
Long-Term Care Insurance Fraud,
Waste and Abuse Risk Management
A Survey of Industry Perspectives
June 2019

2
Copyright © 2019 Society of Actuaries
Long-Term Care Insurance Fraud, Waste and Abuse Risk Management
A Survey of Industry Perspectives
Caveat and Disclaimer
This study is published by the Society of Actuaries (SOA) and contains information from a variety of sources. It may or may not reflect the experience of any
individual company. The study is for informational purposes only and should not be construed as professional or financial advice. The SOA does not
recommend or endorse any particular use of the information provided in this study. The SOA makes no warranty, express or implied, or representation
whatsoever and assumes no liability in connection with the use or misuse of this study.
Copyright © 2019 by the Society of Actuaries. All rights reserved.
AUTHORS
Eileen J. Tell
Karen Smyth
Robert Eaton
SPONSOR
Long Term Care Insurance Section
Project Oversight
Group
Paul Colasanto
Perry Kupferman
Shawna Meyer
Rebecca Tipton

3
Copyright © 2019 Society of Actuaries
CONTENTS
Abstract
RESEARCH OBJECTIVES .............................................................................................................................................. 5
Expectations ............................................................................................................................................................. 5
RESEARCH METHODOLOGY ....................................................................................................................................... 7
Threats and Types of Fraud ........................................................................................................................................ 9
Industry Effectiveness, Tools and Resources ........................................................................................................... 10
Referral and Detection .............................................................................................................................................. 13
Relief and Resolution ................................................................................................................................................ 14
Regulatory Issues ...................................................................................................................................................... 16
DISCUSSION ............................................................................................................................................................ 19
APPENDIX: FULL SURVEY ......................................................................................................................................... 21
About The Society of Actuaries ............................................................................................................................... 22

4
Copyright © 2019 Society of Actuaries
ABSTRACT
Long-Term Care Insurance Fraud, Waste and Abuse Risk Management
A Survey of Industry Perspectives
The Society of Actuaries’ (SOA) Long Term Care (LTC) Section Council in 2018 approved
an initiative to survey LTC companies on their perspectives and practices regarding LTC
claims fraud, waste and abuse. There are many stakeholders who stand to benefit from a
better understanding of the risks posed by LTC claims fraud, waste and abuse risk and the
best practice strategies to address those risks:
1.
Policyholders.
When LTC insurance policyholders seek only legitimate or
contractual claims on their policy, LTC insurance companies are more likely to
remain financially healthy and thus better able to pay all future LTC insurance
claims. Conversely, LTC insurance claims fraud, waste and abuse may require
insurance companies to seek remunerative premium rate increases across all
policyholders.
2.
State insurance regulators.
Regulators wish to understand the difficulties facing
insurance companies. Some state insurance departments have investigative units
to combat fraud, waste and abuse, and would benefit from understanding
insurance company perspectives on this risk.
3.
Long-term care insurance companies.
LTC insurance companies wish to honor
legitimate and contractual claims while remaining financially viable. Claims fraud,
waste and abuse tend to increase claims and threaten future financial health.
4.
Reinsurance companies.
Similar to LTC insurance companies, reinsurance
companies face financial difficulties from claims fraud, waste, and abuse. Typically
reinsurers face this exposure from many insurance companies and many
geographies.
5.
Downstream industry participants.
Other parties such as third-party claims
administrators, care providers and state insurance guarantee funds also have
some stake in LTC claims fraud, waste and abuse.
This survey is intended to share insurance company risk management practices and
perspectives, so that these stakeholders may have a common understanding when
discussing fraud, waste and abuse in LTC insurance claims.

5
Copyright © 2019 Society of Actuaries
RESEARCH OBJECTIVES
The Society of Actuaries (SOA) Long Term Care (LTC) Section conducted a survey of the
leading LTC insurers’ management and perspectives of fraud, waste and abuse as it
relates to the adjudication and payment of benefits under long-term care insurance
contracts. The intent was to survey those long-term care insurers representing the
majority of in-force LTC policies—inclusive of those entities continuing to issue new
business and those managing closed blocks.
Definitions
For the purpose of responding to the survey, the following definitions were employed:
•
Fraud.
The intentional misuse of information to persuade another to part with
something of value or to surrender a legal right. It could also be an act of planned
deception or misrepresentation.
•
Waste.
To use, consume, spend or expend thoughtlessly or carelessly.
•
Abuse.
Providing information or documentation for a health care claim in a
manner that improperly uses program resources for personal gain or benefit, yet
without sufficient evidence to prove criminal intent.
Broadly speaking, the research objectives were:
• To understand companies’ perspectives with regard to key drivers of fraud, waste
and abuse and their opinions of the current and potentially available tools they
have for detection, prevention and recovery.
• To better understand the concerns companies have with their efforts to address
fraud, waste and abuse.
• To identify ways the industry can improve its relationship with regulators in
support of best practices for fraud prevention, detection and recovery.
Expectations
The SOA Long Term Care Section believes the issues identified in this report may serve as
a catalyst to educate both the industry and the regulatory community about the
challenges facing the LTC insurance industry to the extent that these findings generate
interest in action.

6
Copyright © 2019 Society of Actuaries
Insurance fraud is one of the most costly white-collar crimes in America today. Insurance
fraud is a crime in 48 states, plus the District of Columbia (DC). Forty-one states, plus DC
have an insurance fraud bureau charged with investigating and handling multiple lines of
insurance—including LTC. Most other lines of business have a much longer history of
paying claims than the LTC insurance industry and so too, a much longer history of
detecting, preventing and managing incidents of fraud, waste and abuse. It would be
naïve to believe that fraud, waste and abuse haven’t found their way into this industry.
By bringing to light industry concerns, experiences and perspectives, this survey may help
us identify new tools and strategies employed by other industries and to engage
regulators to help us with future prevention, detection and mitigation strategies.
The SOA supports thoughtful efforts to raise awareness of industry efforts surrounding
policy abuse and fraud to the regulatory community.

7
Copyright © 2019 Society of Actuaries
RESEARCH METHODOLOGY
Sample and Response Rate
. The Survey Team (“we,” “our”) gathered insights into fraud,
waste and abuse by issuing a web-based survey to the senior actuary or business practice
leader at nineteen (19) leading LTC insurers. One company reported no longer writing
business, another did not administer its own block, and two others had combined books
of business. Another was unable to participate for compliance reasons, for a remaining
viable sample of fifteen (15) companies able to respond. A total of thirteen (13)
companies completed the survey, for a response rate of 87%.
Questionnaire Development.
The Survey Team working group was formed in spring 2018
to begin development of the research questionnaire. To that end, ideas were collected
for areas of interest and concern from which the survey questionnaire would be built. In
May 2018, the Survey Team sent out a single-item questionnaire to members of the
Long-Term Care Anti-Fraud Forum (an inter-company effort focused on identifying and
sharing policies, procedures, tools and techniques, which may help with the prevention,
identification and mitigation of fraudulent long-term care insurance claims). The
questionnaire asked simply, “What questions should the Society of Actuaries ask when
surveying the long-term care insurance industry as it relates to LTC fraud, waste and
abuse?” Fifteen (15) companies responded, providing a wide range of questions of
interest to them. Many of the companies provided between five to seven questions each.
We analyzed the areas of interest expressed from that outreach, and sorted the
questions into key domains representing fraud, waste and abuse prevention, detection,
recovery and questions about the philosophical approach and the interface between
industry and the regulatory community. The Survey Team refined these items into a
questionnaire that would address the key research objectives without undue respondent
burden. The working group reviewed each draft of the survey to work toward the best
possible final draft.
We sent a pre-test version of the survey to three (3) volunteers from the industry’s Long-
Term Care Anti-Fraud Forum. We incorporated this feedback into the final questionnaire.
In the end, the survey comprised 30 questions, mostly closed-category responses. Survey
Monkey gave the survey a “great” rating for ease of completeness and an estimated
completion time of 15 minutes. Based on results, actual survey completion times ranged
from 7 minutes to 36 minutes.
We distributed the survey with an explanatory cover letter from the SOA in mid-
September 2018. We send periodic reminders and follow-up by both e-mail and
telephone. The Survey Team closed the data collection on January 15, 2019, and tallied
the responses.
8
Copyright © 2019 Society of Actuaries
Profile of Respondents
The respondents represent companies of all sizes:
• About 17% have less than 50,000 policies in force.
• Roughly 8% have between 50,000 and 99,999 insureds.
• Half the companies have blocks of business of 100,000 to 249,999 policies.
• Twenty-five percent (25%) have larger blocks of business.
Most often, the survey was completed by a company representative affiliated with the
business area of claims, either exclusively (five respondents) or in association with
actuarial (two respondents) or operations (two respondents). The remaining respondents
cited operations (2), actuarial (1) or corporate (1) as the business area they represent.
The responding companies also varied in terms of how long they have been writing LTC
policies, from as little as 10 years to several companies with more than 30 years of
experience. (See Table 1.)
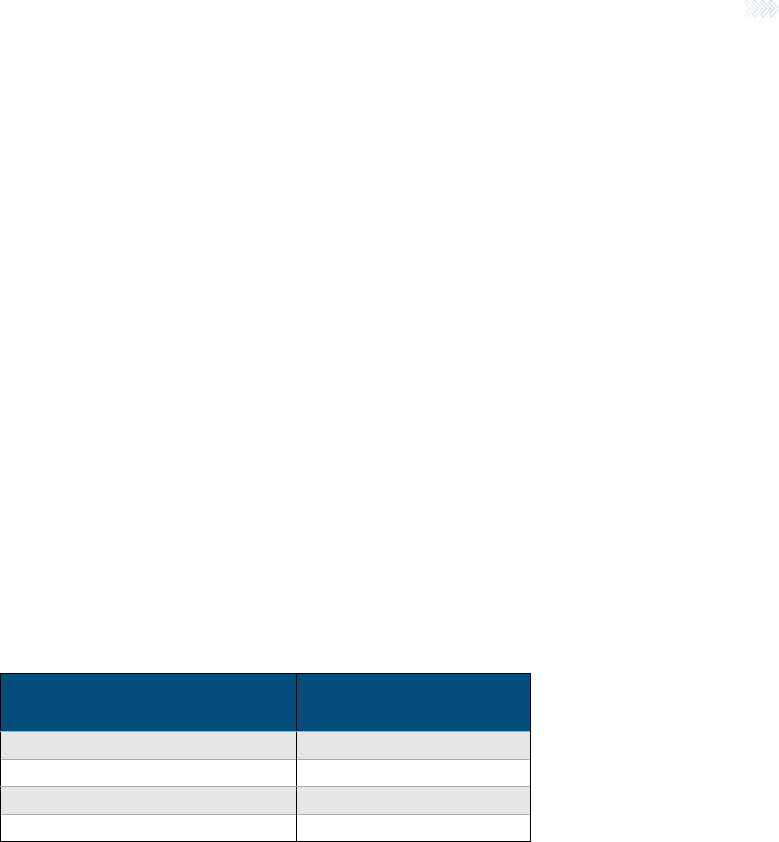
Table 1
NUMBER OF YEARS WRITING LTC POLICIES
Years in the Business*
Number of Responding
Companies
10 years
1
More than 20 years
3
More than 25 years
3
More than 30 years
6
*Question was open-ended so companies could respond as they chose.
9
Copyr
ight © 2019 Society of Actuaries
FINDINGS
Threats and Types of Fraud
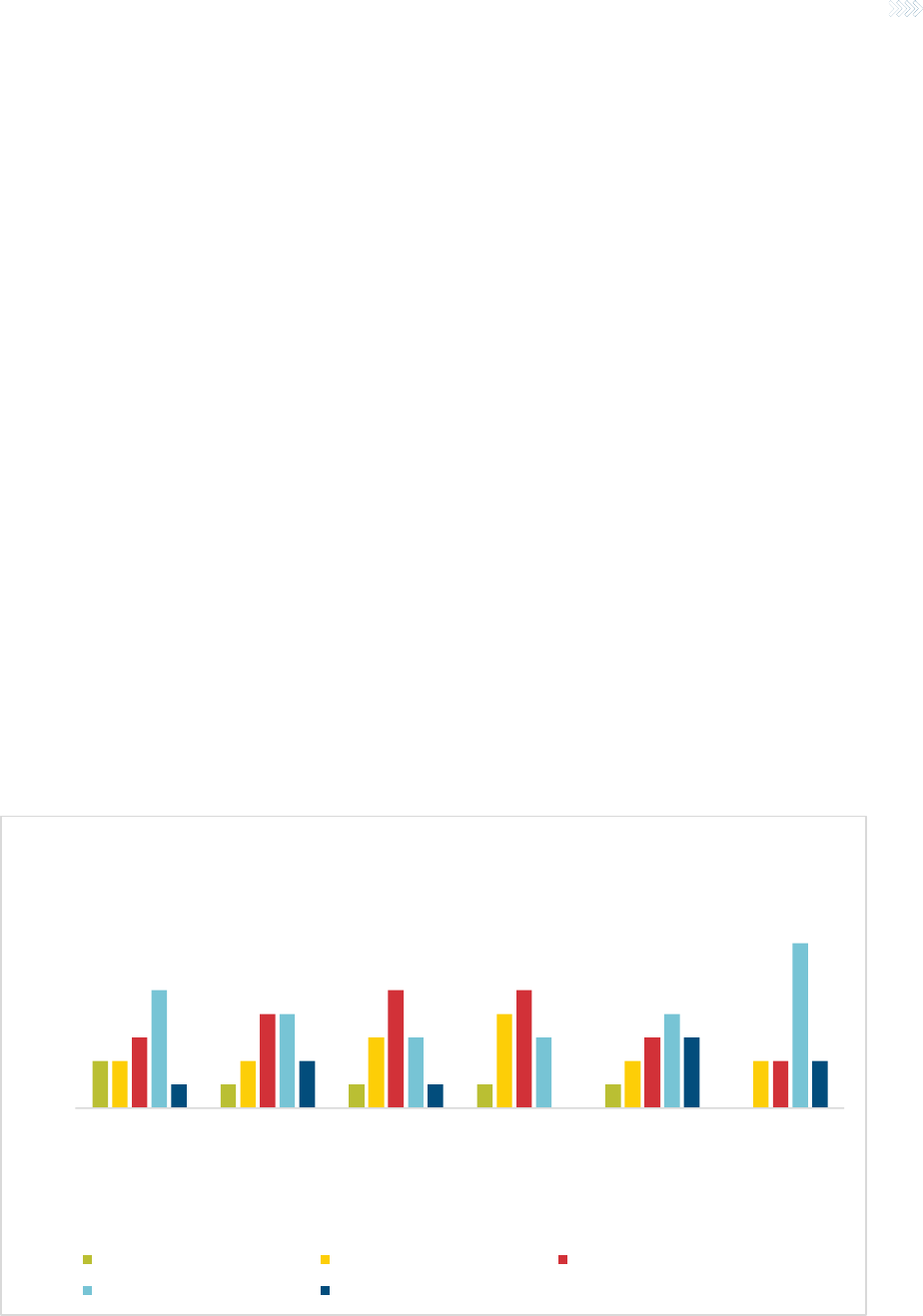
As a starting point, companies were asked to identify how significant to their company’s
overall experience were each of several different types and sources of fraud, waste and
abuse (FWA). In general, they were asked about claimant versus provider
misrepresentation and about the type of misrepresentations made, specifically about the
nature of loss or about services and billing. (See Figure 1.)
Claimant misrepresentation of loss received the highest score, with 15% of respondents
citing it as a very significant source of FWA. We note that the misrepresentation could
also include actions driven by family members, with or without the knowledge or consent
of the claimant. In contrast, only approximately 7% of respondents gave this high a rating
to any of the other sources. Combining the top two categories of significance (a score of
4 or 5 on a 5-point scale), provider misrepresentation of services and billing was cited by
38.5% of companies as a significant source of FWA. Respondents saw very little collusion
between providers and claimants as a source of fraud, waste and abuse experience.
In contrast, looking at the combination of “not very significant” and “not at all
significant,” just under half of the responding companies do not see claimant or provider
misrepresentation of loss as a significant source of potential FWA.
Figure 1
SIGNIFICANCE OF FWA TO LTC EXPERIENCE - See question 4 on page 23 for full X-axis category labels
0.0%
10.0%
20.0%
30.0%
40.0%
50.0%
60.0%
Claimant…
Provider…
Claimant…
Provider…
Collusion between…
Collusion between…
How significant to your company's experience are these
sources of potential fraud, waste, and abuse?
Very Significant Somewhat Significant Neither Significant or Insignificant
Not very Significant Not at all Significant

10
Copyright © 2019 Society of Actuaries
When asked to rank each type of FWA in order of importance to their company’s overall
experience, the top response with 54% of companies citing it, is “claimants who
misrepresent impairments in an attempt to satisfy benefit eligibility.” This speaks to the
importance of strong protocols for determining benefit eligibility and appropriate
schedules for recertification. Ranking second, with 23%, is “providers billing for services
not rendered.”
With regard to the role that the location of the claim plays in FWA, 100% of the
responding companies identified “informal home care claims (e.g., independent provider
or family member)” as the largest portion of potential FWA referrals or investigations.
We note that some policies allow family members to provide informal care while others
do not. Additionally, with regard to claim type, insurers are more concerned about
functional impairment claims (54%) than cognitive impairment (23%), medical necessity
(15%) or other benefit triggers (8%). The low level of concern with medical necessity
triggers likely stems more from their extremely low prevalence in today’s products than
from the nature of the benefit trigger, although the survey did not probe on that concept
specifically.
Finally, the survey asked about other situations related to a claim that might escalate the
potential for FWA. Assignment of benefits was cited by 54% of respondents as the top
reason. This makes sense because when the home care provider is paid directly, the
claimant or their family does not have the opportunity to review the bill and verify that
the charges being submitted accurately reflect the services provided to them. Just under
39% of respondents found that a rate increase was a potential trigger for an escalation in
FWA activity. Only 15% felt that a power of attorney situation posed a risk and 23% felt
that none of these factors were relevant. Other factors mentioned include having a
family member as a care provider or being in premium waiver status.
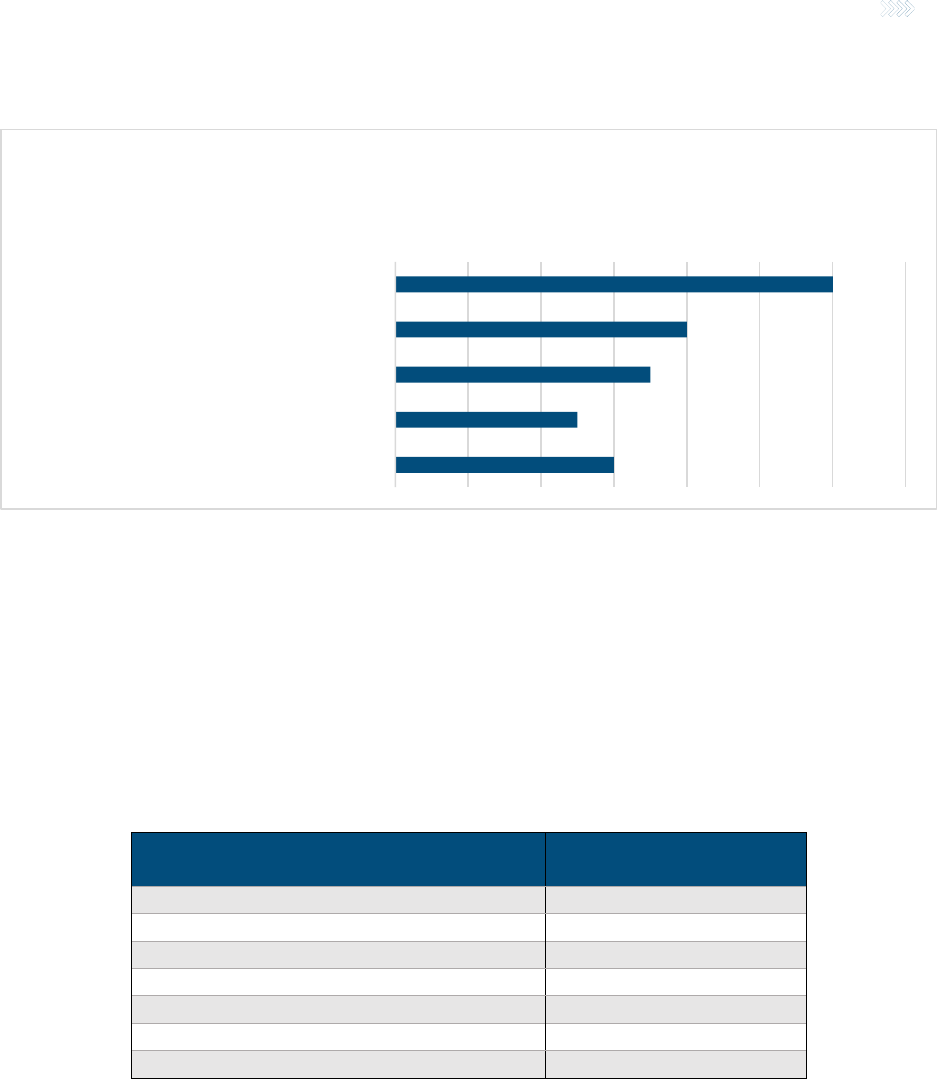
Industry Effectiveness, Tools and Resources
Companies may employ a wide variety of tools and practices in addressing fraud, waste
and abuse. We asked LTC insurers about some strategies that are more typically used in
other product lines that might have some applicability to LTC insurance. Assuming that
whatever regulatory changes would be needed to allow insurers to use these tools could
be obtained, we asked them to assess whether they have or would consider these
approaches. Results are summarized in Table 2.
The largest percent of carriers are already using required proof of payment for expenses
incurred (77%) and electronic tools that verify visits (46%) to validate claims. The top two
tools not currently being used but which a significant share of companies say they would
consider are a database similar to MIB where carriers can report and check suspected

11
Copyright © 2019 Society of Actuaries
fraudulent claimants and/or providers (85% would consider) and gathering forensic data
on mobile devices (54% would consider).
Table 2
TYPICAL PRACTICES TO COMBAT FWA IN LTC INSURANCE
Tool
Have
Considered
Would
Consider
Might
Consider
Would Not
Consider
Not
Familiar
Enough
to Know
Requiring proof of payment for
expenses incurred
77%
24%
—
—
—
Use of electronic visit verification tools
46%
46%
—
—
8%
Recorded interviews
31%
38%
31%
—
—
Pursuing a declaratory judgment
31%
23%
15%
8%
23%
Using field claim consultants to conduct
in-person claimant interviews to
complete claim forms
31%
31%
23%
15%
—
Examinations under oath
15%
38%
23%
8%
15%
MIB-like database for screening for
prior fraudulent claim activity
8%
85%
—
8%
—
Gathering forensic data on mobile
devices
0%
54%
15%
15%
15%
With regard to evaluating its efficacy at handling fraud, waste and abuse, the industry
does not give itself very good grades. None of the respondents feel that the industry is
either very or extremely effective. Just over half (54%) feel it is somewhat effective, and
39% say it is either not so effective or not at all effective.
The primary challenge to industry’s ability to effectively address these issues, cited by just
under 40% of respondents, seems to be the state of the knowledge, training and
technology to address fraud, waste and abuse. Companies feel they are still in the
learning and building phase with regard to these tools. Just under one-fourth of
respondents cite concern with either a lack of resources to address these issues or the
lack of compliance and regulatory support for taking action when fraud is identified. Only
a small portion of respondents (15%) feel that company concern with negative PR gets in
the way of effectively addressing fraud, waste and abuse. (See Figure 2.)

12
Copyright © 2019 Society of Actuaries
Figure 2
LTC INDUSTRY EFFECTIVENESS AT ADDRESSING FWA
Survey respondents had many suggestions for how groups such as SOA, ILTCI, the LTC
Anti-Fraud Forum, AHIP, ACLI and others might help industry address fraud, waste and
abuse. Key among the suggestions was education for all stakeholders, including
education within and across companies and education aimed specifically at regulators.
Some of the specific suggestions included in the following:
• Continue to illustrate and present different solutions and approaches; help
quantify the needs and the benefits of a FWA program.
• Highlight case studies and convene special discussion groups. Encourage
investigative vendors to participate.
• Meet more often as an industry to discuss fraud and ways to address it.
• Expand the conversation on this important topic.
• Increase both consumer and regulator awareness of the problem and its financial
impact.
• Lobby for state funds to address this issue and educate regulators.
• Advocate for regulatory changes to strengthen industry ability to enforce
contracts.
How effective is the industry at addressing fraud,
waste, and abuse?
Don't know/not sure Somewhat effective Not so effective Not at all effective

13
Copyright © 2019 Society of Actuaries
• Continue to support ongoing education for insurers, LTC vendors and state
insurance fraud departments.
Referral and Detection
Companies responded to nine questions regarding the referral and detection of FWA.
When asked how FWA is detected, companies signified that a few methods that were
widely used as shown in Table 3.
Table 3
REFERRAL AND DETECTION OF FWA
Detection Method
% of
Respondents
Red flags that staff are trained to
look for
100%
Secondary review by senior
claim staff, management, law
92%
Internal quality assurance
77%
When asked an open-ended question about the most important controls that companies
(or their TPAs) have in place to help prevent FWA, companies responded with a few key
themes:
• Data analytics
• Surveillance
• Electronic visit verification (EVV) on home health care invoices
• Training programs for claims and fraud analysts
Companies described the following new or creative methods they use to detect
fraudulent activity:
• High-risk scenario data profile development
• Social media searches
Companies indicated that staff are trained to spot potentially fraudulent activity. All of these
used red flag lists, and the majority employed on-the-job training of staff, as shown in Table 4.

14
Copyright © 2019 Society of Actuaries
Table 4
HOW STAFF ARE TRAINED
How Are Staff Trained?
%
Respondents
Red flag lists
100.0%
On the job training
92.3%
Formal training program
76.9%
Case illustrations
53.8%
All companies reported using surveillance to detect or investigate potential FWA, and a majority
of companies search social media in their investigations. Only three of the 13 respondents use
predictive analytics to help identify potential FWA. All respondents using predictive analytics
indicated that it is still too soon to tell whether or not the results are satisfactory.
For the eight respondents who have a dedicated fraud hotline, only two of them found the
hotline to be “somewhat effective”, with the rest indicating that the hotline was “not so
effective” (5) or “not at all effective” (1).
Finally, respondents were asked about the most important aspect of working with investigative
firms in pursing FWA. The following themes summarize the companies’ responses:
• Operate ethically / within compliance and regulatory laws and guidelines
• Expertise and knowledge of the LTC industry
• Communication: specific, clear and frequent
• Surveillance: interpretation and geographical reach
Relief and Resolution
Companies were asked about how confirmed cases of FWA were most typically resolved and
what types of relief were used. Respondents were asked to report all the actions that apply,
since they may take more than one action on a given claim or different actions for different
situations. Figure 3 shows that nearly all (92%) of the companies terminate the claim and just
under two-thirds (61%) will recover payments against the policy. Over half (54%) provide a
return of premium and end the policy, and just under half (46%) file a declaratory action against
the policyholder for rescission or policy surrender when FWA is discovered.
15
Copyright © 2019 Society of Actuaries
Figure 3
TYPE OF RELIEF USED FOR FWA
When asked which type of relief these companies use most often, more than half (53.8%) would
terminate the claim and just under one-third (30.8%) recover payments made against the policy.
Less than 10% give premiums back and end the policy.
Companies indicated other factors outside of the strength of the case that might determine the
type of recovery they would seek on a fraudulent claim. They were asked to identify all factors
that might apply, with the results shown in Table 5.
Table 5
FACTORS DETERMINING TYPE OF RECOVERY
Factors Influencing Type of Recovery Sought
on a Fraudulent Claim
Percent of Companies
Citing as Influencing Factor
Size of the claim
61.5%
Nature of the policy coverage
38.5%
Situs state for the policy
38.5%
Other (e.g., legal fees)
38.5%
Location of the claim
30.8%
Demographics of the claimant
23.1%
Policy premium payment status
7.7%
The frequency with which companies seek recovery on fraudulent claims also varies significantly.
In response to an open-ended question—“in what percent of fraudulent cases do you seek
recovery,” company responses ranged from “none to date” or “zero” or “limited” to “20% to
25%” to “75% to 80%” and a few respondents said 100%.
Just under one-third of the companies responding have prosecuted a claimant for insurance
fraud, waste or abuse. The remaining two-thirds have not done so. (See Figure 4)
0 2 4 6 8 10 12 14
Terminate the claim
Recover payments made against the policy
Give premium back and end the policy
Seek a declaratory judgment
File a declaratory action against a policyholder for
rescission or policy surrender
What are the types of relief/resolution your company pursues
after FWA confirmed?

16
Copyright © 2019 Society of Actuaries
Figure 4
RESPONDENTS’ RESULTS ON QUESTION ON REFERRAL AND PROSECUTION
Regulatory Issues
Overall, the industry does not feel that the regulatory community has a full understanding of the
nature, type and scope of FWA that is prevalent in the experience of the LTC insurance product
today. Just under 80% of respondents disagree or strongly disagree that the regulatory
community has a strong understanding of these issues, as shown in Figure 5.
0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8
Yes
No
After making a referral to a state fraud bureau, has your
company ever had a claimant prosecuted for insurance fraud,
waste or abuse?

17
Copyright © 2019 Society of Actuaries
Figure 5
RESPONDENTS’ RESULTS ON QUESTION WHETHER REGULATING COMMUNITY UNDERSTANDS FWA AND LTC
INSURANCE
Additionally, the industry believes that many referrals made by special investigative units (SIU)
are not pursued for a variety of reasons. Primary among these are budget constraints (69%) and
lack of understanding of the issues (62%). Industry also feels that states perceive the types of
misrepresentations of loss and billing that comprise fraud as “soft fraud” and for that reason are
reluctant to pursue (46%). Concern with consumer complaints or legal action (31%) or just plain
apathy on the issue (23%) may also be factors that the industry feels impede states’ willingness
to act on SIU referrals. A small percentage of respondents (15%) feel that the constraints
perceived in policy language explain why referrals are not pursued.
When asked whether any specific states are especially effective with regard to handling referrals
made by SIUs, a few respondents identified Louisiana, Florida and South Carolina based on their
individual experience there. Most others felt there was no perceived difference by state.
0.0% 5.0% 10.0% 15.0% 20.0% 25.0% 30.0% 35.0% 40.0% 45.0% 50.0%
Not sure/don't know
Strongly disagree
Disagree
Agree
Strongly agree
Do you agree or disagree that the regulatory community has a
full understanding of the nature, type and scope of fraud, waste
and abuse prevalent in the LTC insurance industry today?

18
Copyright © 2019 Society of Actuaries
LIMITATIONS
While we received a credible response rate, the sample size at 13 companies is still small in
terms of representation of the LTC industry as a whole. Specifically, the companies included in
the survey are estimated to represent approximately 40% of the 7.4 million insured lives in the
industry. As a result of a smaller sample size, we are not able to analyze findings by size or type
of company or other variables that might differentiate perspectives or practices on the topic.
The study design was specifically seeking one perspective from each company, primarily focused
on the business leader with the greatest subject matter expertise. It would have been
interesting, however, to have explored how perspectives might differ across business units
within companies. For example, claims might find great value in an approach that legal and
compliance or management is less familiar or less comfortable with.
Finally, there were a number of good questions left on the “drawing board” from the survey
design team that had to be omitted to maintain the survey to a reasonable length. Hopefully,
this report will generate discussion and additional insights to further enrich the findings
presented here.

19
Copyright © 2019 Society of Actuaries
DISCUSSION
Claimants who misrepresent impairments to satisfy the benefit eligibility trigger was identified as
the highest type of fraud, waste and abuse that insurers encounter. The industry has not
reached a universal consensus about the best tools to establish eligibility, since each tool has its
own benefits and limitations. In-person benefit eligibility assessments represent a moment in
time against which to draw a conclusion, but aren’t helpful when a claim is filed after care has
already ended. A lack of standardization raises its own challenges when reviewing provider
records to determine needed assistance. While attending physician statements and medical
records can confirm a diagnosis or yield a score from a cognitive screening test, they aren’t
always the best source of information about activities of daily living. Furthermore, distinctions
between “hands-on assistance” versus “stand-by assistance” and the frequency and intensity of
needing such assistance can be challenging to pinpoint. Claims professionals do well to consider
all “tools in the tool box”—selecting the right ones for the task at hand to make the best
eligibility decision.
Providers who are overbilling for services in excess of what was rendered came in second place.
This issue is mostly linked to home care claims originating from an insurer’s concern that it can
be difficult to tell precisely how long a caregiver is there and what they are doing while with a
claimant. The good news on this front is that electronic visit verification (EVV) has made inroads
with home care providers, since all Medicaid-reimbursed home care providers must be using
EVV as of January 1, 2019. EVV is technology used during a home health care visit—through a
mobile or landline telephone—to check in and out—and some allow the recording of services
rendered. This technology has implications to the home health care delivery system beyond just
those Medicaid-reimbursed claims. It is important to note the government moved to mandate
EVV believing it would cut down on fraud and abuse.
The survey yields a finding that all carriers are using so-called “red flags” to help detect fraud,
waste and abuse. It is also common to detect potential fraud, waste or abuse through internal
quality assurance activity, through claim system controls and by training staff to follow standard
operating procedures for so-called “high risk claims.” While these are not unexpected results, it
is somewhat concerning that only a little over 20% of companies who responded indicated they
are employing automated or predictive data analytics to identify potentially suspect claims.
While it is encouraging that close to 40% of those who responded indicated they are considering
developing this tool, perhaps a lack of resources or know-how is limiting use of this detection
method. It is also possible the limitations of legacy systems, the data captured and the quality of
the data available may not be suitable. Predictive analytics doesn’t have a long track record as a
detection tool and the survey results indicated a universal belief that it is too soon to tell if it is
producing anticipated results. This is one area to watch for future outcomes. Furthermore, it
appears those who are thinking about it or haven’t begun to explore predictive analytics can
learn from those who have.

20
Copyright © 2019 Society of Actuaries
It is widely recognized that older LTC insurance policies were written without regard to many
newer fraud controls that are often written into newer insurance contracts. For example, many
newer policies have “proof of payment” language—not just “proof of loss” requirements.
Policies from other business lines allow insurers the right to take “Examinations under Oath” of
their claimants as well as the right to require production of relevant requested documentation.
Are there any strategies or steps that the LTC Anti-Fraud community might consider taking to put
the companies in a position to be able to take advantage of some of the basic fraud controls that
are simply not expressly included in the policy language?
Approximately 75% of responding carriers stated that they believed that the regulatory
community does not fully understand the nature, type and scope of fraud, waste and abuse
prevalent in the LTC industry, while less than 10% indicated that they believed the regulatory
community had such understanding. Assuming the carriers’ perspective has merit, what has led
to such a disconnect between the regulatory community and the carriers? More important, what
can we do as an industry to help educate the community on important LTC fraud issues and/or
close the knowledge gap?
The survey respondents provided many potential reasons why they believe state fraud bureaus
are pursuing long-term care fraud referrals at a lower frequency than deserved. Is there anything
that the industry can do to stimulate interest from the state fraud bureaus in opening more
fraud investigations into long-term care claims? Should carriers care if fraud bureaus are
pursuing LTC referrals, i.e., are carriers overstating the importance of the possibility of criminal
actions if the carriers are independently making their own claim decisions? What can carriers do
in strong cases when the state fraud bureau chooses not to pursue an investigation?
Last, the carriers were asked, “How effective do you think our industry is in addressing fraud,
waste and abuse?” No carrier indicated that the industry is extremely effective or very effective.
Rather, 55% responded that the industry was “somewhat effective,” while 40% indicated the
industry was either “not so effective” or “not effective at all.” If it is assumed that the industry
perspective is accurate, what are the primary reasons why the industry is so ineffective? Is the
industry trending toward improving its effectiveness in combating fraud? If so, what
improvements are carriers making to increase fraud, waste and abuse mitigation effectiveness?

21
Copyright © 2019 Society of Actuaries
APPENDIX: FULL SURVEY

The Society of Actuaries (SOA) Long Term Care Insurance Section is sponsoring this survey to
better understand the concerns companies have with their efforts to address fraud, waste and
abuse in LTC insurance. Specifically, we want help identifying ways that industry can improve its
relationship with regulators in support of best practices for fraud prevention, detection and
recovery. Please take a few minutes to share your opinions with us. ALL RESPONSES ARE
ANONYMOUS AND NO COMPANY RESPONSES WILL BE INDIVIDUALLY IDENTIFIED.
The person at your company who is likely best suited to complete this survey would be the LTC
business leader. We have attached a PDF version of the survey so that you may review it first to
determine who at your company should complete the survey. We encourage that individual to
obtain input from all relevant areas within the company working on these issues.
First - some basic definitions:
FRAUD - intentional misuse of information in order to persuade another to part with something of
value or to surrender a legal right. It could also be an act of planned deception or
misrepresentation;
WASTE - To use, consume, spend or expend thoughtlessly or carelessly;
ABUSE - Providing information or documentation for a health care claim in a manner that
improperly uses program resources for personal gain or benefit, yet without sufficient evidence to
prove criminal intent.
Introduction
1. First, please tell us in which business area of the company you are engaged (e.g., claims, legal,
actuarial, corporate, etc.?
*
2. And how long has your company been in the LTC business?*
3. Approximately how many policies does your company have inforce?*
Less than 50,000
50,000 to 99,999
100,000 to 249,999
250,000 to 399,999
400,000 or more

Not at all Significant Very Significant
Claimant
misrepresentation of
loss
Provider
misrepresentation of
loss
Claimant
misrepresentation of
services and/or billing
Provider
misrepresentation of
services and/or billing
Collusion between
claimants and providers
with regard to
misrepresentation of
loss
Collusion between
claimants and providers
with regard to
misrepresentation of
services and/or billing
4. Please indicate how significant each of the following is as a source of the fraud, waste and abuse your
company experiences.
*
5. Please rank each of the types of fraud, waste and abuse that your company experiences in the order
of significance to your company (in terms of either cost and/or prevalence) , with "1" being most significant
and "5" being least significant.
*
Claimants who misrepresent impairments in an attempt to satisfy benefit eligible
Claimants who misrepresent continuation of disability (deny recovery) in order to continue to receive benefits
Providers billing for services not rendered
Providers overbilling for service amounts in excess of what was rendered
Billing for providers who are not eligible under the contract

Already using Would consider Might consider Would not consider
Not familiar enough
to know
Examinations under
oath
Recorded interviews
Requiring proof of
payment for expenses
incurred
Pursuing a declaratory
judgment
Gathering forensic data
on mobile devices
Using field claims
consultant to interview
claimant in person and
complete a claim form
(not an assessment)
A database similar
to MIB (Medical
Information Bureau)
where carriers report
suspected fraudulent
claimants and/or
providers
Use of Electronic Visit
Verifications tools
6. Some practices in combating fraud, waste and abuse that are used in other insurance business lines are
shown below. We want to know if you think these might have some applicability to LTC insurance. Please
tell us whether you have or would consider any of these. As you consider them, please assume that
whatever regulatory changes needed to enable or allow you to use them could be obtained.
*
7. Which one of the following types of claim locations do you feel generates the largest portion of potential
fraud, waste and abuse referrals/investigations?
*
Nursing home
Assisted living facility
Formal home care claims
Informal home care claims (e.g., independent provider or
family member)
Other (please specify)

8. Which type of claim diagnosis do you feel generates the highest portion of potential fraud, waste and
abuse referrals/investigations?
*
Functional impairment
Cognitive impairment
Medical necessity
Other (please specify)
9. Are there other specific situations that you feel might escalate the potential for fraud, waste and abuse?
(Please check all that apply)
*
Assignment of Benefit
Rate increase
Power of attorney
None of the above
Other (please specify)
10. What do you feel is the most important control your company or TPA has in place to help prevent fraud,
waste and abuse?
*
11. How is fraud, waste and abuse detected at your company or TPA? (Please check all that apply)?*
Whistleblower program
Fraud warnings on letters
Fraud warnings on claim documents
Fraud warnings as part of policy fulfillment
Fraud hotline
Claim Systems Controls
Automated or Predictive Data Analytics
Internal quality assurance
Secondary review by senior claim staff, management, law
Standard operating procedures that provide guidance for
handling different types of "high risk" claims
Red flags that staff are trained to look for
None of the above
Other (please specify)

12. How are staff trained to spot potentially fraudulent activity? (Please check all that apply)*
Red flag lists
Case illustrations
Formal training program
On the job training
None of the above
Other (please specify)
13. Please tell us about anything new or creative that you have implemented to detect fraudulent activity
that hasn't yet been mentioned in this survey.
14. Which of the following techniques or tools do you use for detecting and/or investigating potential fraud,
waste and abuse? (Check all that apply)
*
Surveillance
Background checks
Social media checks
Unannounced visit
Other (please specify)
15. Do you use automated/predictive analytics to help more cost effectively identify which claims to pursue
for likely fraud, waste or abuse?
*
Yes
Not yet but we are considering it
No
16. If you are using automated predictive analytics, how satisfied are you with the results?*
Very satisfied
Somewhat Satisfied
Not very Satisfied
Not at all satisfied
Too soon to tell
Not relevant - we are not using predictive analytics
17. What is the most important aspect of working with investigative firms on pursuing fraud, waste and
abuse issues?
*

18. If you have a dedicated fraud hotline, or if you encourage use of your customer service line for that
purpose, how effective do you feel it has been in generating useful referrals?
*
Very effective
Somewhat effective
Not so effective
Not at all effective
Other (please specify)
19. What are the types of relief/resolution your company pursues after fraud, waste or abuse is confirmed?
(Please check all that apply)
*
Terminate the claim
Recover payments made against the policy
Give premium back and end the policy
Seek a declaratory judgment
File a declaratory action against a policyholder for rescission
or policy surrender if fraud, waste or abuse is discovered
Other (please specify)
20. Which of these do you use most often? (Please choose only one)*
Terminate the claim
Recover payments made against the policy
Give premium back and end the policy
Seek a declaratory judgment
File a declaratory action against a policyholder for rescission
or policy surrender if fraud, waste or abuse is discovered.
Other (please specify)
21. Other than the strength of the case, what factors determine whether you seek some type of recovery
on fraudulent claims? (Please check all that apply)
*
The size of the claim
Location of the claim
Demographics of the claimant
Nature of the policy coverage
Situs state for the policy
Policy premium payment status
Other (please specify)
22. In what percent of fraudulent claim cases do you seek recovery?*

23. Do you agree or disagree that the regulatory community has a full understanding of the nature, type
and scope of fraud, waste and abuse prevalent in the LTC insurance industry today?
*
Strongly agree
Agree
Disagree
Strongly disagree
Not sure/don't know
24. The industry believes that many referrals made by Special Investigative Units (SIU) to State Fraud
Bureaus are not pursued. Why do you think this is? (Please check all that apply)
*
Budget constraints
Lack of understanding
Apathy
State sees it as "soft fraud"
Feeling of "goodwill" toward elderly - see them as "vulnerable"
population
Not want to "stir the pot"
Concerned with getting complaints or legal action
Constraints perceived in policy language
Other (please specify)
25. Is there any states that you feel are especially effective with regard to handling referrals made by
SIUs? And if so, why do you think that is the case?
26. Overall, how effective do you think our industry is in addressing fraud, waste and abuse?*
Extremely effective
Very effective
Somewhat effective
Not so effective
Not at all effective
Don't know/not sure
27. What do you think is the primary challenge our industry faces in not being more effective in addressing
these issues? (Please choose one)
*
Companies don't understand the problem well enough
Lack of compliance/regulatory support for taking action
Lack of resources to address these issues
Company doesn't prioritize these issues
Company concern with negative PR gets in the way
Still building knowledge, training and technology
I don't see a problem. I'm satisfied with how effectively
industry is dealing with this
Other (please specify)

28. After making a referral to a state fraud bureau, has your company ever had a claimant prosecuted for
insurance fraud, waste or abuse?
*
Yes No
29. What do you think groups like SOA, ILTCI, the LTC Forum, AHIP, ACLI and others should be doing to
address fraud, waste and abuse?
*
30. And finally, one last question. Are you aware that there is an industry group - the Anti-Fraud Forum -
that meets twice a year to share best practices regarding how to handle potentially fraudulent claims?
*
Yes No
31. If you would like more information about the Anti-Fraud Forum, send an email to Jeffrey Ferrand at
jferrand@fuzionanalytics.com
32. Thank you so very much for your participation in this survey. We will be sharing a summary of results
as soon as they are available. If you have any additional comments or concerns, please feel free to share
them with us in the space below.

22
Copyright © 2019 Society of Actuaries
About The Society of Actuaries
The Society of Actuaries (SOA), formed in 1949, is one of the largest actuarial professional organizations in the world
dedicated to serving 32,000 actuarial members and the public in the United States, Canada and worldwide. In line
with the SOA Vision Statement, actuaries act as business leaders who develop and use mathematical models to
measure and manage risk in support of financial security for individuals, organizations and the public.
The SOA supports actuaries and advances knowledge through research and education. As part of its work, the SOA
seeks to inform public policy development and public understanding through research. The SOA aspires to be a
trusted source of objective, data-driven research and analysis with an actuarial perspective for its members,
industry, policymakers and the public. This distinct perspective comes from the SOA as an association of actuaries,
who have a rigorous formal education and direct experience as practitioners as they perform applied research. The
SOA also welcomes the opportunity to partner with other organizations in our work where appropriate.
The SOA has a history of working with public policymakers and regulators in developing historical experience studies
and projection techniques as well as individual reports on health care, retirement and other topics. The SOA’s
research is intended to aid the work of policymakers and regulators and follow certain core principles:
Objectivity:
The SOA’s research informs and provides analysis that can be relied upon by other individuals or
organizations involved in public policy discussions. The SOA does not take advocacy positions or lobby specific policy
proposals.
Quality:
The SOA aspires to the highest ethical and quality standards in all of its research and analysis. Our research
process is overseen by experienced actuaries and nonactuaries from a range of industry sectors and organizations. A
rigorous peer-review process ensures the quality and integrity of our work.
Relevance:
The SOA provides timely research on public policy issues. Our research advances actuarial knowledge
while providing critical insights on key policy issues, and thereby provides value to stakeholders and decision
makers.
Quantification:
The SOA leverages the diverse skill sets of actuaries to provide research and findings that are driven
by the best available data and methods. Actuaries use detailed modeling to analyze financial risk and provide
distinct insight and quantification. Further, actuarial standards require transparency and the disclosure of the
assumptions and analytic approach underlying the work.
Society of Actuaries
475 N. Martingale Road, Suite 600
Schaumburg, Illinois 60173
www.SOA.org
