admissions for an emergency medical condition. This includes hospital admissions for
emergency drug or alcohol detox or for childbirth.
If you are admitted to an out-of-network hospital due to an emergency condition, those services are always
covered at the in-network benefit level. The plan will continue to cover those services until you are medically
stable and can safely transfer to an in-network hospital.
52 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
If you choose to stay in the out-of-network hospital after you are medically stable and can safely transfer to an in-
network hospital, you may be subject to additional charges which may not be covered by your plan.
CLINICAL REVIEW
Premera Blue Cross has developed or adopted guidelines and medical policies that outline clinical criteria used to
make medical necessity determinations. The criteria are reviewed annually and are updated as needed to ensure
our determinations are consistent with current medical practice standards and follow national and regional norms.
Practicing community doctors are involved in the review and development of our internal criteria. Our medical
policies are on our website. You or your provider may review them at www.premera.com/sebb. You or your
provider may also request a copy of the criteria used to make a medical necessity decision for a particular
condition or procedure. To obtain the information, please send your request to Care Management at the address
or fax number shown on the back cover.
Premera Blue Cross reserves the right to deny payment for services that are not medically necessary or that are
considered experimental/investigational. A decision by Premera Blue Cross following this review may be
appealed in the manner described in Complaints And Appeals.
In general, when there is more than one treatment option, the plan will cover the least costly option that will meet
your medical needs. Premera Blue Cross works cooperatively with you and your physician to consider effective
alternatives to hospital stays and other high-cost care to make better use of this plan's benefits.
PERSONAL HEALTH SUPPORT PROGRAMS
The plan offers participation in Premera Blue Cross's personal health support services to help members with such
things as managing complex medical conditions, a recent surgery, or admission to a hospital. Services include:
• Helping to overcome barriers to health improvement or following providers’ treatment plan
• Coordinating care services including access
• Helping to understand the health plan’s coverage
• Finding community resources
Participation is voluntary. To learn more about the personal health support programs, contact Customer Service
at the phone number listed on the back of your ID card.
CHRONIC CONDITION MANAGEMENT
Premera has contracted with a consumer digital health company (the program manager) to give members access
to a program of monitoring and health management support for certain chronic conditions described below. The
program is voluntary. Your digital readings/test results and other data are not shared with Premera, the
Washington State Healthcare Authority, or the School Employees Benefits Board Program, or anyone other than
the program manager. However, the program manager can share your data with your doctor or with someone
close to you if you choose. Please note that this program is voluntary. If you choose to participate in this
program, these services will be provided to you at no cost. Each member that qualifies to participate will be
contacted directly and provided a detailed program schedule.
Diabetes Management
For members who have Type 1 or Type 2 diabetes. If you qualify and join the chronic condition management
program, you will get:
• A blood glucose meter from the program manager that uploads blood sugar readings to a personal online
account.
• A lancing device and lancets.
• Test strips for this meter. You can reorder test strips using the meter or online. The strips will be sent to you
directly.
• Real-time reminders to check blood sugar or to take medication, and tips based on your blood sugar readings
that can help keep your levels within a healthy range.
• Coaching and support via phone, text, e-mail, or the program manager’s mobile app.
53 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Diabetes Prevention
For members who meet pre-diabetes criteria followed by the Centers for Disease Control. If you qualify and join
the program, you will get:
• A digital scale from the program manager that uploads readings to a personal online account.
• Lessons that cover topics such as nutrition, activity and stress.
• Coaching and support via phone, text, e-mail or the program manager’s mobile app.
EXCLUSIONS
In addition to services listed as not covered under Covered Services, this section of your booklet lists the
services that are either limited or not covered by this plan.
Amounts Over The Allowed Amount
Costs over the allowed amount as defined by this plan for a non-emergency service from a non-participating
provider.
Assisted Reproduction
Assisted reproduction technologies such as:
• Drugs to treat infertility or that are required as part of assisted reproduction procedures.
• Artificial insemination or assisted reproduction methods, such as in-vitro fertilization. It does not matter why
you need the procedure.
• Services to make you more fertile or for multiple births
• Reversing sterilization surgery
Benefits from other sources
Services that are covered by other types of insurance or coverage, such as:
• Motor vehicle medical or motor vehicle no-fault
• Any type of no-fault coverage, such as Personal Injury Protection (PIP), Medical Payment coverage, or Medical
Premises coverage
• Any type of liability insurance, such as homeowners' coverage or commercial liability coverage
• Any type of excess coverage
• Boat coverage
• School or athletic coverage
Benefits that have been exhausted
Services in excess of benefit limitations or maximums of this plan.
Broken or missed appointments
Broken or missed appointments, including charges from providers for broken or missed appointments.
Caffeine Dependency
Charges For Records or Reports
Charges from providers for supplying records or reports that aren’t requested by Premera for utilization review.
Complications of a non-covered service
This plan does not cover complications of a non-covered service, including follow-up services or effects of those
services.
Cosmetic Services
Drugs, services or supplies for cosmetic services. This includes services performed to reshape normal structures
of the body in order to improve or alter your appearance and not primarily to restore an impaired function of the
body. This does not apply to services that are determined to be medically necessary for Gender Affirming Care.
54 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Counseling, Education or Training
Counseling, education or training in the absence of illness or injury including but not limited to:
• Job help and outreach
• Social or fitness counseling
• Acting as a tutor, helping a member with schoolwork, acting as an educational or other aide for a member while
the member is at school, or providing services that are part of a school's individual education program or should
otherwise be provided by school staff
• Private school or boarding school tuition
• Community wellness or safety programs
Court-Ordered Services
Services that you must get to avoid being tried, sentenced, or losing the right to drive when they are not medically
necessary.
Custodial Care
Dental Care
Dental care or supplies, that are not covered under any dental benefits.
This exclusion also doesn't apply to dental services covered under the Temporomandibular Joint Disorders
(TMJ) Care benefit.EEG biofeedback or neurofeedback services
Environmental Therapy
Therapy designed to provide a changed or controlled environment.
Experimental or Investigational Services
Experimental or investigational services or supplies, including any complications or effects of such services. This
does not apply to certain services that are part of an approved clinical trial.
Family Members or Volunteers
Services or supplies that you provide to yourself. It also does not cover a provider who is:
• Your spouse, mother, father, child, brother or sister
• Your mother, father, child, brother or sister by marriage
• Your stepmother, stepfather, stepchild, stepbrother or stepsister
• Your grandmother, grandfather, grandchild or the spouse of one of these people
• A volunteer
Governmental Facilities
Services provided by a state or federal facility that are not emergency services or required by law or regulation.
Hair Analysis
Hair Loss
• Drugs, supplies, equipment, or procedures to replace hair, slow hair loss, or stimulate hair growth
• Hair prostheses, such as wigs or hair weaves, transplants and implants
Illegal Acts, Illegal Services and Terrorism
Illness or injury you get while committing a felony, an act of terrorism, or an act of riot or revolt, as well as any
service that is illegal under state or federal law.
Laser Therapy
Low-level laser therapy.
Military Service and War
Illness or injury that is caused by or arises from:
55 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• Acts of war, such as armed invasion, no matter if war has been declared or not
• Services in the armed forces of any country. , including any related civilian forces or units.
Non-Covered Services
Services or supplies directly related to any non-covered condition.
• Ordered when this plan is not in effect or when the person is not covered under this plan
• Provided to someone other than the ill or injured member
• That are not listed as covered under this plan
• Services and supplies for which no charge is made, for which none would have been made if this plan were
not in effect, or for which you are not legally required to pay
• Non-treatment charges, including charges for provider time
• Transporting a member in place of a parent or other family member or accompanying the member to
appointments or other activities outside the home, such as medical appointments or shopping
• Doing housework or chores for the member or helping the member do housework or chores
Non-Diagnostic Testing
Testing required for employment, schooling, screening, or public health purposes.
Non-Treatment Facilities, Institutions or Programs
• Institutional care
• Housing
• Incarceration
• Programs from facilities that are not licensed to provide medical or behavioral health treatment for covered
services. Examples are prisons, nursing homes, juvenile detention facilities.
Orthodontia
Orthodontic services, including casts, models, x-rays, photographs, examinations, appliances, braces, and
retainers.
Personal comfort or convenience items
• Personal services or items such as meals for guests while hospitalized, long-distance phone, radio or TV,
personal grooming, and babysitting.
• Normal living needs, such as food, clothes, housekeeping and transport.
• Dietary assistance, including “Meals on Wheels
Provider’s Licensing or Certification
Services that are outside the scope of the provider's license or certification or any unlicensed or uncertified
providers.
Recreational, Camp and Activity Programs
Recreational, camp and activity-based programs. These programs include:
• Gym, swim and other sports programs, camps and training
• Creative art, play and sensory movement and dance therapy
• Recreational programs and camps
• Wilderness, hiking, tall ship and other adventure programs and camps
• Boot camp programs and outward bound programs
• Equine programs and other animal-assisted programs and camps
• Exercise and maintenance-level programs
Serious Adverse Events and Never Events
Serious Adverse Event means a hospital injury caused by medical management (rather than an underlying
disease) that prolonged the hospitalization, and/or produces a disability at the time of discharge.
56 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Never Events means events that should never occur, such as a surgery on the wrong patient, a surgery on the
wrong body part or wrong surgery.
Members and this plan are not responsible for payment of services provided by in-network providers for serious
adverse events, never events and resulting follow-up care. Serious adverse events and never events are medical
errors that are specific to a nationally-published list. They are identified by specific diagnoses codes, procedure
codes and specific present-on-admission indicator codes. In-Network providers may not bill members for these
services and members are held harmless.
Not all medical errors are defined as serious adverse events or never events. You can obtain a list of serious
adverse events and never events by contacting us at or on the Centers for Medicare and Medicaid Services
(CMS) website.
Services or Supplies Not Medically Necessary
Services or supplies that are not medically necessary even if they are court-ordered. This also includes places of
service, such as inpatient hospital care or stays.
Sexual Dysfunction
Diagnosis and treatment of sexual dysfunctions, regardless of origin or cause; surgical, medical or psychological
treatment of impotence or hypoactive sexual desire disorder, including drugs, medications, or penile or other
implants.
Vision Exams
Routine vision exams to test visual acuity and/or to prescribe any type of vision hardware.
Vision Hardware
Vision hardware (and their fittings) used to improve visual sharpness, including eyeglasses and contact lenses,
and related supplies not covered under the Home Medical Equipment (HME), Orthotics, Prosthetics And
Supplies benefit. This plan never covers non-prescription eyeglasses or contact lenses, or other special purpose
vision aids (such as magnifying attachments), sunglasses or light-sensitive lenses, even if prescribed.
Vision Therapy
Vision therapy, eye exercise, or any sort of training to correct muscular imbalance of the eye (orthoptics), and
pleoptics treatment or surgeries to improve the refractive character of the cornea or results of such treatments.
Voluntary Support Groups
Patient support, consumer or affinity groups such as diabetic support groups or Alcoholics Anonymous
Work-Related Illness or Injury
Any illness, condition or injury for which you get benefits under:
• Separate coverage for illness or injury on the job
• Workers’ compensation laws
• Any other law that would pay you for an illness or injury you get on the job.
However, this exclusion doesn’t apply to owners, partners or executive officers who are full-time employees of the
Group if they’re exempt from the above laws and if the Group doesn’t furnish them with workers’ compensation
coverage. They’ll be covered under this plan for conditions arising solely from their occupations with the Group.
Coverage is subject to the other terms and limitations of this plan.
WHAT IF I HAVE OTHER COVERAGE?
Note: If you participate in a Health Savings Account (HSA) and have other health care coverage that is not a high
deductible health plan as defined by IRS regulations, the tax deductibility of the Health Savings Account
contributions may not be allowed. Contact your tax advisor or HSA plan administrator for more information.
COORDINATING BENEFITS WITH OTHER HEALTH CARE PLANS
When you have more than one health plan, “coordination of benefits (COB)” makes sure that the combined
payments of all your plans don't exceed your covered health costs. You or your provider should file your claims
with your primary plan first. If you have Medicare, Medicare may submit your claims to your secondary plan. See
57 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
COB's Effect On Benefits below in this section for details on primary and secondary plans.
If you do not know which is your primary plan, you or your provider should contact any of the health plans to verify
which plan is primary. The health plan you contact is responsible for working with the other plan(s) to determine
which is primary and will let you know within 30 calendar days.
Caution: All health plans have timely filing requirements. If you or your provider fails to submit your claim to your
secondary plan within that plan's claim filing time limit, the plan can deny the claim. If you experience delays in
the processing of your claim by the primary plan, you or your provider will need to submit your claim to the
secondary plan within its claim filing time limit to prevent a denial of the claim.
To avoid delays in claims processing, if you are covered by more than one plan you should promptly report to
your providers any changes in your coverage.
COB Definitions
For the purposes of COB:
• A plan is any of the following that provides benefits or services for medical or dental care. If separate contracts
are used to provide coordinated coverage for group members, all the contracts are considered parts of the
same plan and there is no COB among them. However, if COB rules don't apply to all contracts, or to all
benefits in the same contract, the contract or benefit to which COB doesn't apply is treated as a separate plan.
• “Plan” means: Group, individual or blanket disability insurance contracts, and group or individual contracts
issued by health care service contractors or HMOs, closed panel plans or other forms of group coverage;
medical care provided by long-term care plans; and Medicare or any other federal governmental plan, as
permitted by law.
• “Plan” doesn't mean: Hospital or other fixed indemnity or fixed payment coverage; accident-only coverage;
specified disease or accident coverage; limited benefit health coverage, as defined by state law; school
accident type coverage; non-medical parts of long-term care plans; automobile coverage required by law to
provide medical benefits; Medicare supplement policies; Medicaid or other federal governmental plans,
unless permitted by law.
• This plan means your plan's health care benefits to which COB applies. A contract may apply one COB
process to coordinating certain benefits only with similar benefits and may apply another COB process to
coordinate other benefits. All the benefits of your Premera Blue Cross plan are subject to COB, but your plan
coordinates dental benefits separately from medical benefits. Dental benefits are coordinated only with other
plans' dental benefits, while medical benefits are coordinated only with other plans' medical benefits.
• Primary plan is a plan that provides benefits as if you had no other coverage.
• Secondary plan is a plan that is allowed to reduce its benefits in accordance with COB rules. See COB's
Effect On Benefits later in this section for rules on secondary plan benefits.
• Allowable expense is a health care expense, including deductibles, coinsurance and copayments, that is
covered at least in part by any of your plans. When a plan provides benefits in the form of services, the
reasonable cash value of each service is an allowable expense and a benefit paid. An amount that isn't
covered by any of your plans isn't an allowable expense.
The allowable expense for the secondary plan is the amount it allows for the service or supply in the absence of
other coverage that is primary. This is true regardless of what method the secondary plan uses to set allowable
expenses.
The exceptions to this rule are when a Medicare, a Medicare Advantage plan, or a Medicare Prescription Drug
plan (Part D) is primary to your other coverage. In those cases, the allowable expense set by the Medicare
plan will also be the allowable expense amount used by the secondary plan.
• Custodial parent is the parent awarded custody by a court decree or, in the absence of a court decree, is the
parent with whom the child resides more than half of the calendar year, excluding any temporary visitation.
Primary And Secondary Rules
Certain governmental plans, such as Medicaid, are always secondary by law. Except as required by law,
Medicare supplement plans and other plans that don't coordinate benefits at all must pay as if they were primary.
A plan that doesn't have a COB provision that complies with Washington regulations is primary to a complying
plan unless the rules of both plans make the complying plan primary. The exception is group coverage that
supplements a package of benefits provided by the same group. Such coverage can be excess to the rest of that
58 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
group's plan. An example is coverage paired with a closed panel plan to provide out-of-network benefits.
The first of the rules below to apply decides which plan is primary. If you have more than one secondary plan, the
rules below also decide the order of the secondary plans to each other.
Non-Dependent Or Dependent The plan that doesn't cover you as a dependent is primary to a plan that does.
However, if you have Medicare, and federal law makes Medicare secondary to your dependent coverage and
primary to the plan that doesn't cover you as a dependent, then the order is reversed.
Dependent Children Unless a court decree states otherwise, the rules below apply:
• Birthday rule When the parents are married or living together, whether or not they were ever married, the plan
of the parent whose birthday falls earlier in the year is primary. If both parents have the same birthday, the plan
that has covered the parent the longest is primary.
• When the parents are divorced, separated or not living together, whether or not they were ever married:
• If a court decree makes one parent responsible for the child’s health care expenses or coverage, that plan is
primary. If the parent who is responsible has no health coverage for the dependent, but that parent's spouse
does, that spouse's plan is primary. This rule and the court decree rules below apply to calendar years
starting after the plan is given notice of the court decree.
• If a court decree assigns one parent primary financial responsibility for the child but doesn't mention
responsibility for health care expenses, the plan of the parent with financial responsibility is primary.
• If a court decree makes both parents responsible for the child's health care expenses or coverage, the
birthday rule determines which plan is primary.
• If a court decree requires joint custody without making one parent responsible for the child's health care
expenses or coverage, the birthday rule determines which plan is primary.
• If there is no court decree allocating responsibility for the child's expenses or coverage, the rules below
apply:
• The plan covering the custodial parent, first
• The plan covering the spouse of the custodial parent, second
• The plan covering the non-custodial parent, third
• The plan covering the spouse of the non-custodial parent, last
• If a child is covered by individuals other than parents or stepparents, the above rules apply as if those
individuals were the parents.
Retired Or Laid-Off Employee The plan that covers you as an active employee (an employee who is neither laid
off nor retired) is primary to a plan covering you as a retired or laid-off employee. The same is true if you are
covered as both a dependent of an active employee and a dependent of a retired or laid-off employee.
Continuation Coverage If you have coverage under COBRA or other continuation law, that coverage is
secondary to coverage that isn't through COBRA or other continuation law.
Note: The retiree/layoff and continuation rules don't apply when both plans don't have the rule or when the “non-
dependent or dependent” rule can decide which of the plans is primary.
Length Of Coverage The plan that covered you longer is primary to the plan that didn't cover you as long. If we
do not have your start date under the other plan, we will use the employee's hire date with the other group
instead. We will compare that hire date to the date your coverage started under this plan to find out which plan
covered you for the longest time.
If none of the rules above apply, the plans must share the allowable expenses equally.
COB's Effect On Benefits
The primary plan provides its benefits as if you had no other coverage.
A plan may take into account the benefits of another plan only when it is secondary to that plan. The secondary
plan is allowed to reduce its benefits so that the total benefits provided by all plans during a calendar year are not
more than the total allowable expenses incurred in that year. When paying a claim, the total amount paid by
the secondary plan in combination with what is paid by the primary plan is never required to be more than
one hundred percent of the highest total allowable expense of either plan plus any savings accrued from
prior claims incurred in the same calendar year.
59 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
The secondary plan must credit to its deductible any amounts it would have credited if it had been primary. It
must also calculate savings for each claim by subtracting its secondary benefits from the amount it would have
provided as primary. It must use these savings to pay any allowable expenses incurred during that calendar year,
whether or not they are normally covered.
This plan requires you or your provider to ask for prior authorization from Premera Blue Cross before you get
certain services or drugs. Your other plan may also require you to get prior authorization for the same service or
drug. In that case, when this plan is secondary to your other plan, you will not have to ask Premera for prior
authorization of any service or drug for which you asked for prior authorization from your other plan. This does
not mean that this plan will cover the service or drug. The service or drug will be reviewed once we receive your
claim.
Certain facts about your other health care coverage are needed to apply the COB rules. We may get the facts we
need for COB from, or give them to, other plans, organizations or persons. We don't need to tell or get the
consent of anyone to do this. State regulations require each of your other plans and each person claiming
benefits under this plan to give us any facts we need for COB. To expedite payment, be sure that you and/or your
provider supply the information in a timely manner.
If the primary plan fails to pay within 60 calendar days of receiving all necessary information from you and your
provider, you and/or your provider may submit your claim to the secondary plan to make payment as if the
secondary plan was primary. In such situations, the secondary plan is required to pay claims within 30 calendar
days of receiving your claim and notice that your primary plan has not paid. However, the secondary plan may
recover from the primary plan any excess amount paid under the Right of Recovery/Facility of Payment
provision in the plan.
Right Of Recovery/Facility Of Payment
The plan has the right to recover any payments that are greater than those required by the coordination of
benefits provisions from one or more of the following:
• The persons the plan paid or for whom the plan has paid
• Providers of service
• Insurance companies
• Service plans or other organizations
If a payment that should have been made under this plan was made by another plan, the plan also has the right to
pay directly to another plan any amount that the plan should have paid. Such payment will be considered a
benefit under this plan and will meet the plan’s obligations to the extent of that payment. This plan has the right to
appoint a third party to act on its behalf in recovery efforts.
SUBROGATION AND REIMBURSEMENT
If we make claims payment on your behalf for injury or illness for which another party is liable, or for which
uninsured/underinsured motorist (UIM) or personal injury protection (PIP) insurance exists, we will be subrogated
to any rights that you may have to recover compensation or damages from that liable party related to the injury or
illness, and we would be entitled to be repaid for payments we made on your behalf out of any recovery that you
obtain from that liable party after you have been fully compensated for your loss. The liable party is also known
as the “third party” because it is a party other than you or us. This party includes a UIM carrier because it stands
in the shoes of a third party tort feasor and because we exclude coverage for such benefits.
Definitions The following terms have specific meanings in this contract:
• Subrogation means we may collect directly from third parties or from proceeds of your recovery from third
parties to the extent we have paid on your behalf for illnesses or injury caused by the third party and you have
been fully compensated for your loss.
• Reimbursement means that you are obligated under the contract to repay any monies advanced by us from
amounts you have received on your claim after you have been fully compensated for your loss.
• Restitution means all equitable rights of recovery that we have to the monies advanced under your plan.
Because we have paid for your illness or injuries, we are entitled to recover those expenses from any
responsible third-party once you have been fully compensated for your loss.
To the fullest extent permitted by law, we are entitled to the proceeds of any settlement or judgment that results in
a recovery from a third party, up to the amount of payments we have made on your behalf after you have been
60 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
fully compensated for your loss. Our right to recover exists regardless of whether it is based on subrogation,
reimbursement or restitution. In recovering payments made on your behalf, we may at our election hire our own
attorney to prosecute a subrogation claim for recovery of payments we have made on your behalf directly from
third-parties, or be represented by your attorney prosecuting a claim on your behalf. Our right to prosecute a
subrogation claim against third-parties is not contingent upon whether or not you pursue the party at fault for any
recovery. If you recover from a third party and we share in the recovery, we will pay our share of the reasonable
legal expenses. Our share is that percentage of the legal expenses reasonable and necessary to secure a
recovery against the liable party that the amount we actually recover bears to the total recovery.
Before accepting any settlement on your claim against a third party, you must notify us in writing of any terms or
conditions offered in a settlement, and you must notify the third party of our interest in the settlement established
by this provision. In the event of a trial or arbitration, you must make a claim against, or otherwise pursue
recovery from third-parties payments we have made on your behalf, and give us reasonable notice in advance of
the trial or arbitration proceeding. (See Notices later in this booklet.) You must also cooperate fully with us in
recovering amounts paid by us on your behalf. If you retain an attorney or other agent to represent you in the
matter, you must require your attorney or agent to reimburse us directly from the settlement or recovery. If you
fail to cooperate fully with us in the recovery of the payments we have paid on your behalf, you are responsible for
reimbursing us for payments we have made on your behalf.
You agree, if requested, to hold in trust and execute a trust agreement in the full amount of payments we made
on your behalf from any recovery you obtain from any third-party until such time as we have reached a final
determination or settlement regarding the amount of your recovery that fully compensates you for your loss.
UNINSURED AND UNDERINSURED MOTORIST/PERSONAL INJURY PROTECTION COVERAGE
We have the right to be reimbursed for benefits provided, but only to the extent that benefits are also paid for such
services and supplies under the terms of a motor vehicle uninsured motorist and/or underinsured motorist (UIM)
policy, personal injury protection (PIP) or similar type of insurance or contract.
Medical Plan Eligibility and Enrollment
In these sections, “health plan” is used to refer to a plan offering medical, vision, dental, or any combination of
these coverages, developed by the School Employees Benefits Board (SEBB) and provided by a contracted
vendor or self-insured plans administered by the Health Care Authority (HCA).
Eligibility for Subscribers and Dependents
School Employee Eligibility
The school employee’s SEBB organization will inform the school employee in writing whether or not they are
eligible for SEBB benefits upon employment and whenever their eligibility status changes. The written notice will
include information about the school employee’s right to appeal eligibility and enrollment decisions.
A school employee of an employer group (such as an employee organization representing school employees or a
tribal school) that contracts with HCA for SEBB benefits should contact their payroll or benefits office for eligibility
criteria.
School employees have the right to appeal eligibility and enrollment decisions. Information about appeals can be
found under “Appeal rights.”
Continuation Coverage Eligibility
The SEBB Program determines whether subscribers are eligible for continuation coverage (COBRA or Unpaid
Leave) upon receipt of their election to enroll in SEBB Continuation Coverage (COBRA or Unpaid Leave). If the
subscriber requests to enroll in and is not eligible for continuation coverage, the SEBB Program will notify them of
their right to appeal. Information about appeals can be found under “Appeal rights.”
School board member eligibility
The SEBB Program determines whether a school board member is eligible to self -pay coverage upon receipt of
their election to enroll. If a school board member requests to enroll and is not eligible, the SEBB Program will
notify them of their right to appeal. Information about appeals can be found under “Appeal rights.”
61 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Dependent Eligibility
The following are eligible dependents:
• Legal spouse
• State-registered domestic partner and substantially equivalent legal unions from jurisdictions as defined in
Washington State statute. Individuals in a state-registered domestic partnership are treated the same as
a legal spouse except when in conflict with federal law.
• Children, through the last day of the month in which their 26th birthday occurred regardless of marital
status, student status, or eligibility for coverage under another plan. It also includes children age 26 or
older with a disability as described below in “Children of any age with a developmental or physical
disability.” Children are defined as the subscriber’s:
• Children based on establishment of a parent-child relationship, as described in Washington
State statutes, except when parental rights have been terminated.
• Children of the subscriber’s spouse, based on the spouse’s establishment of a parent-child
relationship, except when parental rights have been terminated. The stepchild’s relationship to the
subscriber (and eligibility as a dependent) ends on the same date the marriage with the spouse ends
through divorce, annulment, dissolution, termination, or death.
• Children for whom the subscriber has assumed a legal obligation for total or partial support in
anticipation of adoption of the child.
• Children of the subscriber’s state-registered domestic partner, based on the state-registered
domestic partner’s establishment of a parent-child relationship, except when parental rights have
been terminated. The child’s relationship to the subscriber (and eligibility as a dependent) ends on the
same date the subscriber’s legal relationship with the state-registered domestic partner ends through
divorce, annulment, dissolution, termination, or death.
• Children specified in a court order or divorce decree for whom the subscriber has a legal
obligation to provide support or health care coverage.
• Extended dependents in the legal custody or legal guardianship of the subscriber, the
subscriber’s spouse, or the subscriber’s state-registered domestic partner. The legal
responsibility is demonstrated by a valid court order and the child’s official residence with the
custodian or guardian. Extended dependent child does not include foster children unless the
subscriber, the subscriber’s spouse, or the subscriber’s state-registered domestic partner has
assumed a legal obligation for total or partial support in anticipation of adoption.
• Children of any age with a developmental or physical disability that renders them incapable of
self-sustaining employment and chiefly dependent upon the subscriber for support and maintenance,
provided such condition occurs before the age of 26. The following requirements apply to a
dependent child with a disability:
• The subscriber must provide proof of the disability and dependency within 60 days of the child’s
attainment of age 26.
• The subscriber must notify the SEBB Program in writing when the child is no longer eligible
under this subsection.
• A child with a developmental or physical disability who becomes self -supporting is not eligible
as of the last day of the month in which they become capable of self -support.
• A child with a developmental or physical disability age 26 and older who becomes capable of
self-support does not regain eligibility if they later become incapable of self -support.
• The SEBB Program, with input from the medical plan, will periodically verify the eligibility of a
dependent child with a disability beginning at age 26, but no more frequently than annually after
the two-year period following the child’s 26th birthday. Verification will require renewed proof of
disability and dependence from the subscriber.
62 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Enrollment for Subscribers and Dependents
For all Subscribers and Dependents
• To enroll at any time other than during the initial enrollment period, see “Making changes.”
• Any dependents enrolled in medical coverage will be enrolled in the same medical plan as the subscriber.
School Employee Enrollment
A school employee must use the SEBB My Account online enrollment system or Benefits 24/7 (once available) or
submit a School Employee Enrollment or School Employee Enrollment (for Medical Only Groups) form and any
supporting documents to their SEBB organization or employer group when they become newly eligible or regain
eligibility for SEBB benefits. The online enrollment must be completed or the form must be received no later than
31 days after the date the school employee becomes eligible or regains eligibility.
If the school employee does not enroll online or return the form by the deadline, the school employee will be
enrolled in Uniform Medical Plan Achieve 1 and a tobacco use premium surcharge will be incurred. Consequently,
dependents cannot be enrolled until the SEBB Program’s next annual open enrollment or when a qualifying event
occurs that creates a special open enrollment for enrolling a dependent.
Waiving Medical Enrollment
An eligible school employee may waive enrollment in SEBB medical if they are enrolled in other employer-based
group medical, a TRICARE plan, or Medicare. If a school employee waives enrollment in SEBB medical, the
school employee cannot enroll eligible dependents. For information on when an eligible school employee may
waive medical plan enrollment after their initial enrollment period, or to enroll after having waived, see “Making
changes.”
Continuation Coverage Enrollment
A subscriber enrolling in SEBB Continuation Coverage (COBRA or Unpaid Leave) may enroll by using Benefits
24/7, the online enrollment system (once available). or by submitting the applicable SEBB Continuation
Coverage Election/Change form and any supporting documents to the SEBB Program. The online enrollment
must be completed or the SEBB Program must receive the election form no later than 60 days from the date
the enrollee’s SEBB health plan coverage ended or from the postmark date on the SEBB Continuation Coverage
Election Notice sent by the SEBB Program, whichever is later.
Premiums and applicable premium surcharges associated with continuing SEBB medical must be made directly
to HCA. The first premium payment and applicable premium surcharges are due to HCA no later than 45 days
after the election period ends as described above. For more information, see “Options for continuing SEBB
medical coverage” and the SEBB Continuation Coverage Election Notice.
School board member enrollment
A school board member is required to enroll in a medical plan.
A school board member may enroll and self-pay premiums by submitting the School Board Member
Election/Change form and any supporting documents to the SEBB Program. The SEBB Program must receive the
form as follows:
• Currently elected or appointed school board members: Between November 1, 2023 and February 29,
2024.
• Newly elected or appointed school board members: No later than 60 days after their elected or appointed
term begins.
Premiums and applicable premium surcharges associated with continuing SEBB medical must be made directly
to HCA. The first premium payment and applicable premium surcharges are due to HCA no later than 45 days:
• After January 1, 2024 for a school board member whose form is received on or before December 31, 2023.
• After February 29, 2024 for a school board member whose form is received between January 1, 2024 and
February 29, 2024.
• After the 60-day election period ends for a newly elected or appointed school board member as described
above.
63 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
A school board member may renew their participation at the start of each subsequent term as a school board
member. If a school board member is reelected for a new term consecutive from their previous term, they will not
be required to make new elections.
Dependent Enrollment
To enroll an eligible dependent, the subscriber must include the dependent’s information online using SEBB My
Account or Benefits 24/7 (once available), or on the applicable enrollment form and provide the required
document(s) as proof of the dependent’s eligibility. The dependent will not be enrolled in SEBB health plan
coverage if the SEBB Program, the SEBB organization, or the employer group is unable to verify their eligibility
within the SEBB Program enrollment timelines.
National Medical Support Notice (NMSN)
When a National Medical Support Notice (NMSN) requires a subscriber to provide health plan coverage for a
dependent child, the following provisions apply:
The subscriber may enroll their dependent child and request changes to their health plan coverage as described
under “Changes to health plan coverage or enrollment are allowed as directed by the NMSN,” below.
• A school employee must use the SEBB My Account online enrollment system or Benefits or submit the
(once available) required form(s) to their SEBB organization or employer group.
• Any other subscriber must use Benefits 24/7 (once available) or submit the required form(s) to the
SEBB Program.
If the subscriber fails to request enrollment or health plan coverage changes as directed by the NMSN, the SEBB
organization, the employer group, or the SEBB Program may make enrollment or health plan coverage changes
according to “Changes to health plan coverage or enrollment are allowed as directed by the NMSN,” below, upon
request of:
• The child’s other parent.
• A child support enforcement program.
Changes to health plan coverage or enrollment are allowed as directed by the NMSN:
a) The dependent will be enrolled under the subscriber’s health plan coverage as directed by the
NMSN.
b) A school employee who has waived SEBB medical will be enrolled in medical as directed by the
NMSN, in order to enroll the dependent.
c) The subscriber’s selected health plans will be changed if directed by the NMSN.
d) If the dependent is already enrolled under another SEBB subscriber, the dependent will be removed
from the other health plan coverage and enrolled as directed by the NMSN.
e) If the dependent is enrolled in both SEBB medical and Public Employees Benefits Board (PEBB)
medical as a dependent and there is an NMSN in place, enrollment will be in accordance with the
NMSN.
f) If the subscriber is eligible for and elects Consolidated Omnibus Budget Reconciliation Act (COBRA)
coverage or other continuation coverage, the NMSN will be enforced and the dependent must be
covered in accordance with the NMSN.
Changes to health plan coverage or enrollment as described above in (a) through (c) will begin the first day of the
month following receipt of the NMSN. If the NMSN is received on the first day of the month, the change to health
plan coverage or enrollment begins on that day.
A dependent will be removed from the subscriber’s health plan coverage as described above in (d) the last day of
the month the NMSN is received. If that day is the first of the month, the change in enrollment will be made the
last day of the previous month.
When a NMSN requires a subscriber’s spouse, former spouse, or other individual to provide health plan coverage
for a dependent who is already enrolled in the subscriber’s SEBB coverage, and that health plan coverage is in
fact provided, the dependent may be removed from the subscriber’s SEBB health plan coverage prospectively.
64 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Dual Enrollment
A subscriber and their dependents may each be enrolled in only one SEBB medical plan.
A school employee or their dependent who is eligible to enroll in both the SEBB Program and the Public
Employees Benefits Board (PEBB) Program is limited to a single enrollment in either the SEBB or PEBB
Program.
For example:
• A child who is an eligible dependent under two parents enrolled in SEBB Program benefits may be
enrolled as a dependent under both parents but is limited to a single enrollment in SEBB medical.
• A child who is an eligible dependent of a school employee in the SEBB Program and an employee in the
PEBB Program may only be enrolled as a dependent under one parent in either the SEBB or PEBB
Program.
Medicare Eligibility and Enrollment
School Employee and Dependent
If a school employee or their dependent becomes eligible for Medicare, they should contact the Social Security
Administration to ask about the advantages of immediate or deferred Medicare enrollment.
A school employee or their dependent are deemed eligible for Medicare when they have the option to receive
Medicare Part A benefits. If a school employee or their dependent chooses to enroll in Medicare Part A, Medicare
regulations and guidelines will determine whether Medicare is the primary or secondary payer.
A school employee or their dependent who is enrolled in Medicare may remain enrolled in SEBB medical
coverage. However, a school employee may choose to waive their SEBB medical coverage or remove their
dependent from their SEBB medical coverage and choose Medicare as their primary insurer. If a school employee
does so, neither the school employee nor their dependent can enroll in SEBB medical except during the annual
open enrollment or a special open enrollment.
In most situations, a school employee and their dependent can defer Medicare Part B enrollment without a
penalty while enrolled in SEBB medical coverage. When the school employee terminates employment, the school
employee and the dependent can enroll in Medicare Part B during a Special Enrollment Period. If Medicare
eligibility is due to a disability, the school employee or their dependent must contact the Social Security
Administration about deferring enrollment in Medicare Part B.
Upon retirement, Medicare will become the primary insurance payer, and the PEBB medical plan will become
secondary. See “PEBB retiree insurance coverage.”
Continuation Coverage Subscriber, a school board member, or their
Dependent
If a continuation coverage subscriber, a school board member, or their dependent becomes eligible for
Medicare, federal regulations allow enrollment in Medicare three months before they turn age 65. If they do not
enroll within three months before the month they turn age 65, enrollment in Medicare may be delayed. If
enrollment in Medicare does not occur when the subscriber or their dependent is first eligible, a late enrollment
penalty may apply.
A SEBB Continuation Coverage (COBRA) subscriber must notify the SEBB Program in writing within 30 days
if, after electing SEBB Continuation Coverage (COBRA), a subscriber or their dependent becomes eligible for
Medicare (Part A, Part B, or both) or becomes covered under other group health plan coverage. If a subscriber or
their dependent enrolls in SEBB Continuation Coverage (COBRA) and then becomes eligible for Medicare, their
enrollment in SEBB Continuation Coverage (COBRA) will be terminated at the end o f the month in which they
become eligible for Medicare due to turning age 65 or older or when enrolled in Medicare due to a disability. This
may cause the SEBB Continuation Coverage (COBRA) to be terminated early, before the subscriber has used all
the months they would otherwise be entitled to. A subscriber or their dependent who are already enrolled in
Medicare when they enroll in SEBB Continuation Coverage (COBRA) will not have their coverage terminated
early.
65 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
When Medical Coverage Begins
School Employees and Dependents
For a newly eligible school employee and their eligible dependents, medical coverage begins the first day of
the month following the date the school employee becomes eligible.
Exceptions:
• Medical coverage begins on the school employee’s first day of work when their first day of work is on or
after September 1, but not later than the first day of school for the current school year as established by
the SEBB organization.
• When a school employee establishes eligibility toward SEBB benefits at any time in the month of August,
medical coverage begins on September 1
only if the school employee is also determined to be eligible for
the school year that begins on September 1.
For a school employee regaining eligibility, including following a period of leave as described in SEBB
Program rules, and their eligible dependents, medical coverage begins the first day of the month following the
school employee’s return to work if the school employee is anticipated to be eligible for the employer contribution.
Note: When a school employee who is called to active duty in the uniformed services under the Uniformed
Services Employment and Reemployment Rights Act (USERRA) loses eligibility for the employer contribution
toward SEBB benefits, they regain eligibility for the employer contribution toward SEBB benefits the day they
return from active duty. Medical coverage begins the first day of the month in which the school employee returns
from active duty.
Continuation Coverage Subscribers and Dependents
For a continuation coverage subscriber and their eligible dependents enrolling when newly eligible due to a
qualifying event, medical coverage begins the first day of the month following the day they lost eligibility for SEBB
medical plan coverage.
School board members and dependents
For a currently elected or appointed school board member and their eligible dependents enrolling between
November 1, 2023 and February 29, 2024, medical coverage begins as follows:
• If the required form is received on or before December 31, 2023, medical coverage begins January 1, 2024;
or
• If the required form is received between January 1, 2024 and February 29, 2024, medical coverage begins
the first day of the month following the day the SEBB Program receives the required form.
For a newly elected or appointed school board member and their eligible dependents, medical coverage
begins the first day of the month following the day the SEBB Program receives the required form.
All Subscribers and Dependents
For a subscriber or their eligible dependents enrolling during the SEBB Program’s annual open
enrollment, medical coverage begins January 1 of the following year.
For a subscriber or their eligible dependents enrolling during a special open enrollment, medical coverage
begins the first day of the month following the later of the event date or the date the online enrollment election
using SEBB My Account or Benefits 24/7 (once available), or the required form is received. If that day is the first
of the month, medical coverage begins on that day.
If the special open enrollment is due to the birth or adoption of a child, or when the subscriber has assumed a
legal obligation for total or partial support in anticipation of adoption of a child, medical coverage will begin as
follows:
• For a school employee, medical coverage will begin the first day of the month in which the event occurs.
• For a newly born child, medical coverage will begin the date of birth.
• For a newly adopted child, medical coverage will begin on the date of placement or the date a legal
obligation is assumed in anticipation of adoption, whichever is earlier.
66 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• For a spouse or state-registered domestic partner of a subscriber, medical coverage will begin the
first day of the month in which the event occurs.
If the special open enrollment is due to the enrollment of an extended dependent or a dependent child with a
disability, medical coverage will begin the first day of the month following the event date or eligibility certification,
whichever is later.
Making Changes
Removing a dependent who is no longer eligible
A subscriber must provide notice to remove a dependent who is no longer eligible due to divorce, annulment,
dissolution, or a qualifying event of a dependent ceasing to be eligible as a dependent child as described under
“Dependent eligibility.” The notice must be received within 60 days of the last day of the month the dependent no
longer meets the eligibility criteria.
• A school employee must provide notice online using SEBB My Account or Benefits 24/7 (once
available), or by submitting a written request to their SEBB organization or employer group.
• Any other subscriber must provide notice online using Benefits 24/7 (once available) or by submitting a
written request to the SEBB Program.
Consequences for not submitting notice within the required 60 days may include, but are not limited to:
• The dependent may lose eligibility to continue SEBB medical coverage under one of the continuation
coverage options described in “Options for continuing SEBB medical coverage.”
• The subscriber may be billed for claims paid by the medical plan for services that were rendered after the
dependent lost eligibility.
• The subscriber may not be able to recover subscriber-paid insurance premiums for the dependent that
lost eligibility.
• The subscriber may be responsible for premiums paid by the state for the dependent’s medical plan
coverage after the dependent lost eligibility.
Voluntary termination for continuation coverage subscribers or school
board members
A continuation coverage subscriber or a school board member may voluntarily terminate enrollment in a medical
plan at any time by submitting a request online using Benefits 24/7 (once available) or in writing to the SEBB
Program. Enrollment in the medical plan will be terminated the last day of the month in which the request was
received online or by the SEBB Program , or on the last day of the month specified in the termination request,
whichever is later. If the request is received on the first day of the month, medical plan enrollment will be
terminated on the last day of the previous month.
Note: A school board member must be enrolled in all SEBB health plan coverage, including SEBB medical, SEBB
dental, and SEBB vision. A school board member who voluntarily terminates enrollment in a medical plan also
terminates all other health plan enrollment.
Making changes during annual open enrollment and special open
enrollment
A subscriber may make certain changes to their enrollment during the annual open enrollment and if a specific life
event creates a special open enrollment period.
Annual Open Enrollment Changes
A school employee may make the following changes to their enrollment during the SEBB Program’s annual
open enrollment period:
• Change their medical plan
• Waive their medical plan enrollment
• Enroll after waiving medical plan enrollment
• Enroll or remove eligible dependents
67 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
A school employee must submit the election change online using SEBB My Account or Benefits 24/7 (once
available) or submit the required School Employee Change form and any supporting documents to their SEBB
organization or employer group. The change must be completed in online, or the forms received, no later than the
last day of the annual open enrollment period and will be effective January 1 of the following year.
Any other subscriber may make the following changes to their enrollment during the SEBB Program’s annual
open enrollment period:
• Enroll in or terminate enrollment in a medical plan
• Change their medical plan
• Enroll or remove eligible dependents
A continuation coverage subscriber must submit the election change online using Benefits 24/7 (once
available) or submit the required SEBB Continuation Coverage (COBRA) Election/Change, or SEBB Continuation
Coverage (Unpaid Leave) Election/Change form (as appropriate) and any supporting documents to the SEBB
Program. The change must be completed online, or the forms received, no later than the last day of the annual
open enrollment period and will be effective January 1 of the following year.
A school board member must submit the election change online using Benefits 24/7 (once available) or submit
the required School Board Member Election/Change form and any supporting documents to the SEBB Program.
The change must be completed online, or the forms received, no later than the last day of the annual open
enrollment period and will be effective January 1 of the following year.
Special Open Enrollment Changes
A subscriber may change their enrollment outside of the annual open enrollment period if a qualifying event
creates a special open enrollment period. However, the change in enrollment must be allowable under Internal
Revenue Code (IRC) and Treasury Regulations and correspond to and be consistent with the event that creates
the special open enrollment for the subscriber, their dependent, or both.
A special open enrollment event must be other than a school employee gaining initial eligibility or regaining
eligibility for SEBB benefits. The subscriber must provide evidence of the event that created the special open
enrollment.
A special open enrollment may allow a subscriber to make the following changes:
• Enroll in or change their medical plan
• Waive their medical plan enrollment
• Enroll after waiving medical plan enrollment
• Enroll or remove eligible dependents
To request a special open enrollment:
• A school employee must make the change online using SEBB My Account or Benefits 24/7 (once
available) or submit the required School Employee Change form and any supporting documents to their
SEBB organization or employer group.
• A continuation coverage subscriber must make the change online using Benefits 24/7 (once available)
or submit the required SEBB Continuation Coverage (COBRA) Election/Change, or SEBB Continuation
Coverage (Unpaid Leave) Election/Change form (as appropriate) and any supporting documents to the
SEBB Program.
• A school board member must make the change online using Benefits 24/7 (once available) or submit
the required School Board Member Election/Change form and any supporting documents to the SEBB
Program.
The change must be completed online, or the forms must be received no later than 60 days after the event that
creates the special open enrollment. In addition, the SEBB Program, the SEBB organization, or the employer
group will require the subscriber to provide proof of a dependent’s eligibility, evidence of the event that created
the special open enrollment, or both.
Exception: If a subscriber wants to enroll a newborn or child whom the subscriber has adopted or has assumed a
legal obligation for total or partial support in anticipation of adoption in SEBB health plan coverage, the subscriber
should complete the request online or notify their SEBB organization, their employer group, or the SEBB Program
by submitting the required forms as soon as possible to ensure timely payment of claims. If adding the child
68 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
increases the premium, the request must be received online, or the required forms must be received no later than
60 days after the date of the birth, adoption, or the date the legal obligation is assumed for total or partial support
in anticipation of adoption.
Special open enrollment events that allow for a change in health plans
A subscriber may not change their health plan during a special open enrollment if their state-registered domestic
partner or state-registered domestic partner’s child is not a tax dependent.
Any of the following events may create a special open enrollment:
• Subscriber gains a new dependent due to:
• Marriage or registering a state-registered domestic partnership.
• Birth, adoption, or assuming a legal obligation for total or partial support in anticipation of adoption.
• A child becoming eligible as an extended dependent through legal custody or legal guardianship.
• Subscriber or their dependent loses other coverage under a group health plan or through health
insurance coverage, as defined by the Health Insurance Portability and Accountability Act (HIPAA).
• Subscriber has a change in employment status that affects their eligibility for the employer contribution
toward their employer-based group health plan.
• Subscriber has a change in employment
• location that affects medical plan availability. If the subscriber changes employment locations and
their current medical plan is no longer available, the subscriber must select a new medical plan as
described in SEBB Program rules. If the subscriber does not elect a new medical plan as required,
they will be enrolled in a SEBB medical plan designated by the director of HCA or their designee if the
subscriber has one or more new medical plans available, the subscriber may select to enroll in a
newly available plan.
• Subscriber’s dependent has a change in their own employment status that affects their eligibility or their
dependent’s eligibility for the employer contribution under their employer-based group health plan.
“Employer contribution” means contributions made by the dependent’s current or former employer toward
health coverage as described in the Treasury Regulation.
• Subscriber or their dependent has a change in residence that affects health plan availability. If the
subscriber has a change in residence and their current medical plan is no longer available, the subscriber
must select a new medical plan, as described in SEBB Program rules. If the subscriber does not elect a
new medical plan as required, they will be enrolled in a SEBB medical plan designated by the director of
HCA or their designee.
• A court order requires the subscriber or any other individual to provide insurance coverage for an eligible
dependent of the subscriber (a former spouse or former state-registered domestic partner is not an
eligible dependent).
• Subscriber or their dependent enrolls in coverage under Medicaid or a state Children’s Health Insurance
Program (CHIP), or the subscriber or their dependent loses eligibility for coverage under Medicaid or
CHIP.
• Subscriber or their dependent becomes eligible for state premium assistance subsidy for SEBB health
plan coverage from Medicaid or CHIP.
• Subscriber or their dependent enrolls in coverage under Medicare, or the subscriber or their dependent
loses eligibility for coverage under Medicare. If the subscriber’s current medical plan becomes
unavailable due to the subscriber or their dependents enrollment in Medicare, the subscriber must select
a new medical plan.
• Subscriber or their dependent’s current medical plan becomes unavailable because the subscriber or
enrolled dependent is no longer eligible for a health savings account (HSA).
• Subscriber or their dependent experiences a disruption of care for active and ongoing treatment that
could function as a reduction in benefits for the subscriber or their dependent. The subscriber may not
change their health plan election because the subscriber or dependent’s physician stops participation with
the subscriber’s health plan unless the SEBB Program determines that a continuity of care issue exists.
The SEBB Program will consider but not limit its consideration to the following:
• Active cancer treatment, such as chemotherapy or radiation therapy
69 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• Treatment following a recent organ transplant
• A scheduled surgery
• Recent major surgery still within the postoperative period
• Treatment for a high-risk pregnancy
• The SEBB Program determines that there has been a substantial decrease in the providers available
under a SEBB medical plan.
Note: The plan cannot guarantee that any physician, hospital, or other provider will be available or remain under
contract with the plan. An enrollee may not change medical plans simply because their provider or health care
facility discontinues participation with this medical plan until the SEBB Program’s next annual open enrollment or
when another qualifying event creates a special open enrollment for changing health plans, unless the SEBB
Program determines that a continuity of care issue exists or there has been a substantial decrease in the
providers available under the plan.
Special open enrollments events that allow adding or removing a dependent
Any of the following events may create a special open enrollment:
• Subscriber gains a new dependent due to:
• Marriage or registering a state-registered domestic partnership.
• Birth, adoption, or when the subscriber has assumed a legal obligation for total or partial support in
anticipation of adoption.
• A child becoming eligible as an extended dependent through legal custody or legal guardianship.
• Subscriber or their dependent loses other coverage under a group health plan or through health
insurance coverage, as defined by the Health Insurance Portability and Accountability Act (HIPAA).
• Subscriber has a change in employment status that affects their eligibility for the employer contribution
toward their employer-based group health plan.
• Subscriber’s dependent has a change in their own employment status that affects their eligibility or their
dependent’s eligibility for the employer contribution under their employer-based group health plan.
“Employer contribution” means contributions made by the dependent’s current or former employer toward
health coverage as described in the Treasury Regulation.
• Subscriber or their dependent has a change in enrollment under an employer-based group health plan
during its annual open enrollment that does not align with the SEBB Program’s annual open enrollment.
• Subscriber’s dependent has a change in residence from outside of the United States to within the United
States, or from within the United States to outside of the United States and that change in residence
resulted in the dependent losing their health insurance.
• A court order requires the subscriber or any other individual to provide insurance coverage for an eligible
dependent of the subscriber (a former spouse or former state-registered domestic partner is not an
eligible dependent).
• Subscriber or their dependent enrolls in coverage under Medicaid or a state Children’s Health Insurance
Program (CHIP), or the subscriber or their dependent loses eligibility for coverage under Medicaid or
CHIP.
• Subscriber or their dependent becomes eligible for a state premium assistance subsidy for SEBB health
plan coverage from Medicaid or CHIP.
• Subscriber’s dependent enrolls in Medicare or loses eligibility for Medicare.
Special open enrollment events that allow waiving medical enrollment and enrolling after
waiving
A school employee may waive SEBB medical during a special open enrollment if they are
enrolled in other employer-based group medical, a TRICARE plan, or Medicare.
Any of the following events may create a special open enrollment:
• School employee gains a new dependent due to:
70 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• Marriage or registering a state-registered domestic partnership.
• Birth, adoption, or when the school employee has assumed a legal obligation for total or partial
support in anticipation of adoption.
• A child becoming eligible as an extended dependent through legal custody or legal guardianship.
• School employee or their dependent loses other coverage under a group health plan or through health
insurance coverage, as defined by the HIPAA.
• School employee has a change in employment status that affects their eligibility for the employer
contribution toward their employer-based group medical.
• School employee’s dependent has a change in their own employment status that affects their eligibility or
their dependent’s eligibility for the employer contribution under their employer-based group medical.
“Employer contribution” means contributions made by the dependent’s current or former employer toward
health coverage as described in the Treasury Regulation.
• School employee or their dependent has a change in enrollment under an employer-based group medical
plan during its annual open enrollment that does not align with the SEBB Program’s annual open
enrollment.
• School employee’s dependent has a change in residence from outside of the United States to within the
United States, or from within the United States to outside of the United States and the change in
residence resulted in the dependent losing their health insurance.
• A court order requires the school employee or any other individual to provide a health plan for an eligible
dependent of the school employee (a former spouse or former state-registered domestic partner is not an
eligible dependent).
• School employee or their dependent enrolls in coverage under Medicaid or a state Children’s Health
Insurance Program (CHIP), or the school employee or their dependent loses eligibility for coverage under
Medicaid or CHIP. Note: A school employee may only return from having waived SEBB medical for the
events described in this paragraph. A school employee may not waive their SEBB medical for the events
described in this paragraph.
• School employee or their dependent becomes eligible for a state premium assistance subsidy for SEBB
health plan coverage from Medicaid or CHIP.
• School employee or their dependent becomes eligible and enrolls in a TRICARE plan or loses eligibility
for a TRICARE plan.
• School employee becomes eligible and enrolls in Medicare or loses eligibility for Medicare.
When Medical Coverage Ends
Termination dates
Medical coverage ends on the following dates:
• On the last day of the month when any enrollee ceases to be eligible. For a school board member this
includes when their elected or appointed term ends.
• On the date a medical plan terminates due to a change in contracted service area or when the group
policy ends. If that should occur, the subscriber will have the opportunity to enroll in another SEBB
medical plan.
• For a school employee and their dependents when the employment is terminated, medical coverage
ends when:
• The school employee resigns. If this is the case, medical coverage ends on the last day of the month
in which a school employee’s resignation is effective; or
• The SEBB organization or the employer group terminates the employment relationship. If this is the
case, medical coverage ends on the last day of the month in which the employer-initiated termination
is effective.
Note: If the SEBB organization deducted the school employee’s portion of the premium for SEBB insurance
coverage after the school employee was no longer eligible for the employer contribution, medical coverage ends
the last day of the month for which school employee premiums were deducted.
71 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• For a continuation coverage subscriber or a school board member who submits a request to terminate
medical coverage, enrollment in medical coverage will be terminated the last day of the month in which
the request was received online using Benefits 24/7 (one available) or by the SEBB Program ,or on the
last day of the month specified in the termination request, whichever is later. If the request is received on
the first day of the month, medical coverage will be terminated on the last day of the previous month.
A subscriber will be responsible for payment of any services received after the date medical coverage ends as
described above.
Final Premium Payments
Premium payments and applicable premium surcharges are not prorated during any month, for any reason, even
if an enrollee dies or asks to terminate their medical plan before the end of the month.
If the monthly premium or applicable premium surcharges remain unpaid for 30 days, the account will be
considered delinquent. A subscriber is allowed a grace period of 30 days from the date the monthly premiums or
applicable premium surcharges become delinquent to pay the unpaid premium balance and applicable premium
surcharges. If the subscriber’s premium balance or applicable premium surcharges remain unpaid for 60 days
from the original due date, the subscriber’s medical coverage (including enrolled dependents) will be terminated
retroactive to the last day of the month for which the monthly premiums and any applicable premium surcharges
were paid.
If An Enrollee is Hospitalized
An enrollee who is receiving covered services in a hospital on the date medical coverage ends will continue to be
eligible for covered services while an inpatient for the condition which the enrollee was hospitalized, until one of
the following events occur:
• According to this plan’s clinical criteria, it is no longer medically necessary for the enrollee to be an
inpatient at the facility.
• The remaining benefits available for the hospitalization are exhausted, regardless of whether a new
calendar year begins.
• The enrollee becomes covered under another agreement with a group health plan that provides benefits
for the hospitalization.
• The enrollee becomes enrolled under an agreement with another carrier that provides benefits for the
hospitalization.
This provision will not apply if the enrollee is covered under another agreement that provides benefits for the
hospitalization at the time medical coverage ends, except as set forth in this section, or if the enrollee is eligible
for SEBB Continuation Coverage as described in “Options for continuing SEBB medical coverage.”
Options for Continuing SEBB Medical Coverage
When medical coverage ends, the subscriber and their dependents covered by this medical plan may be eligible
to continue SEBB medical coverage during temporary or permanent loss of eligibility.
There are three options the subscriber and their dependents may qualify for when coverage ends.
• SEBB Continuation Coverage (COBRA)
• SEBB Continuation Coverage (Unpaid Leave)
• PEBB retiree insurance coverage
A subscriber also has the right to convert to individual medical insurance coverage with the plan when
continuation of group medical insurance coverage is no longer possible.
SEBB Continuation Coverage
The SEBB Program administers the following continuation coverage options to temporarily extend group
insurance coverage when the enrollee’s SEBB medical plan coverage ends due to a qualifying event:
• SEBB Continuation Coverage (COBRA) includes eligibility and administrative requirements under
federal COBRA laws and regulations. Some enrollees who are not qualified beneficiaries under federal
COBRA, may also qualify for SEBB Continuation Coverage (COBRA).
72 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• SEBB Continuation Coverage (Unpaid Leave) is an option created by the SEBB Program with wider
eligibility criteria and qualifying event types than COBRA.
An enrollee who qualifies for both types of SEBB Continuation Coverage (COBRA and Unpaid Leave) may enroll
in only one of these options. See “Continuation coverage enrollment” and the SEBB Continuation Coverage
Election Notice.
Premium payments for SEBB Continuation Coverage
If a subscriber enrolls in continuation coverage, the subscriber is responsible for timely payment of premiums and
applicable premium surcharges.
PEBB Retiree Insurance Coverage
A retiring school employee or a dependent becoming eligible as a survivor is eligible to continue enrollment or
defer enrollment in Public Employees Benefits Board (PEBB) insurance coverage if they meet procedural and
substantive eligibility requirements. See the PEBB Retiree Enrollment Guide for details.
Transitional Continuation Coverage
Non-represented educational service district (ESD) school employees and their dependents may gain temporary
eligibility for SEBB benefits, on a self-pay basis, if they meet the following criteria:
• A non-represented ESD school employee and their dependents who are enrolled in medical, dental, or vision
under a group plan offered by a SEBB organization on December 31, 2023, who lose eligibility because the
school employee is not eligible for SEBB benefits, may elect to continue existing enrollment in one or more of
the following SEBB benefits: medical, dental, or vision coverage. These benefits will be provided for a
maximum of 18 months.
• A dependent of a SEBB eligible non-represented school employee of an ESD who is enrolled in medical,
dental, or vision under a school employee's account on December 31, 2023, who loses eligibility because
they are not an eligible dependent may continue existing enrollment for a maximum of 36 months.
• A dependent of a non-represented school employee who is continuing medical, dental, or vision coverage
through an ESD on December 31, 2023, may elect to continue existing enrollment to finish out their remaining
months, up to the maximum number of months authorized by Consolidated Omnibus Budget Reconciliation
Act for a similar event, by enrolling in a medical, dental, or vision plan offered through the SEBB Program.
Contract Termination
Termination of the Group Contract for this plan completely ends all members’ coverage and all our obligations .
This plan is guaranteed renewable. However, this plan will automatically terminate if subscription charges aren’t
paid when due; coverage will end on the last day for which payment was made.
Family and Medical Leave Act of 1993
A school employee on approved leave under the federal Family and Medical Leave Act (FMLA) may continue to
receive the employer contribution toward SEBB benefits in accordance with the federal FMLA.
The SEBB organization or the employer group determines if the school employee is eligible for leave and the
duration of the leave under FMLA. The school employee must continue to pay their monthly premium contribution
and applicable premium surcharges during this period to maintain eligibility.
If a school employee exhausts the period of leave approved under FMLA, they may continue SEBB insurance
coverage by self-paying the monthly premium and applicable premium surcharges set by HCA, with no
contribution from the SEBB organization or the employer group. See “Options for continuing SEBB medical
coverage.”
Paid Family and Medical Leave Act
A school employee on approved leave under the Washington State Paid Family and Medical Leave (PFML)
Program may continue to receive the employer contribution toward SEBB benefits. The Employment Security
Department determines if the school employee is eligible for leave under PFML. The school employee must
continue to pay their monthly premium contribution and applicable premium surcharges during this period to
maintain eligibility.

73 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
If a school employee exhausts the period of leave approved under PFML, they may continue SEBB insurance
coverage by self-paying the monthly premium and applicable premium surcharges set by HCA, with no
contribution from the SEBB organization or the employer group. See “Options for continuing SEBB medical
coverage.”
Conversion of Coverage
An enrollee has the right to switch from SEBB group medical to an individual conversion plan offered by this plan
when they are no longer eligible to continue the SEBB group medical plan and are not eligible for Medicare or
covered under another group insurance coverage that provides benefits for hospital or medical care.
An enrollee must apply for conversion coverage and pay the first month’s premium no later than 31 days after
their group medical plan ends or within 31 days from the date the notice of termination of coverage is received,
whichever is later.
Evidence of insurability (proof of good health) is not required to obtain the conversion coverage. Rates, coverage,
and eligibility requirements of this conversion plan differ from those of the enrollee’s current group medical plan.
To receive detailed information on conversion options under this medical plan, call us at 1-800-807-7310 (TRS:
711).
General provisions for eligibility and enrollment
Payment of premiums during a labor dispute
Any school employee or dependent whose monthly premiums are paid in full or in part by the SEBB organization
or the employer group may pay premiums directly to HCA if the school employee’s compensation is suspended or
terminated directly or indirectly because of a strike, lockout, or any other labor dispute, for a period not to exceed
six months.
When the school employee’s compensation is suspended or terminated, HCA will notify the school employee
immediately, by mail at the last address of record, that the school employee may pay premiums as they become
due.
If coverage is no longer available to the school employee under this certificate of coverage, then the school
employee may be eligible to purchase an individual medical plan from this plan consistent with premium rates
filed with the Washington State Office of the Insurance Commissioner.
Appeal rights
Any current or former school employee of a SEBB organization or their dependent may appeal a decision
made by the SEBB organization regarding SEBB eligibility, enrollment, or premium surcharges to the SEBB
organization.
Any current or former school employee of an employer group that contracts with HCA for SEBB benefits, or
their dependent may appeal a decision made by an employer group regarding SEBB eligibility, enrollment, or
premium surcharges to the employer group.
Any enrollee may appeal a decision made by the SEBB Program regarding SEBB eligibility, enrollment, premium
payments, or premium surcharges to the SEBB Appeals Unit.
Any enrollee may appeal a decision regarding the administration of a SEBB medical plan by following the appeal
provisions of the plan, except when regarding eligibility, enrollment, and premium payment decisions.
Learn more at hca.wa.gov/sebb-appeals.
Relationship to law and regulations
Any provision of this certificate of coverage that is in conflict with any governing law or regulation of Washington
State is hereby amended to comply with the minimum requirements of such law or regulation.
.
74 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Contract Termination
No rights are vested under this plan. Termination of the Group Contract for this plan completely ends all
members’ coverage and all our obligations, except as provided under Extended Benefits; please see the How
Do I Continue Coverage? section below.
This plan is guaranteed renewable. However, this plan will automatically terminate if subscription charges aren’t
paid when due; coverage will end on the last day for which payment was made. This plan may also terminate as
indicated below.
The Group may terminate the Group Contract:
• Effective on any subscription charge due date, upon 30 days' advance written notice
• By rejecting in writing the contract changes we make after the initial term. The written rejection must reach us
at least 15 days before the changes are to start. The Group Contract will end on the last date for which
subscription charges were paid.
We may terminate the Group Contract, upon 30 days advance written notice to the Group if:
• The Group has performed an act or practice that constitutes fraud or made an intentional misrepresentation of
material fact under the terms of the coverage
• The Group fails to meet the minimum participation or contribution requirements stated in its signed application
• The Group no longer has any members who reside or work in Washington
• Published policies, approved by the Office of the Insurance Commissioner, have been violated
• There is a material breach of the Group Contract, other than non-payment
• Changes in or implementation of federal state laws that no longer permit the continued offering of the Group
Contract
• We discontinue this Group Contract, as allowed by law
• We are otherwise permitted to do so by law
For the timeliness of the delivery of our notice, please see Notices in Other Information About This Plan.
HOW DO I FILE A CLAIM?
Claims Other Than Prescription Drug Claims
Many providers will submit their bills to us directly. However, if you need to submit a claim for medical benefits to
us, follow the simple steps below.
Step 1
Complete a Subscriber Claim Form. A separate Subscriber Claim Form is necessary for each patient and each
provider. You can order extra Subscriber Claim Forms by calling Customer Service.
Step 2
Attach the itemized bill. The itemized bill must contain all of the following information:
• Names of the subscriber and the member who incurred the expense
• Identification numbers for both the subscriber and the Group (these are shown on the subscriber's identification
card)
• Name, address and IRS tax identification number of the provider
• Information about other insurance coverage
• Date of onset of the illness or injury
• Diagnosis or diagnosis code from the most current edition of the International Classification of Diseases
manual
• Procedure codes from the most current edition of the Current Procedural Terminology manual, the
Healthcare Common Procedure Coding manual, or the American Dental Association Current Dental
Terminology manual for each service
• Dates of service and itemized charges for each service rendered

75 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• If the services rendered are for treatment of an injury, the date, time, location and a brief description of the
event
Step 3
If you're also covered by Medicare, and Medicare is primary, you must attach a copy of the “Explanation of
Medicare Benefits.”
Step 4
Check that all required information is complete. Bills received won't be considered to be claims until all necessary
information is included.
Step 5
Sign the Subscriber Claim Form in the space provided.
Step 6
Mail your claims to us at the mailing address shown on the back cover of this booklet.
Prescription Drug Claims
To make a claim for covered prescription drugs, please follow these steps:
In-Network Pharmacies
For retail pharmacy purchases, you don't have to send us a claim. Just show your Premera Blue Cross ID card to
the pharmacist, who will bill us directly. If you don't show your ID card, you'll have to pay the full cost of the
prescription and submit the claim yourself.
For mail-order pharmacy purchases, you don't have to send us a claim, but you'll need to follow the instructions
on the order form and submit it to the address printed on the form. Please allow up to 14 days for delivery.
Out-Of-Network Pharmacies
You'll have to pay the full cost for new prescriptions and refills purchased at these pharmacies. You'll need to fill
out a prescription drug claim form, attach your prescription drug receipts and submit the information to the
address shown on the claim form.
If you need a supply of in-network mail-order pharmacy order forms or prescription drug claim forms, contact our
customer service department at the numbers shown on the back cover of this booklet.
Timely Filing
You should submit all claims within 90 days of the start of service or within 30 days after the service is completed.
We must receive claims:
• Within 365 days of discharge for hospital or other medical facility expenses, or within 365 days of the date the
expenses were incurred for any other services or supplies
• For members who have Medicare, within 90 days of the process date shown on the Explanation of Medicare
Benefits, whichever is greater
The plan won't provide benefits for claims we receive after the later of these 2 dates except when required by law.
COMPLAINTS AND APPEALS
If at any time you have questions regarding your healthcare, you may contact customer service for assistance.
They are here to serve you and answer questions.
If you disagree with a decision we made or feel dissatisfied, and would like us to formally review your concerns,
you can file a complaint or appeal with Premera.
What is a Complaint?
Other than denial of payment for medical services or nonprovision of medical services, a complaint is when you
are not satisfied with customer service, quality, or access to medical service, and you want to share it with
Premera.

76 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
How to file a complaint
For complaints received in writing, we will send a written response within 30 days.
What is an Appeal?
An appeal is a request to review a specific decision or an adverse benefit determination Premera has made.
An adverse-benefit determination means a decision to deny, reduce, terminate or a failure to provide or to make
payment, in whole or in part for services. This includes:
• A limitation on otherwise covered benefits
• A clinical review decision
• A decision that a service is experimental, investigative, not medically necessary or appropriate, or not
effective
• A decision related to compliance with protections against balance billing as defined by federal and state law
WHAT YOU CAN APPEAL
Claims and
Prior Authorization
Payment
Benefits or charges were not applied correctly, including a limit or
restriction on otherwise covered benefits.
Denied
Coverage of your service, supply, device or prescription was denied
or partially denied. This includes prior authorization denials. It also
includes denials of drugs not on the plan’s list of covered drugs. (See
Prescription Drug for details
APPEAL LEVELS
You have the right to two levels of appeals:
Appeal Level
What it means
Deadline to appeal
Level 1 (Internal)
This is your first appeal. Premera will
review your appeal.
180 days from the date you were notified
of our decision.
External
If we deny your Level 1 appeal, you
can ask for an Independent Review
Organization (IRO) to review your
appeal.
OR
You can ask for an IRO review if
Premera has not made a decision by
the deadline for the Level 1 appeal.
There is no cost to you for an external
appeal.
180 days from the date you were notified
of our Level 1 appeal decision.
OR
180 days from the date the response to
your Level 1 appeal was due, if you did
not get a response or it was late.
How to Submit an Appeal in Writing
Step 1.
Get the form
• Complete the Member Appeal Form, you can find it on
www.premera.com/sebb or call customer service to request a
copy.
If you need help submitting an appeal, or would like a copy of the
appeals process, call customer service at 800-807-7310 (TRS:711)
Call customer service at 800-807-7310 (TRS:711)
Send the details in writing to:
Premera Blue Cross
PO Box 91102
Seattle, WA 98111-9202
Send a fax to 425-918-5592

77 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Step 2.
Collect supporting
documents
• Collect any supporting documents that may help with your appeal.
This may include chart notes, medical records, or a letter from
your doctor. Within 3 working days, we will confirm in writing that
we have your request.
• If you would like someone to appeal on your behalf, including your
provider, complete a Member Appeal Form with authorization,
you can find it on www.premera.com/sebb. We can’t release
your information without this form.
Step 3.
Send in my appeal
To help process your appeal, be sure to complete the form and return
with any supporting documents.
Send your documents to:
Premera Blue Cross
Attn: Appeals Coordinator
PO Box 91102
Seattle, WA 98111-9202
Fax to 425-918-5592
Note: You may also call customer service to verbally submit an appeal.
If you would like to review the information used for your appeal, send us a request in writing to:
Premera Blue Cross
Attn: Appeals Coordinator
PO Box 91102
Seattle, WA 98111
Fax: 425-918-5592
Appeal Response Time Limits
We’ll review your appeal and send a decision in writing within the time limits below. The timeframes are based on
what the appeal is about, not the appeal level. At each level, Premera representatives who have not reviewed the
case before will review and make a decision. Medical review denials will be reviewed by a medical specialist.
Type of appeal
When to expect a response
Urgent appeals
No later than 72 hours. We will call, fax, or email you
with the decision, and follow up in writing
Pre-service appeals (a decision made by us
before you received services)
Within 14 days
Appeals of experimental and investigative
denials
Within 20 days
All other appeals
14-30 days
External appeals
• Urgent appeals within 72 hours
• Other IRO appeals within 15 days after the IRO gets
the information or 20 days from the date the IRO
gets your request

78 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
IF WE NEED MORE TIME
Except for urgent appeals, we can extend the time limits. We will notify you, if for good cause, more time is
needed. An extension cannot delay the decision beyond 30 days without your informed written consent.
WHAT IF YOU HAVE ONGOING CARE
Ongoing care is continuous treatment you are currently receiving, such as residential care, care for a chronic
condition, inpatient care and rehabilitation.
If you appeal a decision that affects ongoing care because we’ve determined the care is no longer medically
necessary, the plan will continue to cover your care during the appeal period. This continued coverage during the
appeal period does not mean that the care is approved. If our decision is upheld, you must repay all amounts the
plan paid for ongoing care during the appeal review.
WHAT IF IT'S URGENT
If your condition is urgent, you will get our response sooner. Please see the table above. Urgent appeals are
only available for services you are currently receiving or have not yet received.
Examples of urgent situations are:
• Your life or health is in serious danger, or a delay in treatment would cause you to be in severe pain that you
cannot bear, as determined by our medical professional or your treating physician
• You are requesting coverage for inpatient or emergency care that you are currently receiving
If your situation is urgent, you may ask for an expedited external appeal at the same time you request an
expedited internal appeal.
HOW TO ASK FOR AN EXTERNAL REVIEW
External reviews will be done by an Independent Review Organization (IRO).
Step 1.
Get the form
We’ll tell you about your right to an external review with the
written decision of your internal appeal.
• Complete the Independent Review Organization (IRO) Request
form, you can find it on www.premera.com/sebb or call customer
service to request a copy. You may also write to us directly to ask
for an external appeal.
Step 2.
Collect supporting
documents
• Collect any supporting documents that may help with your external
review. This may include medical records and other information.
• We’ll forward your medical records and other information to the
Independent Review Organization (IRO). We will notify you which
IRO was selected to review your appeal. If you have additional
information on your appeal, you may send it to the IRO directly
within five business days.
Step 3.
Send in my external review
request
To help process your external review, be sure to complete the form
and return with any supporting documents.
Send your documents to:
Premera Blue Cross
Attn: Appeals Coordinator
PO Box 91102
Seattle, WA 98111-9202
Fax to 425-918-5592
Note: You may also call customer service to verbally submit an external review request.
79 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
ONCE THE IRO DECIDES
For urgent appeals, the IRO will inform you and Premera immediately. Premera will accept the IRO decision.
If the IRO:
• Reverses our decision, we will apply their decision quickly
• Stands by our decision, there is no further appeal. However, you may have other steps you can take under
state or federal law, such as filing a lawsuit.
If you have questions about a denial of a claim or your appeal rights, you may call customer service at the number
listed on your Premera ID card. Contact Washington Consumer Assistance Program at any time during this
process if you have any concerns or need help filing an appeal.
Washington Consumer Assistance Program
5000 Capitol Blvd.
Tumwater, WA 98501
1-800-562-6900
E-mail: mailto:cap@oic.wa.gov.
ADDITIONAL INFORMATION ABOUT YOUR COVERAGE
Your benefit booklet provides you with detailed information about this plan’s benefits, limitations and exclusions,
how to obtain care and how to appeal our decisions.
You may also ask for the following information:
• How to access care under this plan, including from providers who do not contract with us. See How Providers
Affect Your Costs earlier in this booklet.
• Our confidentiality policies
• Your right to seek and pay for care outside of your plan. Note: Premera is not responsible for any services
provided outside of your plan.
• The plan's drug list, also called a "formulary"
• How we pay providers
• How providers’ payment methods help promote good patient care
• A statement of all benefit payments in each year that have been counted toward this plan’s benefit limitations,
visit, day, or dollar benefit maximums or other overall limitations
• How to file a complaint and a copy of our process for resolving complaints
• How to appeal decisions you don't agree with
• Documents, instruments and other information referred to in this Contract
• How to access specialists
• How to get prior authorization when needed
• How we monitor quality and performance, including accreditation status of our plans with national managed
care organizations
• Use of the health employer data information set (HEDIS) to track performance
• How to replace your ID card. Note: If coverage under your plan terminates, your ID card will no longer be valid.
If you want to receive this information, please go to our website. If you don’t have access to the Web, please call
customer service. Our Web address and phone numbers are shown on the back cover of this booklet.
Also, when you enrolled in this plan, you got information such as how to access our provider directory and
preferred drug lists. If you need this information again, please call customer service.
You may also ask customer service for more information about:
• Other healthcare plans we offer
• A description of the payment arrangements we use to pay providers
80 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
OTHER INFORMATION ABOUT THIS PLAN
This section tells you about how your Group's contract with us and this plan are administered. It also includes
information about federal and state requirements we must follow and other information we must provide to you.
Conformity With The Law
The Group Contract is issued and delivered in the state of Washington and is governed by the laws of the state of
Washington, except to the extent pre-empted by federal law. If any provision of the Group Contract or any
amendment thereto is deemed to be in conflict with applicable state or federal laws or regulations, upon discovery
of such conflict the Group Contract will be administered in conformance with the requirements of such laws and
regulations as of their effective date.
Entire Contract
The entire contract between the Group and us consists of all of the following:
• The contract face page and Standard Provisions
• The benefit booklet(s)
• The Group's signed application
• The Funding Arrangement Agreement between the Group and us
• All attachments, endorsements and riders included or issued hereafter
No agent or representative of Premera Blue Cross or any other entity is authorized to make any changes,
additions or deletions to the Group Contract or to waive any provision of this plan. Changes, alterations, additions
or exclusions can only be done over the signature of an officer of Premera Blue Cross.
Evidence Of Medical Necessity
We have the right to require proof of medical necessity for any services or supplies you receive before we provide
benefits under this plan. This proof may be submitted by you or on your behalf by your health care providers. No
benefits will be available if the proof isn't provided or acceptable to us.
The Group And You
Your Group is your representative for all purposes under this plan and not the representative of Premera Blue
Cross. Any action taken by the Group will be binding on you.
Healthcare Providers - Independent Contractors
All healthcare providers who provide services and supplies to a member do so as independent contractors. None
of the provisions of the contract between Premera and the Group are intended to create, nor shall they be
deemed or construed to create, any employment or agency relationship between us and the provider of service
other than that of independent contractors.
Intentionally False Or Misleading Statements
If this plan’s benefits are paid in error due to a member's or provider's commission of fraud or providing any
intentionally false or misleading statements, we’ll be entitled to recover these amounts. Please see the Right Of
Recovery provision later in this section.
And, if a member commits fraud or makes any intentionally false or misleading statements on any application or
enrollment form that affects the member's acceptability for coverage, we may, at our option:
• Deny the member's claim
• Reduce the amount of benefits provided for the member's claim
• Void the member's coverage under this plan (void means to cancel coverage back to its effective date, as if it
had never existed at all)
Finally, statements that are fraudulent, intentionally false or misleading on any group form required by us, that
affect the acceptability of the Group or the risks to be assumed by us, may cause the Group Contract for this plan
to be voided.
81 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Note: we cannot void your coverage based on a misrepresentation you made unless you have performed an act
or practice that constitutes fraud; or made an intentional misrepresentation of material fact that affects your
acceptability for coverage.
Member Cooperation
You're under a duty to cooperate with us in a timely and appropriate manner in our administration of benefits.
You're also under a duty to cooperate with us in the event of a lawsuit.
Newborn’s and Mother’s Health Protection Act
Group health plans and health insurance issuers generally may not, under federal law, restrict benefits for any
hospital length of stay in connection with childbirth for the mother or newborn child to less than 48 hours following
a vaginal delivery, or less than 96 hours following a cesarean section. However, federal law generally does not
prohibit the mother’s or newborn’s attending provider, after consulting with the mother, from discharging the
mother or her newborn earlier than 48 hours (or 96 hours as applicable.) In any case, group health plans and
health insurance issuers may not, under federal law, require that a provider obtain authorization from the plan or
the insurance issuer for prescribing a length of stay not in excess of the 48 hours (or 96 hours as applicable.)
Notice Of Information Use And Disclosure
We may collect, use, or disclose certain information about you. This protected personal information (PPI) may
include health information, or personal data such as your address, telephone number or Social Security number.
We may receive this information from, or release it to, health care providers, insurance companies, or other
sources.
This information is collected, used or disclosed for conducting routine business operations such as:
• Underwriting and determining your eligibility for benefits and paying claims. (Genetic information is not
collected or used for underwriting or enrollment purposes.)
• Coordinating benefits with other health care plans
• Conducting care management, or quality reviews
• Fulfilling other legal obligations that are specified under the Group Contract
This information may also be collected, used or disclosed as required or permitted by law
To safeguard your privacy, we take care to ensure that your information remains confidential by having a
company confidentiality policy and by requiring all employees to sign it.
If a disclosure of PPI isn't related to a routine business function, we remove anything that could be used to easily
identify you or we obtain your prior written authorization.
You have the right to request inspection and /or amendment of records retained by us that contain your PPI.
Please contact our customer service department and ask a representative to mail a request form to you.
Notice Of Other Coverage
As a condition of receiving benefits under this plan, you must notify us of:
• Any legal action or claim against another party for a condition or injury for which we provide benefits; and the
name and address of that party's insurance carrier
• The name and address of any insurance carrier that provides:
• Personal injury protection (PIP)
• Underinsured motorist coverage
• Uninsured motorist coverage
• Any other insurance under which you are or may be entitled to recover compensation
• The name of any other group or individual insurance plans that cover you
Notices
Any notice we're required to submit to the Group or subscriber will be considered to be delivered if it's mailed to
the Group or subscriber at the most recent address appearing on our records. We'll use the date of postmark in
determining the date of our notification. If you or your Group is required to submit notice to us, it will be
considered delivered 3 days after the postmark date, or if not postmarked, the date we receive it.
82 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Right Of Recovery
We have the right to recover amounts we paid that exceed the amount for which we're liable. Such amounts may
be recovered from the subscriber or any other payee, including a provider. Or, such amounts may be deducted
from future benefits of the subscriber or any of their dependents (even if the original payment wasn't made on that
member's behalf) when the future benefits would otherwise have been paid directly to the subscriber or to a
provider that does not have a contract with us.
In addition, if the contract for this plan is rescinded as described in Intentionally False Or Misleading
Statements, we have the right to recover the amount of any claims we paid under this plan and any
administrative costs we incurred to pay those claims.
Right To And Payment Of Benefits
Benefits of this plan are available only to members. Except as required by law, we won't honor any attempted
assignment, garnishment or attachment of any right of this plan. In addition, members may not assign a payee for
claims, payments or any other rights of this plan.
At our option only and in accordance with the law, we may pay the benefits of this plan to:
• The subscriber
• A provider
• Another health insurance carrier
• The member
• Another party legally entitled under federal or state medical child support laws
• Jointly to any of the above
Payment to any of the above satisfies our obligation as to payment of benefits.
Venue
All suits or legal proceedings brought against us by you or anyone claiming any right under this plan must be filed:
• Within 3 years of the date we denied, in writing, the rights or benefits claimed under this plan, or of the
completion date of the independent review process if applicable; and
• In the state of Washington or the state where you reside or are employed.
All suits or legal or arbitration proceedings brought by us will be filed within the appropriate statutory period of
limitation, and you agree that venue, at our option, will be in King County, the state of Washington.
Women's Health and Cancer Rights Act of 1998
Your plan, as required by the Women's Health and Cancer Rights Act of 1998 (WHCRA), provides benefits for
mastectomy-related services including all stages of reconstruction and surgery to achieve symmetry between the
breasts, prostheses, and complications resulting from a mastectomy, including lymphedemas. See Covered
Services.
Workers' Compensation Insurance
This contract doesn’t replace, affect or supplement any state or federal requirement for the Group to provide
workers’ compensation insurance, employer’s liability insurance or other similar insurance. When an employer is
required by law to provide or has the option to provide workers’ compensation insurance, employer’s liability
insurance or other similar insurance and doesn’t provide such coverage for its employees, the benefits available
under this plan won’t be provided for illnesses and/or injuries arising out of the course of employment that are or
would be covered by such insurance, unless otherwise excepted under the Exclusions section in this booklet.
83 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
DEFINITIONS
The terms listed throughout this section have specific meanings under this plan. As part of the routine operation
of this plan, we use our expertise and judgment to apply the terms of the contracts for making decisions in specific
benefits, eligibility and claims situations. For example, we use the medical judgment and expertise of Medical
Directors to determine whether claims for benefits meet the definitions below of “Medically Necessary” or
“Experimental/Investigational Services.” We also have medical experts who determine whether care is custodial
care or skilled care and reasonably interpret the level of care covered for your medical condition. This does not
prevent you from exercising rights you may have under applicable state or federal law to app eal, have
independent review or bring a civil challenge to any eligibility or claims determinations.
Adverse Benefit Determination
An adverse benefit determination means a decision to deny, reduce, terminate or a failure to provide or to make
payment, in whole or in part for services. This includes
• A member’s or applicant’s eligibility to be or stay enrolled in this plan or health insurance coverage
• A limitation on otherwise covered benefits
• A clinical review decision
• A decision that a service is experimental, investigative, not medically necessary or appropriate, or not effective
Accidental Injury
Physical harm caused by a sudden, unexpected event at a certain time an place. Accidental injury does not mean
any of the following:
• An illness, except for infection of a cut or wound
• Dental injuries caused by biting or chewing
• Over-exertion or muscle strains
Affordable Care Act
The Patient Protection and Affordable Care Act of 2010 (Public Law 111-148) as amended by the Health Care
and Education Reconciliation Act of 2010 (Public Law 111-152).
Ambulatory Surgical Center
A healthcare facility that’s licensed or certified as required by the state it operates in and that meets all of the
following:
• It has an organized staff of physicians.
• It has permanent facilities that are equipped and operated mainly for the purpose of performing surgical
procedures.
• It doesn’t provide inpatient services or accommodations.
Annual open enrollment
A period of time defined by HCA when a subscriber may change to another health plan offered by the SEBB
Program and make certain other account changes for an effective date beginning January 1 of the following year.
Applied Behavioral Analysis (ABA)
The design, implementation and evaluation of environmental modifications, using behavioral stimuli and
consequences, including direct observation, measurement and functional analysis of the relationship between
environment and behavior to produce socially significant improvement in human behavior or to prevent the loss of
an attained skill or function.
Autism Spectrum Disorders
Pervasive developmental disorders or a group of conditions having substantially the same characteristics as
pervasive developmental disorders, as defined in the current Diagnostic and Statistical Manual (DSM) published
by the American Psychiatric Association, as amended or reissued from time to time.
84 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Benefit
What this plan provides for a covered service. The benefits you get are subject to this plan’s cost shares.
Benefit Booklet
Benefit booklet describes the benefits, limitations, exclusions, eligibility and other coverage provisions included in
this plan and is part of the entire contract.
Calendar Year
The period of 12 consecutive months that starts each January 1 at 12:01 a.m. and ends on the next December 31
at midnight.
Clinical Trials
An approved clinical trial means a scientific study using human subjects designed to test and improve prevention,
diagnosis, treatment, or palliative care of cancer, or the safety and effectiveness of a drug, device, or procedure
used in the prevention, diagnosis, treatment, or palliative care, if the study is approved by the following:
• An institutional review board that complies with federal standards for protecting human research subjects and
• One or more of the following:
• The United States Department of Health and Human Services, National Institutes of Health, or its institutes
or centers
• The United States Department of Health and Human Services, United States Food and Drug Administration
(FDA)
• The United States Department of Defense
• The United States Department of Veterans’ Affairs
• A nongovernmental research entity abiding by current National Institute of Health guidelines
Community Mental Health Agency
An agency that’s licensed as such by the state of Washington to provide mental health treatment under the
supervision of a physician or psychologist.
Complication of Pregnancy
A medical condition related to pregnancy or childbirth that falls into one of these three categories:
• A condition of the fetus that needs surgery while still in the womb (in utero)
• A condition the mother has that is caused by the pregnancy. It is more difficult to treat because of the
pregnancy. These conditions are limited to:
• Ectopic pregnancy
• Hydatidiform mole/molar pregnancy
• Incompetent cervix that requires treatment
• Complications of administration of anesthesia or sedation during labor or delivery
• Obstetrical trauma, such as uterine rupture before onset or during labor
• Hemorrhage before or after delivery that requires medical or surgical treatment
• Placental conditions that require surgical intervention
• Preterm labor and monitoring
• Toxemia
• Gestational diabetes
• Hyperemesis gravidarum
85 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• Spontaneous miscarriage or missed abortion
• A disease the mother has during pregnancy that is not caused by the pregnancy. The disease is made
worse by pregnancy.
• A complication of pregnancy needs services that are more than the usual maternity services. This includes
care before, during, and after birth (normal or cesarean).
Congenital Anomaly
A marked difference from the normal structure of an infant's body part, that's present from birth.
Continuation Coverage
The temporary continuation of SEBB benefits available to enrollees under the Consolidated Omnibus Budget
Reconciliation Act (COBRA), the Uniformed Services Employment and Reemployment Rights Act (USERRA), or
SEBB policies
Cosmetic Services
Services that are performed to reshape normal structures of the body in order to improve or alter your appearance
and not primarily to restore an impaired function of the body.
Cost-Share
The member’s share of the allowed amount for covered services. Deductibles, copays, and coinsurance are all
types of cost-shares. See the Summary Of Your Costs to find out what your cost-share is.
Covered Service
A service, supply or drug that is eligible for benefits under the terms of this Plan.
Custodial Care
Any portion of a service, procedure or supply that is provided primarily:
• For ongoing maintenance of the member’s health and not for its therapeutic value in the treatment of an illness
or injury
• To assist the member in meeting the activities of daily living. Examples are help in walking, bathing, dressing,
eating, preparation of special diets, and supervision over self -administration of medication not requiring
constant attention of trained medical personnel
Dependent
An eligible spouse, state-registered domestic partner, child, or other eligible family member as described in the
“dependent eligibility” section of this certificate that is enrolled or eligible to be enrolled by this plan under the
subscriber’s account.
Detoxification
Active medical management of medical conditions due to substance intoxication or substance withdrawal. Active
medical management means repeated physical examination appropriate to the substance taken, repeated vital
sign monitoring, and use of medication to manage intoxication or withdrawal. Observation without active medical
management, or any service that is claimed to be detoxification but does not include active medical management,
is not detoxification.
Doctor (also called “Physician”)
A state-licensed:
• Doctor of Medicine and Surgery (MD)
• Doctor of Osteopathy (DO)
In addition, professional services provided by one of the following types of providers will be covered under this
plan, but only when the provider is providing a service within the scope of their state license; providing a service
or supply for which benefits are specified in this plan; and providing a service for which benefits would be payable
if the service were provided by a physician as defined above:
86 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• Chiropractor (DC)
• Dentist (DDS or DMD)
• Optometrist (OD)
• Podiatrist (DPM)
• Psychologist (PhD)
• Nurse (RN and ARNP) licensed in Washington state
Donor Human Milk
Human milk that has been contributed to a milk bank by one or more donors.
Effective Date
The date when your coverage under this plan begins.
Eligibility Waiting Period
The length of time that must pass before a subscriber or dependent is eligible to be covered under the Group’s
health care plan. If a subscriber or dependent enrolls under the Special Enrollment provisions of this plan or
enrolls on a date other than when first eligible to enroll, any period prior to such enrollment isn’t considered an
eligibility waiting period, unless all or part of the initial eligibility waiting period had not been met.
Emergency Medical Condition (also called “Emergency”)
A medical condition, mental health, or substance use disorder condition which manifests itself by acute symptoms
of sufficient severity, including, but not limited to, severe pain or emotional distress, such that a prudent
layperson, who possesses an average knowledge of health and medicine, could reasonably expect the absence
of immediate attention to result in 1) placing the health of the individual (or with respect to a pregnant member,
the member’s health or the unborn child) in serious jeopardy; 2) serious impairment to bodily functions; or 3)
serious dysfunction of any bodily organ or part.
Examples of an emergency medical condition are severe pain, suspected heart attacks and fractures. Examples
of a non-emergency medical condition are minor cuts and scrapes.
Emergency Service
• A medical screening examination to evaluate an emergency that is within the capability of the emergency
department of a hospital, including ancillary services (such as laboratory and radiology services) given in an
emergency department. Emergency services are also provided by a behavioral health emergency service
provider, including a crisis stabilization unit, triage facility, mobile rapid response crisis team, and an agency
certified by the Department of Health.
• Examination and treatment as required to stabilize a patient to the extent the examination and treatment are
within the capability of the staff and facilities available at a hospital. Stabilize means to provide medical,
mental health, or substance use disorder treatment necessary to ensure that, within reasonable medical
probability, no material deterioration of an emergency condition is likely to occur during or to result from the
transfer of the patient from a facility; and for a pregnant woman in active labor, to perform the delivery.
• Ambulance transport, as needed, in support of the services above.
Enrollee or Member (also called “You” and “Your”)
A person covered under this plan as a subscriber or dependent.
Essential Health Benefits
Benefits defined by the Secretary of Health and Human Services that shall include at least the following general
categories: ambulatory patient services, emergency services, hospitalization, maternity and newborn care, mental
health and substance use disorder services, including behavioral health treatment, prescription drugs,
rehabilitative and habilitative services and devices, laboratory services, preventive and wellness services and
chronic disease management and pediatric services, including oral and vision care. The designation of benefits
as essential shall be consistent with the requirements and limitations set forth under the Affordable Care Act and
applicable regulations as determined by the Secretary of Health and Human Services.
87 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Experimental/Investigational Services
A treatment, procedure, equipment, drug, drug usage, medical device or supply that meets one or more of the
following criteria:
• A drug or device which cannot be lawfully marketed without the approval of the U.S. Food and Drug
Administration and does not have approval on the date the service is provided.
• It is subject to oversight by an Institutional Review Board.
• There is no reliable evidence showing that the service is effective, in clinical diagnosis, evaluation,
management or treatment of the condition.
• It is the subject of ongoing clinical trials to determine its maximum tolerated dose, toxicity, safety or efficacy.
• Evaluation of reliable evidence shows that more research is necessary before the service can be classified as
equally or more effective than conventional therapies
Reliable evidence means only published reports and articles in authoritative medical and scientific literature and
assessments and coverage recommendations published by the Blue Cross Blue Shield Association Technical
Evaluation Center (TEC).
Explanation of Benefits
An explanation of benefits is a statement that shows what you will owe and what we will pay for healthcare
services received. It’s not a bill.
Facility (Medical Facility)
A hospital, skilled nursing facility, approved treatment facility for substance use disorder, state-approved
institution for treatment of mental or psychiatric conditions, or hospice. Not all health care facilities are covered
under this contract.
Group
The large employer that is a party to the Group Contract. A large employer is one that had an average of at least
51 common law employees on its normal work days in the preceding calendar year. It must also have at least 51
common law employees on the first day of the current contract term.
The Group is responsible for collecting and paying all subscription charges, receiving notice of additions and
changes to subscriber and dependent eligibility and providing such notice to us, and acting on behalf of its
employees and continuation coverage subscribers.
Health Care Authority (HCA)
The Washington State agency that administers the PEBB and SEBB Programs.
Home Health Agency
An organization that provides covered home health care services to a member.
Home Medical Equipment (HME)
Equipment ordered by a healthcare provider for everyday or extended use to treat an illness or injury. HME may
include: oxygen equipment, wheelchairs or crutches. This is also sometimes known as “Durable Medical
Equipment” or “DME”.
Hospice
A facility or program designed to provide a caring environment for supplying the physical and emotional needs of
the terminally ill.
Hospital
A healthcare facility that meets all of these criteria:
• It operates legally as a hospital in the state where it is located.
• It has facilities for the diagnosis, treatment and acute care of injured and ill persons as inpatients.
• It has a staff of providers that provides or supervises the care.
• It has 24-hour nursing services provided by or supervised by registered nurses.
88 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
A facility is not considered a hospital if it operates mainly for any of the purposes below:
• As a rest home, nursing home, or convalescent home
• As a residential treatment center or health resort
• To provide hospice care for terminally ill patients
• To care for the elderly
• To treat substance use disorder or tuberculosis
Illness
A sickness, disease or medical condition.
Injury
Physical harm caused by a sudden event at a specific time and place. It is independent of illness, except for
infection of a cut or wound.
In-Network Pharmacy (In-Network Retail/In-Network Mail Order Pharmacy)
A licensed pharmacy which contracts with us or our Pharmacy Benefit Manager to provide prescription drug
benefits.
In-Network Provider
A provider that is in one of the networks stated in the
How Providers Affect Your Costs
section.
Inpatient
Confined in a medical facility as an overnight bed patient.
Lifetime Maximum
The maximum amount that your insurance benefit will provide during your lifetime.
Long-term Care Facility
A nursing facility licensed under chapter 18.51 RCW, continuing care retirement community defined under RCW
70.38.025, or assisted living facility licensed under chapter 18.20 RCW.
Maternity Care
Health services you get during pregnancy (before, during, and after birth) or for any condition caused by
pregnancy. This includes the time during pregnancy and within 45 days following delivery.
Medical Equipment
Mechanical equipment that can stand repeated use and is used in connection with the direct treatment of an
illness or injury.
Medically Necessary and Medical Necessity
Services a provider, exercising prudent clinical judgment, would use with a patient to prevent, evaluate, diagnose
or treat an illness or injury or its symptoms. These services must:
• Agree with generally accepted standards of medical practice;
• Be clinically appropriate, in terms of type, frequency, extent, site and duration. They must also be considered
effective for the patient’s illness, injury or disease.
• Not be mostly for the convenience of the patient, physician, or other health care provider. They do not cost
more than another service or series of services that are at least as likely to produce equivalent therapeutic or
diagnostic results as to the diagnosis or treatment of that patient’s illness, injury or disease.
For these purposes, "generally accepted standards of medical practice" means standards that are based on
credible scientific evidence published in peer reviewed medical literature. This published evidence is recognized
by the relevant medical community, physician specialty society recommendations and the views of physicians
practicing in relevant clinical areas and any other relevant factors.
89 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Member (also called “You” and “Your”)
A person covered under this plan as a subscriber or dependent.
Mental Health Condition
A condition that is listed in the most recent edition of the Diagnostic and Statistical Manual of Mental Disorders
(DSM). This does not include conditions and treatments for substance use disorder.
Milk Bank
An organization that engages in the procurement, processing, storage, distribution, or use of human milk
contributed by donors.
Non-Contracted Provider
A provider is not in any network of Premera Blue Cross, Premera Blue Cross Blue Shield of Alaska, or the local
Blue Cross Blue Shield licensee.
Non-Participating Provider
A provider that is not in one of the provider networks stated in the How Providers Affect Your Costs section or
is not in any network of Premera Blue Cross, Premera Blue Cross Blue Shield of Alaska, or the local Blue Cross
Blue Shield licensee.
Orthodontia
The branch of dentistry which specializes in the correction of tooth arrangement problems, including poor
relationships between the upper and lower teeth (malocclusion).
Orthotic
A support or brace applied to an existing portion of the body for weak or ineffective joints or muscles, to aid,
restore or improve function.
Out-Of-Network Provider
A provider that is not in one of the provider networks stated in the How Providers Affect Your Costs section.
Outpatient
Treatment received in a setting other than as inpatient in a medical facility.
Outpatient Surgical Center
A facility that’s licensed or certified as required by the state it operates in and that meets all of the following:
• It has an organized staff of physicians
• It has permanent facilities that are equipped and operated primarily for the purpose of performing surgical
procedures
• It doesn’t provide inpatient services or accommodations
Pharmacy Benefit Manager
An entity that contracts with us to administer the Prescription Drug benefit under this plan.
Plan
The benefits, terms and limitations stated in this contract.
Prescription Drug
Any medical substance, including biological products, the label of which, under the Federal Food, Drug and
Cosmetic Act, as amended, is required to bear the legend: “Caution: Federal law prohibits dispensing without a
prescription.”
Benefits available under this plan will be provided for “off-label” use, including administration, of prescription drugs
for treatment of a covered condition when use of the drug is recognized as effective for treatment of such
condition by:

90 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• One of the following standard reference compendia:
• The American Hospital Formulary Service-Drug Information
• The American Medical Association Drug Evaluation
• The United States Pharmacopoeia-Drug Information
• Other authoritative compendia as identified from time to time by the Federal Secretary of Health and Human
Services or the Insurance Commissioner
• If not recognized by one of the standard reference compendia cited above, then recognized by the majority of
relevant, peer-reviewed medical literature (original manuscripts of scientific studies published in medical or
scientific journals after critical review for scientific accuracy, validity and reliability by independent, unbiased
experts)
• The Federal Secretary of Health and Human Services
“Off-label use” means the prescribed use of a drug that’s other than that stated in its FDA -approved labeling.
Benefits aren’t available for any drug when the U.S. Food and Drug Administration (FDA) has determined its use
to be contra-indicated, or for experimental or investigational drugs not otherwise approved for any indication by
the FDA.
Prior Authorization
Prior authorization is a process that requires you or a provider to follow before a service is given, to determine if
service is a covered service and meets the requirements for medical necessity, clinical appropriateness, level of
care, or effectiveness. You must ask for prior authorization before the service is delivered.
Provider
A person who is in a provider category regulated under Title 18 or Chapter 70.127 RCW to practice health care
related services consistent with state law. Such persons are considered health care providers only to the extent
required by RCW 48.43.045 and only to the extent services are covered by the provisions of this plan. Also
included is an employee or agent of such a person, acting in the course of and within the scope of their
employment.
Providers also include certain health care facilities and other providers of health care services and supplies, as
specifically indicated in the provider category listing below. Health care facilities that are owned and operated by
a political subdivision or instrumentality of the state of Washington and other such facilities are included as
required by state and federal law.
In states other than Washington, “provider” means health care practitioners and facilities that are licensed or
certified consistent with the laws and regulations of the state in which they operate, and that provide health care
services consistent with applicable state requirements.
In Washington State, covered licensed or certified categories of providers regulated under Title 18 and Chapter
70.127 RCW, will include the following, provided that the services they furnish are consistent with state law and
the conditions of coverage described elsewhere in this plan are met:
• Acupuncturists (LAc) (in Washington, also called East Asian Medicine Practitioners (EAMP)
• Audiologists
• Chiropractors (DC)
• Counselors
• Dentists (DDS or DMD)
• Denturists
• Dietitians and Nutritionists (D or CD, or CN)
• Home Health Care, Hospice and Home Care Agencies
• Marriage and Family Therapists
• Massage Practitioners (LMP)
• Midwives
• Naturopathic Physicians (ND)
91 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
• Nurses (RN, LPN, ARNP, or NP)
• Nursing Homes
• Occupational Therapists (OTA)
• Ocularists
• Opticians (Dispensing)
• Optometrists (OD)
• Osteopathic Physician Assistants (OPA) (under the supervision of a DO)
• Osteopathic Physicians (DO)
• Pharmacists (RPh)
• Physical Therapists (LPT)
• Physician Assistants (under the supervision of an MD)
• Physicians (MD)
• Podiatric Physicians (DPM)
• Psychologists
• Radiologic Technologists (CRT, CRTT, CRDT, CNMT)
• Respiratory Care Practitioners
• Social Workers
• Speech-Language Pathologists
The following health care facilities and other providers of health care services and supplies will be considered
health care providers for the purposes of this plan, as long as they're licensed or certified by the State (unless
otherwise stated) and the services they furnish are consistent with state law and the conditions of coverage
described elsewhere in this plan are met:
• Ambulance Companies
• Ambulatory Diagnostic, Treatment and Surgical Facilities
• Audiologists (CCC-A or CCC-MSPA)
• Birthing Centers
• Blood Banks
• Community Mental Health Centers
• Drug and Alcohol Treatment Facilities
• Medical Equipment Suppliers
• Hospitals
• Kidney Disease Treatment Centers (Medicare-certified)
• Psychiatric Hospitals
• Speech Therapists (Certified by the American Speech, Language and Hearing Association)
Board Certified Behavior Analysts (BCBAs) will be considered health care providers for the purposes of providing
applied behavior analysis (ABA) therapy, as long as both of the following are true: 1) They’re licensed when
required by the State in which they practice, or, if the State does not license behavior analysts, are certified as
such by the Behavior Analyst Certification Board, and 2) The services they furnish are consistent with state law
and the scope of their license or board certification. Therapy assistants/behavioral technicians/paraprofessionals
that do not meet the requirements above will also be covered providers under this plan when they provide ABA
therapy and their services are supervised and billed by a BCBA or one of the following state-licensed provider
types: psychiatrist, developmental pediatrician, pediatric neurologist, psychiatric nurse practitioner, advanced
nurse practitioner, advanced registered nurse practitioner, occupational or speech therapist, psychologist,
community mental health agency that is also state-certified to provide ABA therapy.
Psychiatric Condition
A condition listed in the current edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM). This
does not include conditions and treatments for substance abuse disorder.
92 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Public Employees Benefits Board (PEBB)
A group of representatives, appointed by the governor, who approves insurance benefit plans for employees and
their dependents, and establishes eligibility criteria for participation in insurance benefit plans.
Public Employees Benefits Board (PEBB) Program
The HCA program that administers PEBB benefit eligibility and enrollment.
Reconstructive Surgery
Is surgery:
• That restores features damaged as a result of injury or illness.
• To correct a congenital deformity or anomaly
Rehabilitation Therapy
Rehabilitation therapy services or devices are medical services or devices provided when medically necessary for
restoration of bodily or cognitive functions lost due to a medical condition.
Rehabilitation services include physical therapy, and speech-language therapy when provided by a state-licensed
or state-certified provider acting within the scope or their license. Therapy performed to maintain a current level of
functioning without documentation of significant improvement is considered maintenance therapy and is not a
rehabilitative service. Rehabilitative devices may be limited to those that have FDA approval and are prescribed
by a qualified provider.
School Employees Benefits Board (SEBB)
A group of representatives, appointed by the governor, who designs and approves insurance benefit plans for
school employees and their dependents, and establishes eligibility criteria for participation in insurance benefit
plans.
School Employees Benefits Board (SEBB) Organization
A public school district or educational service district or charter school established under Washington state statute
that is required to participate in benefit plans provided by the School Employees Benefits Board (SEBB).
School Employees Benefits Board (SEBB) Program
The program within HCA that administers insurance and other benefits for eligible school employees and eligible
dependents
Service Area
The area in which we directly operate provider networks, which includes all of Washington State (except for Clark
County) and Alaska.
Services
Procedures, surgeries, consultations, advice, diagnosis, referrals, treatment, supplies, drugs, devices,
technologies or places of service.
Skilled Nursing Care
Medical care ordered by a physician and requiring the knowledge and training of a licensed registered nurse.
Skilled Nursing Facility
A medical facility providing services that require the direction of a physician and nursing supervised by a
registered nurse, and that’s approved by Medicare or would qualify for Medicare approval if so requested.
Spouse
Someone who is legally married to the subscriber. A spouse can also be the subscriber’s domestic partner.
93 Standard PPO Plan (Non-Grandfathered)
January 1, 2023
4018486
Subscriber
A school employee or continuation coverage enrollee who has been determined eligible and is enrolled in this
plan, and is the individual to whom the SEBB Program or We will issue notices, information, requests, and
premium bills on behalf of an Enrollee.
Subscription Charges
The monthly rates we establish as consideration for the benefits offered under this contract.
Substance Use Disorder Conditions
They are substance-related disorders included in the most recent edition of the Diagnostic and Statistical Manual
of Mental Disorders published by the American Psychiatric Association. Substance use disorder is an addictive
relationship with any drug or alcohol characterized by a physical or psychological relationship, or both, that
interferes on a recurring basis with an individual's social, psychological, or physical adjustment to common
problems. Substance use disorder does not include addiction to or dependency on tobacco, tobacco products, or
foods.
Urgent Care
Treatment of unscheduled, drop-in patients who have minor illnesses and injuries. These illnesses or injuries
need treatment right away, but they are not life-threatening. Examples are high fevers, minor sprains and cuts,
and ear, nose and throat infections. Urgent care is provided at a medical facility that is open to the public and has
extended hours.
Virtual Care
Healthcare services provided through the use of online technology, telephonic and secure messaging of member
initiated care from a remote location (e.g. home) or an originating site with a provider that is diagnostic and
treatment focused. Originating site: Hospital, Rural health clinic, federally qualified health center, physician’s or
other health care providers office, community mental health center, skilled nursing facility, home or renal dialysis
center, except an independent renal dialysis center.
Visit
A visit is one session of consultation, diagnosis, or treatment with a provider. We count multiple visits with the
same provider on the same day as one visit. Two or more visits on the same date with different providers count as
separate visits.
We, Us and Our
Premera Blue Cross in the state of Washington, and Premera Blue Cross Blue Shield of Alaska in the state of
Alaska.

Where To Send Claims
MAIL YOUR CLAIMS TO
Premera Blue Cross
7001 220th St. SW
Mountlake Terrace, WA 98043-2124
PRESCRIPTION DRUG CLAIMS
Mail Your Prescription Drug Claims To
Contact the Drug Benefit Manager At
Express Scripts
ATTN: Commercial Claims
PO Box 14711
Lexington, KY 40512-4711
1-800-391-9701
www.express-scripts.com
Customer Service
Mailing Address
Phone Numbers
Premera Blue Cross
7001 220th St. SW
Mountlake Terrace, WA 98043-2124
Local and toll-free number:
1-800-807-7310
Physical Address
Local and toll-free TRS number:
711
7001 220th St. S.W.
Mountlake Terrace, WA 98043-2124
Care Management
Prior Authorization And Emergency Notification
Premera Blue Cross
7001 220th St. SW
Mountlake Terrace, WA 98043-2124
Local and toll-free number:
1-800-807-7310
Fax: 1-800-843-1114
Complaints And Appeals
Premera Blue Cross
Attn: Appeals Coordinator
PO Box 91102
Seattle, WA 98111-9202
Fax: (425) 918-5592
BlueCard
Website
1-800-810-BLUE(2583)
Visit our website www.premera.com/sebb
for information and secure online access to
claims information
Premera Blue Cross is an Independent Licensee of the Blue Cross Blue Shield Association
