
EDUCATION STANDARDS:
Curriculum Guidelines and
Education Competencies for
Neonatal Nurse Practitioner Programs
2023
National Association of Neonatal Nurse Practitioners
2
Committee for the 2023 Revision of Education Standards: Curriculum
Guidelines and Education Competencies for Neonatal Nurse
Practitioner Programs
Michele K. Savin, DNP APRN NNP-BC CNE, Chair
Tracey R. Bell, DNP APRN NNP-BC
Media Esser, PhD NNP-BC APNP CWCN
Desi M. Newberry, DNP NNP-BC CHSE
Amy Koehn, PhD NNP-BC
Jenna Staggs, DNP APRN NNP-BC RNC-NIC C-ONQS C-ELBW
Jan Wilson, DNP CRNP NNP-BC C-ELBW FAANP
Acknowledgments
The committee thanks the many people who provided guidance, input, and feedback
during development of this publication. In alphabetical order, they include:
Bobby Bellflower, DNSc NNP-BC FAANP, NANNP Council liaison and reviewer
Dedra Teel, MSN RN NNP-BC, NANNP Council liaison and reviewer
Suzanne L. Staebler, DNP APRN NNP-BC FAANP FAAN, content reviewer
Sandy Bellini, DNP APRN NNP-BC CNE, content reviewer
Carol Kenner, PhD RN FAAN, content reviewer
Carol Wallman, DNP APRN NNP-BC, NCC President and content reviewer
Mary Beth Bigley, DrPH ANP-BC FAAN, NONPF CEO and content reviewer
Barbara Snapp, DNP APRN NNP-BC, NANNP Council Chair
NANNP Faculty Special Interest Group (SIG) members, content reviewers
Leanne M. Nantais-Smith, PhD RN NNP-BC FAANP, NANNP Council reviewer
The committee also thanks the American Nurses Credentialing Center (ANCC) and
National Organization of Nurse Practitioner Faculties (NONPF) for providing permission
for NANNP to include portions of their educational domains, competencies, and
subcompetencies in this publication.
Adopted by the National Association of Neonatal Nurse Practitioners (NANNP) Council
in April 2023. Title amended in August 2023. No part of this publication may be
reproduced without the written consent of the National Association of Neonatal Nurse
Practitioners (NANNP).
Note: Titles of previous editions of this document include Education Standards for
Neonatal Nurse Practitioner Programs (2003), Education Standards
and Curriculum Guidelines for Neonatal Nurse Practitioner Programs (2009, 2017), and
Curriculum Guidelines and Education Competencies for Neonatal Nurse Practitioner
Programs (April 2023-August 2023).
Copyright © 2023 National Association of Neonatal Nurse Practitioners
Published by the National Association of Neonatal Nurses
8735 W. Higgins Road, Suite 300, Chicago, IL 60631
847.375.3660
www.nann.org
3
CONTENTS
Introduction ................................................................................................................... 4
Curriculum Guidelines ................................................................................................ 10
Chapter I: Mission and Governance ................................................................... 10
Chapter II: Resources ......................................................................................... 12
Chapter III: Curriculum ....................................................................................... 14
Chapter IV: Evaluation ........................................................................................ 16
Education Competencies ........................................................................................... 20
Appendices .................................................................................................................. 48
Appendix A. 2023 NNP Competencies List ........................................................ 48
Appendix B. Suggested Responsibilities and Activities ...................................... 51
Appendix C. 2021 AACN Domains ..................................................................... 53
Appendix D. 2021 AACN Concepts .................................................................... 55

4
INTRODUCTION
Neonatal nurse practitioners (NNPs) provide holistic, family-centered, child-focused
care in the preventative, restorative, chronic, and palliative spheres for patients from
birth at any gestation to age 2.
As healthcare providers, NNPs perform advanced health assessment, diagnostic
reasoning, and critical decision-making and have clinical competence for the diagnosis,
management, and treatment of primary care as well as acute, chronic, and complex
health problems. Collaborating on an interprofessional team, the NNP participates in a
wide variety of complex patient-care activities in settings that include, but are not limited
to, all levels of neonatal inpatient care in both academic- and community-based
settings, transport, and delivery room. NNPs provide health care in acute, primary,
chronic, and outpatient settings. NNPs practice autonomously and in coordination with
other healthcare professionals, providing a unique emphasis on the convalescence,
health and well-being of the child and family through a focus on health promotion,
disease prevention, and health education.
NNPs are thus prepared across all aspects/spheres of the nurse practitioner (NP) role:
clinical care; conducting and reviewing evidence-based projects and implementing
research; education; consultation, and advocacy to optimize the care of newborns,
infants, and toddlers. NNPs occupy a unique space on the inter-professional team.
Their neonatal role–specific knowledge is validated through national certification.
There continues to be a shortage of NNPs. Given the neonatal population–specific
educational components needed to produce a competent, novice-level NNP, filling the
gaps with providers who have a generalist education—such as physician assistants,
pediatricians, or nurse practitioners educated in other population foci—is not in the best
interest of providing high-quality, safe, and cost-effective neonatal care.
Defining NNP Competencies
The National Association of Neonatal Nurses (NANN) and the National Association of
Neonatal Nurse Practitioners (NANNP) believe it is imperative that neonatal content
experts define NNP competencies and the systems of education and training required to
obtain them. NANN and NANNP collaborate with a number of regulatory, licensing,
education, and credentialing agencies to produce the most current education and
curriculum standards.
The competencies align with and reflect:
• American Association of Colleges of Nursing (AACN) The Essentials: Core
Competencies for Professional Nursing Education (2021)
• National Organization of Nurse Practitioner Faculties (NONPF) Nurse
Practitioner Role Core Competencies (2022)
• National Task Force on Quality Nurse Practitioner Education (NTF) 2022
Standards for Quality Nurse Practitioner Education (6th edition).
5
The Essentials: Core Competencies for Professional Nursing Education defines 10
domains that are the “essence of professional nursing practice,” along with eight
concepts and four spheres of care (AACN, 2021, p. 1). Each domain has competencies
for advanced nursing practice and subcompetencies that define advanced nursing
practice.
Developed by expert educators and practitioners, with stakeholder input, AACN’s 2021
The Essentials: Core Competencies for Professional Nursing Education and NTF’s
2022 Standards for Quality Nurse Practitioner Education (6th edition) represent best
practices for NP program development, support, education, and evaluation. Those
seminal documents’ forward-thinking changes in approaches to nursing and nurse
practitioner education prompted this 2023 update of Education Standards: Curriculum
Guidelines and Education Competencies for Neonatal Nurse Practitioner Programs.
Items specific to NNP education and practice are reflected here. In previous iterations,
there were six program standards. This new document is organized in the same four
sections as the NTF Standards: mission and governance, resources, curriculum, and
evaluation. However, all items required in the 2021 Essentials: Core Competencies for
Professional Nursing Education and 2022 Standards for Quality Nurse Practitioner
Education (6th edition) apply to NNP programs, whether expounded upon here or not.
NONPF has further identified nurse practitioner (NP) core competencies in Nurse
Practitioner Role Core Competencies (2022). This publication from NANNP contributes
the specialty competencies necessary for safe and competent NNP practice.
It should be noted that The Essentials: Core Competencies for Professional Nursing
Education no longer organizes the essentials by educational degree but by entry to
practice and advanced-level competencies. These advanced-level competencies
presented by AACN apply to any nurse obtaining further education beyond the entry-to-
practice–level competencies. NONPF’s Nurse Practitioner Role Core Competencies are
written for a student to be evaluated at a clinical doctoral level (NONPF, 2022). At this
time, NANNP supports NNP education at the master’s or doctoral level. Students may
continue to choose the master’s or doctoral education as the end point of a program of
study, and universities will make individual determinations as to the degrees offered.
Key Callouts
AACN’s The Essentials: Core Competencies for Professional Nursing Education (2021),
NONPF’s Nurse Practitioner Role Core Competencies (2022), and NTF’s 2022
Standards for Quality Nurse Practitioner Education (6th edition) have some key areas of
emphasis:
The necessity of input from the community of interest to ensure a quality NP
program
All NP programs should actively seek thoughtful input from community stakeholders in
the development and outcome of NP education. For the NNP specialty, these
stakeholders include (but are not limited to) students, children and families,
communities, and employers of NNPs.
6
Though some students master skills and demonstrate competence more rapidly than
others, a minimum number of practicum hours are still required at this time to promote
consistency in NNP education that is evident to stakeholders (AACN, 2021, see pages
18 and 22). Program learning outcomes should reflect attainment of all competencies.
Through the demonstration of the competencies documented in AACN’s Essentials:
Core Competencies for Professional Nursing Education nursing, NONPF’s Nurse
Practitioner Role Core Competencies, and the NANNP NNP specialty competencies,
stakeholders—including employers—will have a clear understanding of NNP education
and how it provides the critical knowledge and skills that prepare the NNP to practice as
a unique member of the healthcare team (AACN, 2021).
Competency-based education
Competency-based education focuses on what a student learns and can demonstrate,
rather than what the educational program teaches. Faculty, therefore, need to offer
active didactic and clinical experiences which are scaffolded, are interprofessional, and
offer the repetition and time to build student confidence and expertise in advanced-level
nursing skills (AACN, 2021, see page 23).
Student competence should be transferable across defined neonatal care settings and
is integral to the achievement of a professional identity as an NNP. Domains, concepts,
and spheres of care should be woven throughout the curriculum. Individual course-
based outcomes should build on one another and be linked to the competencies.
Complexity should build over time, and assessments and performance should both
teach and evaluate (AACN, 2021, see page 18).
Increasing requirement to 750 direct patient-care hours (from 500)
NTF’s 2022 Standards for Quality Nurse Practitioner Education (6th edition) requires
750 direct-care clinical hours, not inclusive of simulation hours. NANNP assures
stakeholders that we put great thought and consideration into the 750-hour direct-care
requirement. This increase is an opportunity to strengthen current curriculum to create
competent NNPs across the continuum of our scope of practice. Programs, especially at
the doctoral level, may choose to require more than 750 hours. As competency-based
education becomes more established, specific numbers of hours in programs will
become less integral to student evaluations.
Faculty and preceptor requirements
The NTF document makes clear that neonatal program directors and educators are
required to have ongoing experience and current knowledge and must directly
participate in and make decisions regarding NNP programs (NTF, 2022, see page 10).
Universities should support faculty in clinical practice and ensure NNP programs have
direct oversight by a doctoral-prepared NNP (NTF, 2022, see Criterion 1.F on page 8).
Faculty must have appropriate academic and specialty credentials to support the
planning and evaluation of student work which demonstrates “longitudinal attainment of
7
advanced level subcompetencies,” enabling the student to make the connection
between scholarly activity and full NP scope of practice (AACN, 2021, p. 25).
NNP programs educate nurses to be competent in a neonatal advanced practice
nursing role and in the advanced-level competencies. As part of the interprofessional
team caring for sick, convalescing, and well children, NNP students are exposed to a
rich learning environment, including mentors with diverse education and ideas. Students
work with and learn from all members of the interprofessional team.
Ideally, NNPs precept NNPs. However, this proves challenging in some circumstances.
According to the NTF (2022, see Criterion II.C on page 11), the documentation
programs must collect for supervisors of NPs includes:
Documentation of clinical preceptors’ preparation and current expertise to
support each student’s development of NP professional role and student
achievement of expected program clinical outcomes…relevant
biography/curriculum vitae of clinical preceptors that address current
qualifications…documentation of degree(s), unencumbered license or other state
authorization to practice in the state or territory in which they practice, and
national certification of preceptor. (p. 11)
As such, master’s- or doctoral-prepared neonatal-certified NNPs or perinatal-neonatal
board-certified physicians are qualified preceptors in the neonatal intensive care unit
(NICU). In other clinical areas, documentation of area of expertise and national board
certification in that specialty area, along with license, should also be obtained.
Clarification of faculty roles and responsibilities for clinical site placement and
student clinical experiences
Clinical sites need to be congruent with program/course goals. Programs are
responsible for ensuring students have access to sufficient clinical sites (AACN, 2021,
see page 20). There are many interprofessional learners in the neonatal space, creating
demand for real-world experiences for certain educational goals; the preceptor should
advocate for the student to perform procedures and other patient care activities
happening to their patients. It is incumbent upon programs to create simulation
opportunities to demonstrate procedural competencies and meet educational standards
for the role, using national simulation best practice standards (International Nursing
Association for Clinical Simulation and Learning Standards Committee, 2021).
Documentation of diversity, equity, and inclusion policies and procedures
The Essentials: Core Competencies for Professional Nursing Education emphasizes
diversity, equity, and inclusion. NNPs take pride in our role as holistic providers of care
to infants, toddlers, and their families. Introspection and work are necessary to ensure
equity in education and provision of care. This document from NANNP supports
academic freedom, while expecting all educational programs to meet the stated
guidelines.
8
Determination that NP students have achieved entry-level advanced practice
nursing patient-care competence before students start direct patient-care clinical
hours
NANNP recognizes that many educational standards and guidelines rely on expert
opinion and usual practice in areas where there is a lack of clear evidence. The goal is
to adhere to best practice when it exists. Where evidence is conflicting or lacking, this
document reflects a conscious decision to adhere to current practice without lowering
the standard.
One area robustly discussed by faculty is the requirement of acute-care practice in the
neonatal/pediatric areas prior to program admission. Given the challenges of preparing
NNPs and new requirements to document baseline advanced practice before entering
clinical courses, prior experience in and a minimal baseline knowledge of neonatal care
are necessary. Benner’s novice to expert model demonstrates competence as the third
stage in the development and acquisition of skill, occurring at 2–3 years of practice
(Benner, 1982).
Therefore, lacking other evidence, this document retains the recommendation of a
minimum of 2 years of relevant NICU experience for students before entry into clinical
courses. The committee believes learners have the best opportunity to succeed if they
have prior Level III and Level IV NICU experience. Programs should evaluate
candidates holistically on a case-by-case basis and may in certain cases be able to
document practice experience in other areas to narrow the 2-year window.
There are areas of suggested best practice in this document that strongly encourage
programs to utilize methods to optimize success, such as use of clinical logs to
document competency achievement. This document does not have requirements for
numbers of procedures or activities, rather each program will need to offer stakeholders
and certifying bodies documentation of the ways learners have met programmatic
outcomes.
Focus on evidence-based practices and self-care as part of NP professional
identity and responsibility.
The professional identity of an NNP is more than the sum of their clinical knowledge.
The advanced role requires self-awareness as well as the ability to participate in quality
improvement while educating and advocating for patients, their families, and the
profession. NNPs work to improve health care via broad utilization and dissemination of
quality improvement, implementation science, and research to strengthen evidence-
based care (NONPF, 2022, see Competency 4.2).
The Essentials: Core Competencies for Professional Nursing Education’s new Domain
10: Personal, Professional and Leadership Development (AACN, 2021, see page 53)
presents a shift in the understanding of nursing professionalism. NNP practice is
supported by personal attributes of self-care, reflection, and lifelong learning which

9
promote role transition and leadership potential. Individuals have a personal
responsibility to both self and patient. NANN and NANNP support NNPs through
position statements such as “The Impact of Advanced Practice Registered Nurses’ Shift
Length and Fatigue on Patient Safety” and “State of Neonatal APRN Role and Action for
the Future,” the Neonatal Nurse Practitioner Workforce Survey, and other efforts
(NANN, n.d.).
How to Use this Document
This 2023 publication of Education Standards: Curriculum Guidelines and Education
Competencies for Neonatal Nurse Practitioner Programs is aligned and intended to be
used in conjunction with the following three publications:
• The new model for education published by AACN in The Essentials: Core
Competencies for Professional Nursing Education (2021)
• NP-specific core competencies described by NONPF in Nurse Practitioner Role
Core Competencies
• Evaluation criteria outlined by NTF in Standards for Quality Nurse Practitioner
Education, 6th Edition
This document describes the minimum standards necessary to ensure NNP program
graduates receive preparation to practice and provide high-quality, safe, and cost-
effective neonatal care. It serves as a tool for the development and evaluation of new
NNP programs and a self-study manual for existing programs. Programs will find
neonatal-specific support here, but should refer to the AACN, NONPF, and NTF
documents listed above for a complete understanding of educational expectations for
the nurse practitioner role.
Students educated using this new model will demonstrate competence in all aspects of
the NNP role, rooted in self-reflection and professionalism, which supports lifelong
learning.
10
CHAPTER I: MISSION AND GOVERNANCE
As providers of health care to a specific population, NNPs’ practice "spans the
healthcare delivery continuum from public health prevention to disease management of
[neonates] and describes collaborative activities with both traditional and non-traditional
partnerships from affected communities, public health, industry, academia, health care,
local government entities, and others for the improvement of equitable population health
outcomes" (AACN, 2021, p. 10).
NNPs provide primary, acute, chronic, and critical care to the population of preterm
neonates, neonates, infants, and toddlers up to 2 years of age (NANN, 2017; NONPF,
2013).
"The [neonatal] NP program is aligned with the institution’s mission/philosophy/values
and governance that support educational excellence through a structure that addresses
quality assurance and improvement; diversity, equity, and inclusion (DEI); and input
from the community of interest" (NTF, 2022, p. 7, see Criteria I.A, I.B., and I.C. on page
7 and Criterion I.F on page 8).
"The governance structure within the institution facilitates ongoing quality improvement
through participation in the development, implementation, maintenance, and evaluation
of the NP program by a community of interest, including administrators, faculty,
students, and practice partners" (NTF, 2022, p. 7, see Criterion I.B. on page 7).
The “community of interest” for NNP programs includes neonates, infants, and toddlers
up to age 2 in primary, acute, chronic, and outpatient settings and their families;
academic partners; preceptors; professional and community organizations, including
healthcare organizations; and employers who support neonatal care.
For the neonatal population focused track, each program must employ a neonatal
“faculty member who holds an institutional appointment to provide direct oversight of the
track. This individual is doctorally prepared, currently licensed, or authorized to practice,
and nationally board certified as [an NNP]…” (NTF, 2022, p. 8, see Criterion I.F on page
8).
Program Requirements
Prior to the start of a new NNP program, assessments should be completed of
workforce needs and enrollment capacity (NTF, 2022, see Criterion I.I on page 9).
The NNP program should be awarded preapproval, pre-accreditation candidacy, or
accreditation status prior to the admission of students.
Programs must have an adequate number of neonatal faculty to meet the needs of the
students and the program (NTF, 2022; see Criterion II.C on page 10). Program
leadership should be directed by and oversight provided by doctoral-prepared NNPs
(NTF, 2022; see Criterion I.F on page 8).
Active or recent (within the past 2 years) clinical practice in the neonatal scope and

11
national neonatal nurse practitioner certification are required for those teaching NNP
clinical courses, and academic practice partnerships are encouraged. Institutional
policies should support faculty scholarship and clinical practice in order to maintain
clinical expertise (NTF, 2022, see Criterion II.C. on page 9).
Non-NNP faculty members must have and maintain expertise in the area in which they
are teaching (NTF, 2022, see Criterion II.C. on page 10).
The NNP program should prepare the graduate for population-focused practice in the
NNP role, to practice across the continuum, providing primary, acute, chronic, and
critical care to neonates, infants, and toddlers to age 2.
It is the responsibility of the faculty to maintain National Certification Corporation (NCC)
compliance. Graduates must remain eligible for NCC Neonatal Nurse Practitioner
examinations or other national neonatal certification options as applicable. See NCC’s
Nurse Practitioner Program Profile for more information.
A minimum of 750 direct patient-care hours and documentation of mastery of novice
NNP competencies are required for student completion of the program (NTF, 2022; see
NTF Criterion III.H on page 14).
Level III and Level IV NICUs and sites with delivery room learning opportunities are
appropriate for meeting a minimum of 600 hours of the 750-hour requirement. Other
clinical sites may be utilized as needed to meet necessary competencies and remaining
clinical hours.
Oversight of student clinical experiences should be conducted by board-certified
advanced practice registered nurses (APRNs) or by board-eligible or board-certified
physician preceptors. NANNP recognizes that other members of the interprofessional
team will be active educational partners (NANN, 2017; NTF, 2022; see NTF Criterion
II.D on page 11). Programs are responsible for maintaining documentation that faculty
adjuncts and preceptors meet the requirements for education and national specialty
certification.
12
CHAPTER II: RESOURCES
Faculty
NNP program faculty should comprise individuals with expertise and emphasis in
research, teaching, and clinical practice. Though it may be difficult for some faculty
members to balance research, practice, and teaching responsibilities, all faculty
members who teach clinical courses must maintain national certification as NNPs and
have active or recent clinical experience. Maintaining this currency is important to
ensuring clinical competence in the area of teaching responsibility. A faculty-to-student
clinical supervision ratios of 1:6 is preferred.
Preceptors
Preceptors mentoring students in Level III and Level IV NICUs must have a graduate
degree in nursing (ie, MS, MSN, or higher) and be nationally certified as NNPs or be
physicians who are board-certified in neonatology or board-certification eligible (NTF,
2022; see Criterion II.C on page 11).
In settings outside of the NICU, preceptors must have a graduate degree in nursing (ie,
MS, MSN, or higher) and be nationally certified as an NP (eg, PNP, ACPNP).
Preceptors also may be board-certified physicians. (NTF, 2022, see Criterion II.C on
page 11).
Preceptors should have a minimum of 1 year full-time equivalent experience in the
NP/MD role and be fully oriented to the role at the clinical site. A qualified preceptor
should have no limitations on the performance of their job, such as probationary status
(NTF, 2022; see Criterion II.C on page 11).
Each preceptor will decide how many students they are comfortable managing each
shift, taking into consideration precepting and other patient-care responsibilities.
Consider a 1:1 preceptor/student ratio if preceptors have their own patient load and 1:2
ratio if they do not have their own patient load (Loewen et al., 2017, NANN, 2017; NTF,
2016, see Criterion IV.B.1 on page 14).
Preceptors must be oriented to NNP program requirements and to the expectations for
supervision and evaluation of the NNP students (NTF, 2022; see Criteria II.C and II.G
on page 12).
Preceptor responsibilities include (NTF, 2022; see Criteria II.C and II.G on page 12):
• Discuss learning objectives, institutional guidelines and protocols, and scheduling
prior to starting clinical hours.
• Ensure ongoing student and faculty feedback regarding student progression and
any recommended remediation
• Provide feedback throughout the semester and in written form at the end of the
semester
See Suggested Student Learning Activities in Appendix B.
13
Clinical Sites
Each NNP program will identify specific student responsibilities for each clinical site
(NTF, 2022; see Criterion II.C on pages 10–11). See Appendix B for suggested student
responsibilities.
Clinical sites should:
• Provide the student with ample opportunities to meet learning objectives,
demonstrate competencies, and have educational experiences outlined by their
program (NTF, 2022; see Criterion II.G on page 12).
• Ensure that direct onsite supervision and consultation are available from the
preceptor (NTF, 2022; see Criterion II.G on page 12).
• Be congruent with the expected student learning objectives and competencies as
outlined per program course or semester goals (NTF, 2022; see Criteria II.F and
II.G on page 12).
• Provide the student with support to practice to the full scope of practice under the
supervision on the fully licensed neonatal professional (NTF, 2022, see Criterion
II.C on pages10–11).
14
CHAPTER III: CURRICULUM
Before a student begins NNP clinical courses, they must have the equivalent of 2 years
of clinical practice experience (within the past 5 years) in the care of critically ill
neonates or infants in critical care inpatient settings. Students may enroll in preclinical
courses while obtaining the necessary practice experience.
The MSN to DNP and BSN to DNP degree are both recognized as appropriate for entry
into practice as an NNP.
It is strongly encouraged that DNP candidates have a neonatal content expert involved
in the planning, implementation, and dissemination of their project. This increases
involvement of community of interest (AACN, 2006; NTF, 2022; see Criteria III.C and
IV.D on page 13).
Under the direction of the NNP faculty, the curriculum must contain content and clinical
experiences to meet the core NP competencies and neonatal population-specific
competencies for NNP practice shown in the Competencies section in this document.
Individuals providing didactic instruction should come from the interprofessional team of
healthcare providers who have expertise in their respective areas. Participants will be
determined according to the resources available to the program but generally should
include NNPs, neonatologists, pediatric subspecialists, APRNs, and allied health
specialists.
The NNP program must prepare students at the advanced practice level prior to
beginning direct patient-care hours (NTF, 2022; see Criterion II.G on page 14).
Core Courses
The curriculum must include, at a minimum, three separate graduate-level core courses,
which precede NNP population-specific coursework, in the following areas:
• advanced physiology and pathophysiology, including general principles that
apply across the lifespan
• advanced health assessment, including advanced assessment techniques,
concepts, and approaches
• advanced pharmacology, including pharmacodynamics, pharmacokinetics, and
pharmacotherapeutics of all broad categories of agents.
Specific neonatal content and/or courses related to advanced physiology and
pathophysiology, advanced health assessment, and advanced pharmacology must be
included and integrated throughout the other neonatal-specific didactic and clinical
courses (NTF, 2022; see Criterion III.I on page 14)
Didactic, Clinical, and Simulation Content
Didactic and clinical content related to primary care of high-risk infants during the first 2
15
years of life must be included in the curriculum. It is strongly encouraged that the NNP
curriculum and clinical component include interprofessional educational experiences
(NTF, 2022; see Criterion III.F on page 14).
The clinical component of the NNP curriculum must include a minimum of 750 direct
patient-care hours.
• Settings can include delivery rooms; newborn nurseries; Level II, III, and IV
NICUs; and pediatric ICUs (PICUs). Clinical care in settings that encompass
primary care for the patient to 2 years of age (ie, pediatric offices, developmental
clinics, follow-up clinics) can be included in the 750 hours.
• At minimum, 600 direct patient-care hours must be spent with critically ill
newborns and/or infants in Level III and/or Level IV NICUs. Precepted clinical
hours caring for infants with cardiac disease or postsurgically in the PICU or
Cardiac Intensive Care Unit (CICU) also may count toward the minimum 600
clinical hours.
• Direct patient-care hours may include telehealth and global health experiences
involving infants, neonates, and toddlers up to 2 years of age. (NTF, 2022; see
Criteria III.H and III.J on pages 14–15).
The NNP program must contain evidence of the use of simulation, following best
practice and national standards (International Nursing Association for Clinical
Simulation and Learning Standards Committee, 2021), to support student learning,
competency development, and evaluation.
Observational or simulation hours do not count toward the 750 direct patient-care hour
minimum (NTF, 2022; see Criteria III.H and III.J on pages 14–15).
Postgraduate students must successfully complete graduate didactic and clinical
requirements of an academic graduate NNP program through a formal graduate-level
certificate or degree-granting graduate level NNP program (NTF, 2022; see NTF
Criterion III.N on page 16). They also must complete 750 precepted direct patient-care
hours. A formal gap analysis must be performed to assess past graduate education,
including didactic clinical hours and courses.
16
CHAPTER IV: EVALUATION
"The [NNP] program has a formal comprehensive and systematic program evaluation
plan that determines program quality and the ongoing quality improvement (QI) process.
The QI process includes a plan for the overall assessment of the program, its policies
and resources, including faculty and students, curriculum, and evaluation with indicated
revisions" (NTF, 2022, p.17)
Graduates of NNP educational programs should be eligible to take the nationally
recognized certification exam. This national certification assesses the broad educational
preparation of the individual, including graduate core, APRN core, and NNP role/core
competencies and competencies specific to the neonatal population.
Curriculum Evaluation
Evaluation of the NNP program and curriculum should include:
• A systematic process to assess program outcomes with methods, metrics,
measures, and certification pass rates at a specified interval not to exceed 5
years (NTF, 2022, see Criterion IV.A on page 17)
• Documentation of NNP community interest in program relevancy (NTF, 2022;
see Criterion IV.D on page 17)
• Documentation of results of review to assess that curriculum reflects current
practice and trends in neonatology (NTF, 2022; see Criterion IV.D on page 17)
• Regular review of NNP program resources (eg, faculty, preceptors, clinical sites,
simulations) with implementation of ongoing QI that provides data to identify
deficiencies and gaps and to assist with concerns (NTF, 2022; see Criteria IV.B,
IV.C, and IV.E on page 17)
Faculty Evaluation
Faculty evaluation should include:
• Annual evaluation as set by individual institutional policy of faculty NNP
competency, licensure, and certification (NTF, 2022; see Criterion IV.F on page
18).
• Documentation of faculty course evaluations completed by students at end of
each course (NTF, 2022; see Criterion IV.G on page 18).
Student Evaluation
Ongoing student evaluation by faculty, student self-assessment, and achievement of
specific NNP competencies should include:
• Didactic experiences using summative and formative evaluations by faculty
(NTF, 2022; see Criterion IV.G on page 18).
• Clinical course experiences as evaluated by preceptors and faculty at midpoint
17
and completion of semester (NTF, 2022; see Criterion IV.H on page 18).
• Clinical experience evaluation completed by primary preceptor and recognizing
the input and involvement of additional preceptor(s).
• Contributions and feedback on performance (NTF, 2022; see Criterion IV.H on
page 18) related to delivery room experiences; patient management in primary,
acute, and chronic care settings; and procedural skills evaluation according to
semester goals and outcomes (NTF, 2022; see Criterion IV.G on page 18).
Preceptor(s) Evaluation
Preceptors are evaluated for appropriateness prior to clinical placement and throughout
the clinical experience by students and faculty (NTF, 2022; see Criterion IV.I on page
18).
NNPs are preferred as primary preceptors, and other neonatal- and pediatric-certified
providers may be considered and evaluated according to course goals and outcomes.
Clinical Site(s) Evaluation
NNP program faculty should provide oversight of the clinical learning environment.
Clinical sites are to be evaluated:
• By students and faculty for relevancy to course outcomes, learning experience
relevancy, and preceptor functionality (NTF, 2022; see NTF Criterion IV.I on
page 18)
• For student attainment of competencies over the course of the NNP program
inclusive of delivery-room experiences, history taking and management, prenatal
and nursery consultations, and experiences in the follow-up clinic, primary care,
and Level II, III, and IV NICUs.
The evaluation process may include, but is not limited to, physical and virtual site visits
and e-mail and phone consultations with the preceptor and agency administrators, as
well as students’ appraisal of the clinical learning environment.
A plan should be in place for reevaluation and interval evaluation of the site by faculty,
students, and preceptors.
Additional Areas for Evaluation
• Simulation experience evaluation (NTF, 2022; see Criterion IV.J on page 18)
should include student evaluation of each completed experience.
• Procedural skills simulation, which provides exposure and practice in preparation
for clinical experience according to NNP competencies, should be evaluated with
a process that includes student evaluation of each completed experience.

18
REFERENCES
American Association of Colleges of Nursing. (2006). The Essentials of Doctoral
Education for Advanced Nursing Practice.
https://www.aacnnursing.org/DNP/DNP-Essentials
American Association of Colleges of Nursing. (2021). The Essentials: Core
Competencies for Professional Nursing Education.
https://www.aacnnursing.org/Essentials/Download-Order
Benner, P. (1982). From novice to expert. The American Journal of Nursing, 82(3), 402–
407.
International Nursing Association for Clinical Simulation and Learning Standards
Committee. (2021). The Healthcare Simulation Standards of Best Practice.
TM
https://www.inacsl.org/healthcare-simulation-standards
Loewen, P., Legal, M., Gamble, A., Shah, K., Tkachuk, S., & Peter Zed, P. (2017).
Learner:preceptor ratios for practice-based learning across health disciplines: A
systematic review. Medical Education, 51(2), 146-157.
https://doi.org/10.1111/medu.13144
National Association of Neonatal Nurses. (n.d.) Position and consensus statements and
APRN publications. http://nann.org/about/position-statements
National Association of Neonatal Nurses. (2017). Education standards and curriculum
guidelines for neonatal nurse practitioner programs.
https://nann.org/uploads/2017_NNP_Education_Standards_completed_FINAL.pd
f
National Organization of Nurse Practitioner Faculties. (2013). Population-focused nurse
practitioner competencies.
https://www.aacnnursing.org/Portals/42/AcademicNursing/pdf/Population-
Focused-NP-Competencies-2013.pdf
National Organization of Nurse Practitioner Faculties. (2022). National Organization of
Nurse Practitioner Faculties' nurse practitioner role core competencies.
https://www.nonpf.org/page/NP_Role_Core_Competencies
National Task Force on Quality Nurse Practitioner Education. (2016). Criteria evaluation
of nurse practitioner programs, 5th edition, A report of the National Task Force
on Quality Nurse Practitioner Education.
https://cdn.ymaws.com/www.nonpf.org/resource/resmgr/Docs/EvalCriteria2016Fi
nal.pdf
National Task Force on Quality Nurse Practitioner Education. (2022). Standards for
quality nurse practitioner education, 6th edition, A report of the national task force

20
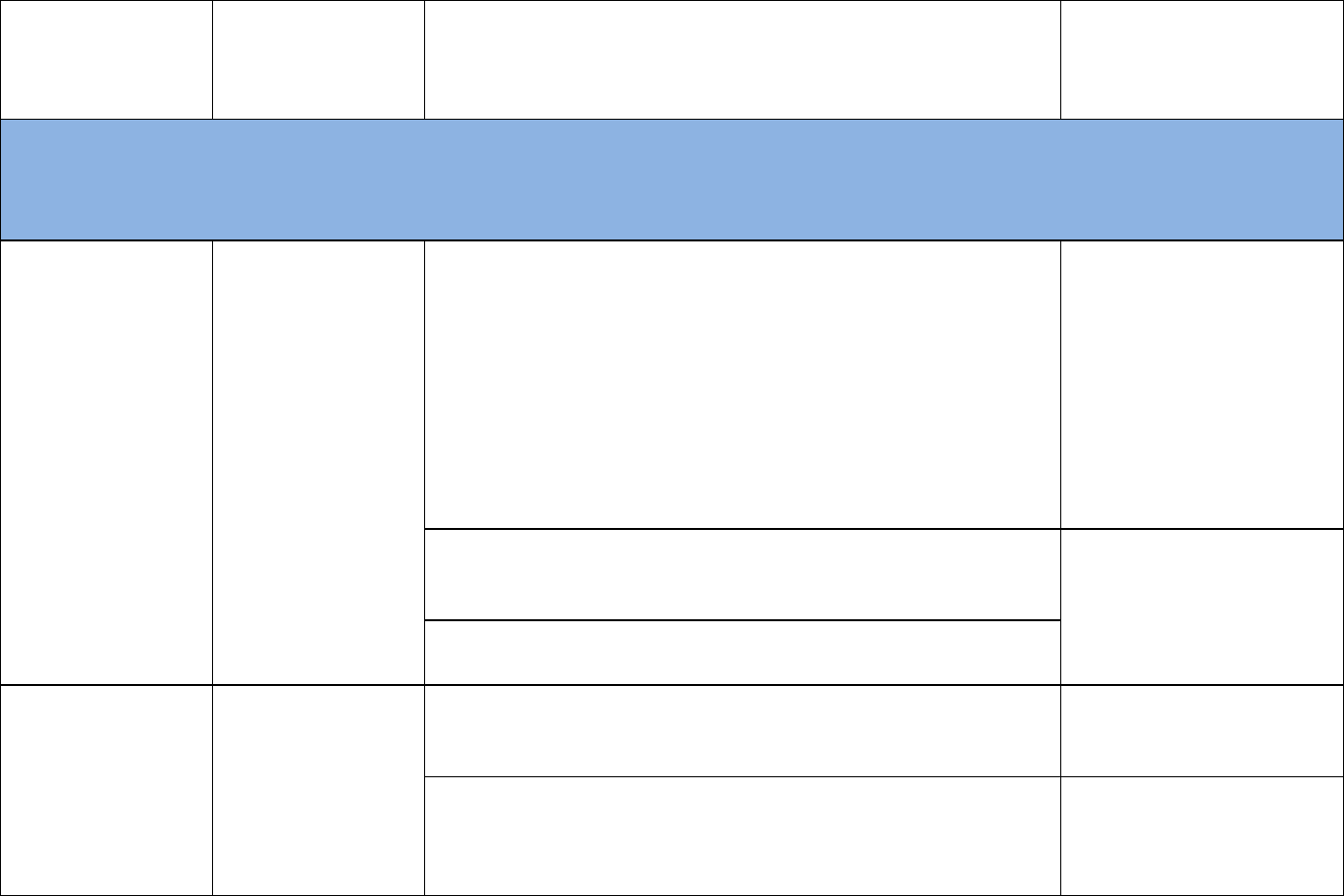
EDUCATION COMPETENCIES
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
DOMAIN 1: Knowledge for Nursing Practice
"Integration, translation, and application of established and evolving disciplinary nursing knowledge and ways of knowing, as well as knowledge from
other disciplines, including a foundation in liberal arts and natural and social sciences. This distinguishes the practice of professional nursing and forms
the basis for clinical judgment and innovation in nursing practice” (AACN, 2021, p. 27).
1.1: Demonstrate an
understanding of the
discipline of nursing’s
distinct perspective
and where shared
perspectives exist
with other disciplines
NP 1.1: Demonstrate
an understanding of
the discipline of
nursing’s and the NP
role’s distinct
perspectives and
where shared
perspectives exist
with other disciplines.
NP 1.1h: Integrate historical, foundational, and population-focused
knowledge into NP practice.
NNP 1.1: Articulate the
unique perspective of
neonatal advanced practice
and its contribution to the
collaborative care of ill and
convalescing children from
birth at any gestation to age
2, including episodic/acute
and primary care.
NP 1.1i: Translate evidence from nursing science and other sciences
into NP practice.
NP 1.1j: Evaluate the application of nursing science to NP practice.
1.2: Apply theory and
research‐based
knowledge from
nursing, the arts,
humanities, and
NP 1.2: Apply theory
and research-based
knowledge from
nursing, the arts,
humanities, and
NP 1.2k: Synthesize evidence from nursing and other disciplines to
inform and improve NP practice at micro, meso, and macro levels.
NP 1.2l: Translate science-based theories and concepts to guide
overall NP practice.

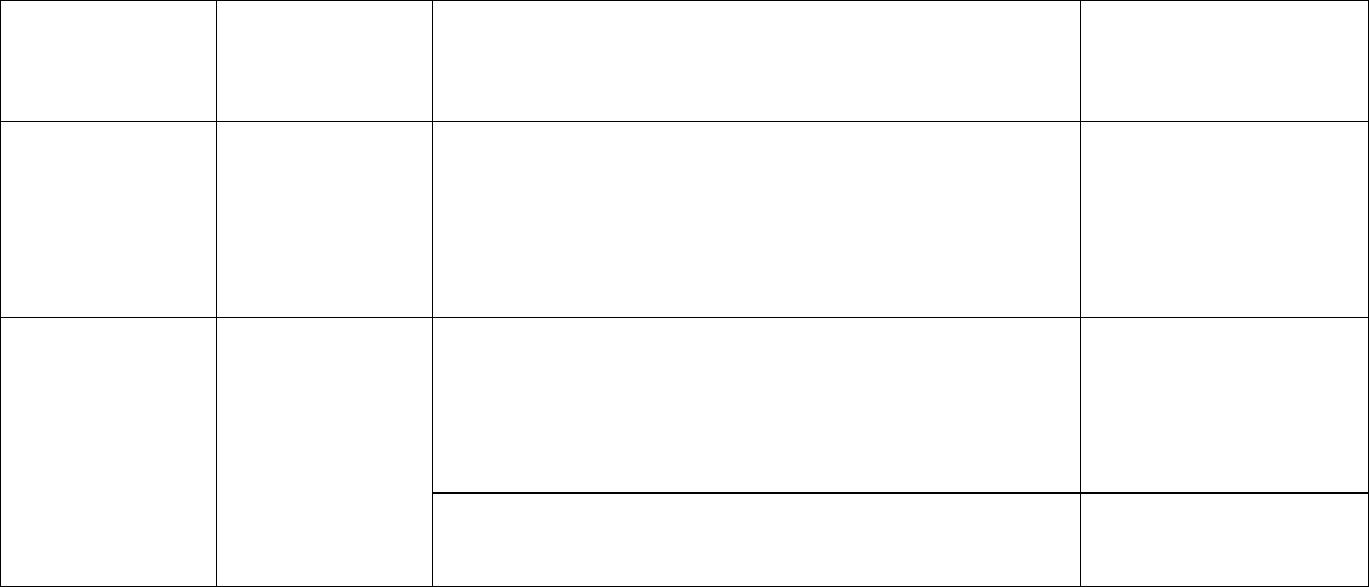
21
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
other sciences.
other sciences.
NP 1.2m: Employ ethical decision-making to manage and evaluate
patient care and population health.
NP 1.2n: Practice socially responsible leadership.
1.3: Demonstrate
clinical judgment
founded on a broad
knowledge base.
NP 1.3: Demonstrate
clinical judgment
founded on a broad
knowledge base.
NP1.3f: Demonstrate clinical judgment using a systematic approach to
inform, improve, and advance NP practice processes and outcomes.
NP 1.3g: Demonstrate clinical judgment to inform and improve NP
practice based on the foundational knowledge of advanced
physiology/pathophysiology, advanced health assessment, and
advanced pharmacology.
NNP 1.3: Demonstrate
critical thinking and
diagnostic reasoning skills
using knowledge of
embryology, neonatal
physiology and
pathophysiology,
assessment, pharmacology,
and developmental
milestones in the provision of
health care to children from
birth at any gestation to age
2.
NP1.3h: Synthesize current and emerging evidence to influence NP
practice.

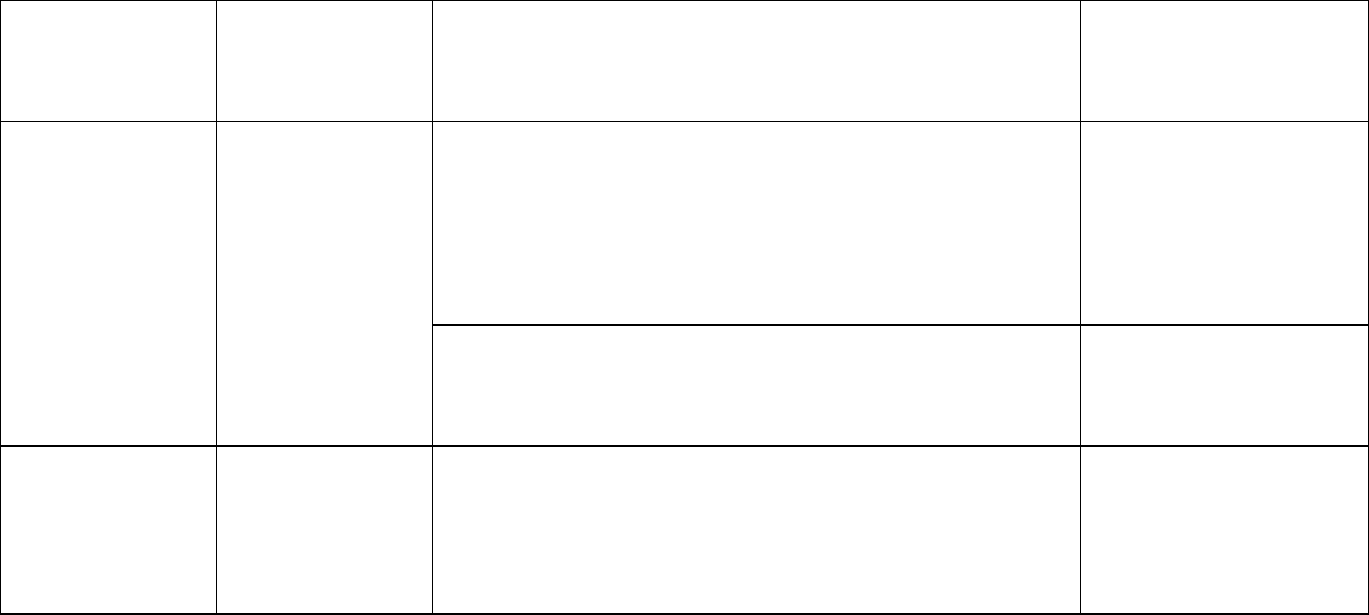
22
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
DOMAIN 2: Person Centered Care
“Person-centered care focuses on the individual within multiple complicated contexts, including family and/or important others. Person-centered care is
holistic, individualized, just, respectful, compassionate, coordinated, evidence-based, and developmentally appropriate. Person-centered care builds on a
scientific body of knowledge that guides nursing practice regardless of specialty or functional area (AACN, 2021, p. 29).
2.1: Engage with the
individual in
establishing a caring
relationship.
NP 2.1: Engage with
individuals and/or
caregivers in
establishing a caring
relationship
NP 2.1f: Practice holistic person-centered care to include
confidentiality, privacy, comfort, emotional support, mutual trust, and
respect.
NNP 2.1.1: Design
communication strategies
that recognize privacy and
confidentiality while
balancing the needs of the
child in relation to family
dynamics.
NP 2.1g: Engage in shared decision-making with consideration of
determinants of health.
NNP 2.1.2: Identify
individualized patient needs
informed by specific family
concerns including barriers
that may be related to social
determinants of health,
equity, diversity, and
inclusion.
2.2: Communicate
effectively with
NP 2.2:
Communicate
NP 2.2k: Utilize communication tools and techniques to promote
therapeutic relationships with individuals and/or caregiver.

23
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
individuals.
effectively with
individuals.
NP 2.2l: Apply motivational interviewing techniques to engage
individual and/or caregiver in management of health.
NP 2.2m: Communicate findings to the interprofessional team,
including the preceptor, in a systematic, concise manner to accurately
convey the health status of the patient.
NP 2.2n: Demonstrate empathy and compassion in communication
with others.
2.3: Integrate
assessment skills in
practice.
NP 2.3: Integrate
advanced
assessment in NP
practice.
NP2.3i: Utilize advanced critical thinking to determine the appropriate
focused or comprehensive relevant patient history.
NNP 2.3.1: Document a
thorough history including
medical, obstetrical, and
interim history.
NP 2.3j: Apply advanced assessment skills to perform a
comprehensive patient physical assessment utilizing appropriate
techniques.
NNP 2.3.2: Demonstrate
physical examination in a
concise, systematic
approach, employing
developmentally appropriate
care based on clinical
condition and gestational
age.
NP 2.3k: Apply advanced assessment skills to perform a focused
patient physical assessment utilizing appropriate techniques.

24
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
NP 2.3l: Order the appropriate diagnostic and screening tests based
on the patient’s risk factors and chief complaint.
NNP 2.3.3: Construct plans
for screening utilizing
evidence-based guidelines
specific for gestational
age/postconceptual age.
NP 2.3m: Identify health risk factors.
NNP 2.3.4: Develop
comprehensive problem list
relevant to obstetric and
interim history.
NP 2.3n: Evaluate determinants of health that may influence the
patient’s well-being.
NP 2.3o: Utilize appropriate evidence-based screening tools.
NP 2.3p: Document comprehensive history, screening, and
assessment.
NNP: 2.3.5: Recognize
behavioral cues and
developmental milestones
expected from birth at any
gestational age to age 2.

25
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
2.4: Diagnose actual
or potential health
problems and needs.
NP 2.4: Diagnose
actual or potential
health problems and
needs.
NP 2.4h: Analyze physical findings to differentiate between normal,
variations of normal, and signs of pathology to formulate actual and
differential diagnoses.
NP 2.4i: Utilize diagnostic reasoning to formulate actual and
differential diagnoses.
NNP 2.4.1: Identify and
perform appropriate
diagnostic procedures and
interventions for common
diagnoses for neonates and
children to age 2.
NNP 2.4.2: Analyze
laboratory and radiological
findings using
neonatal/pediatric-specific
reference values.
2.5: Develop a plan
of care.
NP 2.5: Manage care
of individuals
NP 2.5k: Provide holistic person-centered care by developing a
mutually acceptable, cost-conscious, and evidence-based plan of care.
NP 2.5l: Synthesize data to develop and initiate a person-centered
plan of care.
NNP 2.5.1: Construct plan of
care incorporating fetal
development, embryology,
and current postconceptual
age.

26
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
NP 2.5m: Prescribe medications safely and accurately using patient
data and following legal and regulatory guidelines.
NNP 2.5.2: Identify
appropriate pharmacological
therapy for gestational/
postconceptual age and
condition.
NNP 2.5.3: Describe legal
standards for prescriptive
authority locally and
nationally.
NP 2.5n: Order appropriate nonpharmacological interventions.
NNP 2.5.4: Compare and
contrast tools for pain
assessment inclusive of
gestational age,
pathophysiology, and
development.
NNP 2.5.5: Formulate plans
of care, inclusive of pain
management, using
pharmacological and
nonpharmacological
strategies.

27
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
NP 2.5o: Anticipate risks and take action to mitigate adverse events.
NNP 2.5.6: Intervene
according to established
standards of care to
resuscitate and stabilize
compromised newborns,
infants, and toddlers.
NP 2.5p: Incorporate health promotion, health maintenance, and
restoration of health into plans of care.
NNP 2.5.7: Develop a plan of
care that incorporates
appropriate growth,
development, and
anticipatory guidance for
children born at any gestation
to age 2.
2.6: Demonstrate
accountability for
care delivery.
NP 2.6: Demonstrate
accountability for
care delivery.
NP 2.6k: Provide healthcare services within scope-of-practice
boundaries, which include health promotion, disease prevention,
anticipatory guidance, counseling, disease management, palliative,
and end-of-life care.
NP 2.6l: Collaborate with the interprofessional team to formulate a
plan of care.
NP 2.6m: Order consultations or referrals based on evidence and
standards of professional care.

28
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
NP 2.6n: Document the comprehensive care provided.
NP 2.6o: Engage caregivers and support systems in care planning for
the individual.
2.7: Evaluate
outcomes of care.
NP 2.7: Evaluate
outcomes of care.
NP 2.7g: Evaluate individual outcomes based on evidence-based
interventions.
NP 2.7h: Revise plans of care based on effectiveness.
NP 2.7i: Analyze data to evaluate interventions, inequities, and gaps in
care.
2.8: Promote self‐
care management.
NP 2.8: Promote
self-care
management.
NP 2.8k: Integrate the principles of self-care management.
NP 2.8l: Incorporate coaching in patient and family self-care
management.
NNP 2.8.1: Utilize trauma-
informed care when working
with neonates and children to
age 2 and their families.
NNP 2.8.2: Assess family
and caregiver dynamics in
development of immediate
and long-term plans of care.

29
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
NP 2.8m: Create partnerships with community organizations to support
self-care management.
NNP 2.8.3: Initiate
consultations and referrals
for social and medical needs.
NNP 2.8.4: Distinguish and
document available
community resources to
assist families and
caregivers.
2.9: Provide care
coordination.
NP 2.9: Provide care
coordination.
NP 2.9k: Implement evidence-based guidelines and strategies that
enable effective transitions of care and care coordination.
NNP 2.9.1: Coordinate
successful transitions of care
between inpatient and
outpatient care with complete
documentation and
communication.

30
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
DOMAIN 3: Population Health
“Population health spans the healthcare delivery continuum from public health prevention to disease management of populations and describes
collaborative activities with both traditional and nontraditional partnerships from affected communities, public health, industry, academia, health care, local
government entities, and others for the improvement of equitable population health outcomes” (AACN, 2021, p. 33).
3.1: Manage
population health.
NP 3.1: Manage
population health.
NP 3.1o: Evaluate outcomes of population health using available
sources of data to inform NP practice, guidelines, and policies.
NNP 3.1.1: Appraise public
and private resources which
impact disease prevention,
care management, and
outcomes of children born at
any gestation.
NP 3.1p: Integrate findings of population health data to impact
competent care.
3.2: Engage in
effective
partnerships.
NP 3.2: Engage in
effective
partnerships.
NP 3.2i: Contribute clinical expertise and knowledge from advanced
practice to interprofessional efforts to protect and improve health.

31
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
3.3: Consider the
socioeconomic
impact of the delivery
of health care.
NP 3.3: Consider the
socioeconomic
impact of the delivery
of health care.
NP 3.3g: Appraise ethical, legal, and social factors to guide population
health policy development.
NNP 3.3.1: Incorporate
ethical, legal, and social
factors (including social
determinants of health,
equity, and inclusion) that
contribute to infant morbidity
and mortality in all spheres of
care when appraising health
policy.
3.4: Advance
equitable population
health policy
NP 3.4: Advance
equitable population
health policy.
NNP 3.4.1: Analyze
community and family
resources within the context
of complex systems when
planning care for children
born at any gestation to age
2.
3.5: Demonstrate
advocacy strategies.
NP 3.5: Demonstrate
advocacy strategies.
3.6: Advance
preparedness to
protect population
health during
disasters and public
NP 3.6: Advance
preparedness to
protect population
health during
disasters and public
NP 3.6k: Summarize the unique roles and responsibilities of NPs in
emergency preparedness and disaster response.
3.6l: Collaborate with a team to advance preparedness for potential
public health emergencies.

32
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
health emergencies.
health emergencies.
NP 3.6m: Evaluate the impact of globalization on population health.
33
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
DOMAIN 4: Scholarship for the Nursing Discipline
“The generation, synthesis, translation, application, and dissemination of nursing knowledge to improve health and transform health care” (AACN, 2021,
p. 37).
4.1: Advance the
scholarship of
nursing.
NP 4.1: Advance the
scholarship of NP
nursing practice.
NP 4.1n: Translate advanced practice knowledge to inform practice
and patient outcomes.
NNP 4.1.1: Apply knowledge
of basic research principles
to the care of children from
birth at any gestation to age
2.
NNP 4.1.2: Describe the
barriers associated with
research in the vulnerable
maternal/child population.
NP4.1o: Lead scholarly activities resulting in the focus of the
translation and dissemination of contemporary evidence into practice.
NP 4.1p: Apply clinical investigative skills to improve health outcomes.
4.2: Integrate best
evidence into nursing
practice.
NP 4.2: Integrate
best evidence into
NP practice.
NP 4.2l: Evaluate quality improvement processes and evidence-based
outcomes.
NP 4.2m: Disseminate findings from quality improvement,
implementation science, and research to improve healthcare delivery
and patient outcome.

34
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
4.3: Promote the
ethical conduct of
scholarly activities.
NP 4.3: Promote the
ethical conduct of
scholarly activities.
NP 4.3j: Translate knowledge from clinical practice to improve
population health outcomes through diversity, equity, and inclusion.
NP 4.3k: Utilize ethical principles to ensure participant safety through
scholarship activities.
NNP 4.3.1: Integrate legal
and ethical principles into the
health care of children from
birth at any gestation to age
2.

35
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
DOMAIN 5: Quality and Safety
“Employment of established and emerging principles of safety and improvement science. Quality and safety, as core values of nursing practice, enhance
quality and minimize risk of harm to patients and providers through both system effectiveness and individual performance” (AACN, 2021, p. 39).
5.1: Apply quality
improvement
principles in care
delivery.
NP 5.1: Apply quality
improvement
principles in care
delivery.
NP 5.1p: Systematically evaluate quality and outcomes of care using
quality improvement principles.
NNP 5.1.1: Utilize evidence-
based guidelines and
standards to develop care
strategies for the child from
birth at any gestation to age
2.
NP 5.1q: Evaluate the relationships and influence of access,
populations, cost, quality, and safety on health care.
NP 5.1r: Evaluate the impact of organizational systems in health care
to include care processes, financing, marketing, and policy.
5.2: Contribute to a
culture of patient
safety.
NP 5.2: Contribute to
a culture of patient
safety.
NP 5.2k: Build a culture of safety through quality improvement
methods and evidence-based interventions.
NNP 5.2.1: Engage in the
collection of neonatal-specific
quality measures and discuss
the impact of quality
improvement projects in
implementing best practice to
support safety.

36
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
5.3: Contribute to a
culture of provider
and work
environment safety.
NP 5.3: Contribute to
a culture of provider
and work
environment safety.

37
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
DOMAIN 6: Interprofessional Partnerships
“Intentional collaboration across professions and with care team members, patients, families, communities, and other stakeholders to optimize care,
enhance the healthcare experience, and strengthen outcomes” (AACN, 2021, p. 42).
6.1: Communicate in
a manner that
facilitates a
partnership approach
to quality care
delivery.
NP 6.1:
Communicate in a
manner that
facilitates a
partnership approach
to quality care
delivery.
NP6.1m: Engage in collaboration with multiple interprofessional
stakeholders (e.g., individuals, community, integrated health care
teams, and policy makers) to impact a diverse and inclusive healthcare
system.
NP 6.1n: Demonstrate equitable and quality health care through
interprofessional collaboration with the healthcare team.
NP 6.1o: Advocate for the patient as a member of the healthcare
team.
NP 6.1p: Demonstrate sensitivity to diverse organizations, cultures,
and populations.
6.2 Perform
effectively in different
team roles, using
principles and values
of team dynamics.
NP 6.2 Perform
effectively in different
team roles, using
principles and values
of team dynamics.
NP 6.2k: Assume different roles (e.g., member, leader) within the
interprofessional healthcare team.
NNP 6.2.1: Execute the roles
of leader, patient and family
advocate, educator,
consultant, and care
coordinator within the
neonatal interprofessional
healthcare team.
38
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
6.3 Use knowledge
of nursing and other
professions to
address healthcare
needs.
NP 6.3 Use
knowledge of nursing
and other
professions to
address healthcare
needs.
6.4: Work with other
professions to
maintain a climate of
mutual learning,
respect, and shared
values.
NP 6.4: Work with
other professions to
maintain a climate of
mutual learning,
respect, and shared
values.
NP 6.4j: Promote a climate of respect, dignity, inclusion, integrity,
civility, and trust to foster collaboration within the healthcare team.
NNP 6.4.1: Involve the child's
family and support system,
as defined by the family, as
vital members of the
healthcare team.
NP 6.4k: Collaborate to develop, implement, and evaluate healthcare
strategies to optimize safe, effective systems of care.

39
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
DOMAIN 7: Systems-Based Practice
“Responding to and leading within complex systems of health care. Nurses effectively and proactively coordinate resources to provide safe, quality, and
equitable care to diverse populations” (AACN, 2021, p. 44).
7.1: Apply
knowledge of
systems to work
effectively across the
continuum of care.
NP 7.1: Apply
knowledge of
systems to work
effectively across the
continuum of care.
NP 7.1i: Apply knowledge of organizational practices and complex
systems to improve healthcare delivery.
NNP 7.1.1: Manage the
transition of healthcare
needs—including
consultation and referral
respecting diversity, equity,
and inclusivity—for patients
from birth at any gestation to
age 2, as they transition
between acute, convalescing,
and primary care.
7.2: Incorporate
consideration of
cost‐effectiveness of
care.
NP 7.2: Incorporate
consideration of cost-
effectiveness of care.
NP 7.2m: Demonstrate fiduciary stewardship in the delivery of quality
care.
7.3: Optimize system
effectiveness through
application of
innovation and
evidence‐based
practice.
NP 7.3: Optimize
system effectiveness
through application
of innovation and
evidence-based
practice.

40
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
DOMAIN 8: Informatics and Healthcare Technologies
“Information and communication technologies and informatics processes are used to provide care, gather data, form information to drive decision making,
and support professionals as they expand knowledge and wisdom for practice. Informatics processes and technologies are used to manage and improve
the delivery of safe, high-quality, and efficient healthcare services in accordance with best practice and professional and regulatory standards” (AACN,
2021, p. 46).
8.1: Describe the
various information
and communication
technology tools
used in the care of
patients,
communities, and
populations.
NP 8.1: Appraise the
available information
and communication
technologies used in
the care of patients,
communities, and
populations.
NP 8.1l: Evaluate technologies and communication platforms in the
care of patients.
NNP 8.1.1: Assess the health
literacy and technological
access of families and
facilitate communication
methods to meet their needs.
8.2: Use information
and communication
technology to gather
data, create
information, and
generate knowledge.
8.2: Use information
and communication
technologies to
gather data, create
information, and
generate knowledge.
NP 8.2k: Analyze data to impact care delivery at the person,
population, or systems level.
NP 8.2l: Use technology systems to generate, analyze, and interpret
data on variables for the evaluation of health care.
NP 8.2m: Select appropriate technology and communication tools to
promote engagement and share credible information that is congruent
with patient needs, values, and learning styles.

41
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
8.3: Use information
and communication
technologies and
informatics
processes to deliver
safe nursing care to
diverse populations
in a variety of
settings.
NP 8.3: Use
information and
communication
technologies and
informatics
processes to deliver
safe care to diverse
populations in a
variety of settings.
8.4: Use information
and communication
technology to
support
documentation of
care and
communication
among providers,
patients, and all
system levels.
NP 8.4: Use
information and
communication
technology to
support
documentation of
care and
communication
among providers,
patients, and all
system levels.
NP 8.4h: Assess patients’ and caregivers’ learning and communication
needs to address gaps in access, knowledge, and information literacy.
NP 8.4i: Evaluate the design and implementation of clinical information
systems within the contexts of quality care, accountability, ethics, and
cost-effectiveness.

42
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
8.5: Use information
and communication
technologies in
accordance with
ethical, legal,
professional, and
regulatory standards
and workplace
policies in the
delivery of care.
NP 8.5: Use
information and
communication
technologies in
accordance with
ethical, legal,
professional, and
regulatory standards
and workplace
policies in the
delivery of care.
NP 8.5m: Use information technology safely, legally, and ethically to
manage data to ensure quality care and organizational accountability
to promote interprofessional communication.

43
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
DOMAIN 9: Professionalism
“Formation and cultivation of a sustainable professional identity, including accountability, perspective, collaborative disposition, and comportment, that
reflects nursing’s characteristics and values” (AACN, 2021, p. 49).
9.1: Demonstrate an
ethical comportment
in one's practice
reflective of nursing’s
mission to society.
NP 9.1: Demonstrate
an ethical
comportment in
one's practice
reflective of nursing's
mission to society.
NP 9.1l: Demonstrate the ability to apply ethical principles in complex
healthcare situations.
NNP 9.1.1: Construct care
strategies to deliver ethical
care management that is
culturally sensitive, inclusive,
and free of personal biases.
NP 9.1m: Develop strategies to prevent one’s own personal biases
from interfering with delivery of quality care.
NNP 9.1.2: Describe areas in
which implicit bias might
impact care of families and
children.
NP 9.1n: Actively seeks opportunities for continuous improvement in
professional practice.
9.2: Employ
participatory
approach to nursing
care.
NP 9.2: Employ
participatory
approach to NP care.
NP 9.2m: Demonstrate an NP professional identity.
NNP 9.2.1: Demonstrate
competent and safe practice
to the full scope of the NNP
role, including management
of patients at birth, born at
any gestation, and to age 2.

44
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
NP 9.2n: Demonstrate accountability to practice within the regulatory
standard and scope of educational preparation.
9.3: Demonstrate
accountability to the
individual, society,
and the profession.
NP 9.3: Demonstrate
accountability to the
individual, society,
and profession.
NP 9.3p: Participate in professional organizations to advance the NP
profession and improve health.
NNP 9.3.1: Contribute to
findings that can be utilized
to improve NNP and patient
specific outcomes in the care
of children from birth at any
gestation to age 2.
NP 9.3q: Reflect on past experiences to guide present and future
practice.
9.4: Comply with
relevant laws,
policies, and
regulations.
NP 9.4: Comply with
relevant laws,
policies, and
regulations.
NP 9.4i: Advocate for policies that support population-focus NPs to
practice at the full extent of their education.
NP 9.4j: Articulate the regulatory process that guides NP practice at
the national and individual state level.
P 9.4k: Analyze laws, policies, and regulations to describe scope of
practice in future population focus.
45
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
9.5: Demonstrate the
professional identity
of nursing.
NP 9.5: Demonstrate
the professional
identity of nursing.
NP 9.5j: Articulate NPs’ unique professional identity to other
interprofessional team members and the public.
NNP 9.5.1: Differentiate to
families and the community
of interest the role of the
NNP as compared to other
members of the
interdisciplinary team.
NP 9.5k: Demonstrate the ability to effectively educate and mentor
peers, students, [and] members of the interprofessional healthcare
team.
9.6: Integrate
diversity, equity, and
inclusion as core to
one’s professional
identity.
NP 9.6: Integrate
diversity, equity, and
inclusion as core to
one’s professional
identity.

46
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
DOMAIN 10: Personal, Professional and Leadership Development:
“Participation in activities and self-reflection that foster personal health, resilience, and well-being; contribute to lifelong learning; and support the
acquisition of nursing expertise and the assertion of leadership” (AACN, 2021, p. 53).
10.1: Demonstrate a
commitment to
personal health and
well‐being.
NP 10.1:
Demonstrate a
commitment to
personal health and
well-being.
NP 10.1e: Create an environment that promotes self-care, health, and
well-being.
NP 10.1f: Support whole-person health and holistic well-being of self.
10.2: Demonstrate a
spirit of inquiry that
fosters flexibility and
professional maturity.
NP 10.2:
Demonstrate
professional maturity.
NP 10.2k: Demonstrate responsibility to practice in the NP population
focus area defined by one’s education, certification, and license.
NNP 10.2.1: Demonstrate
critical advanced-practice
thinking and decision-making
ability beyond the scope of
the RN and within the scope
of the NNP.
NNP 10.2.2: Engage in self-
reflection and respond to
professional feedback
regarding one’s growth in the
NNP role along the novice to
expert continuum.
NP 10.2l: Employ empathy to communicate effectively.
NP 10.2m: Conduct oneself in a professional manner.

47
Competency
(AACN, 2021)
NP Role Core
Competencies
(NONPF, 2022)
NP Role Core
Subcompetencies
(NONPF, 2022)
NNP
Competencies
(NANN/NANNP, 2022)
NP 10.2n: Uphold standards of the NP profession.
10.3: Develop
capacity for
leadership.
NP 10.3: Develop
capacity for
leadership.
NP 10.3r: Articulate the complex leadership role of the NP.
NP 10.3s: Execute leadership skills in the translation of new
knowledge to improve outcomes.
NP 10.3t: Provide leadership on teams, and in different team roles,
across a variety of practice settings.
NP 10.3u: Mentor peers.
NP 10.3v: Engage in advocacy efforts to address health disparities,
social justice, and equity to improve healthcare outcomes.
Note. Table adapted with permission from The Essentials: Core Competencies for Professional Nursing Education by American Association of Colleges of Nursing, 2021
(Competency column) and from Nurse Practitioner Role Core Competencies by National Organization of Nurse Practitioner Faculties, 2022 (NP Role Core Competencies and NP
Role Core Subcompetencies columns). The NNP Competencies column content was developed by NANNP for this publication and is available in Appendix A. AACN’s Domains,
which were reprinted with permission in this table, are also available in Appendix D. Further detail is available through the Concepts in Appendix D, which are also reprinted with
permission from AACN.
48
APPENDICES
Appendix A: 2023 NNP Competencies List
Knowledge for Nursing Practice
NNP 1.1: Articulate the unique perspective of neonatal advanced practice and its
contribution to the collaborative care of ill and convalescing children from birth at any
gestation to age 2, including episodic/acute and primary care.
NNP 1.3: Demonstrate critical thinking and diagnostic reasoning skills using knowledge
of embryology, neonatal physiology and pathophysiology, assessment, pharmacology,
and developmental milestones in the provision of health care to children from birth at
any gestation to age 2.
Person-Centered Care
NNP 2.1.1: Design communication strategies that recognize privacy and confidentiality
while balancing the needs of the child in relation to family dynamics.
NNP 2.1.2: Identify individualized patient needs informed by specific family concerns
including barriers that may be related to social determinants of health, equity, diversity,
and inclusion.
NNP 2.3.1: Document a thorough history including medical, obstetrical, and interim
history.
NNP 2.3.2: Demonstrate physical examination in a concise, systematic approach,
employing developmentally appropriate care based on clinical condition and gestational
age.
NNP 2.3.3: Construct plans for screening utilizing evidence-based guidelines specific
for gestational age/postconceptual age.
NNP 2.3.4: Develop comprehensive problem list relevant to obstetric and interim
history.
NNP: 2.3.5: Recognize behavioral cues and developmental milestones expected from
birth at any gestational age to age 2.
NNP 2.4.1: Identify and perform appropriate diagnostic procedures and interventions for
common diagnoses for neonates and children to age 2.
NNP 2.4.2: Analyze laboratory and radiological findings using neonatal/pediatric-
specific reference values.
NNP 2.5.1: Construct plan of care incorporating fetal development, embryology, and
current postconceptual age.
NNP 2.5.2: Identify appropriate pharmacological therapy for gestational/postconceptual
age and condition.
49
NNP 2.5.3: Describe legal standards for prescriptive authority locally and nationally.
NNP 2.5.4: Compare and contrast tools for pain assessment inclusive of gestational
age, pathophysiology, and development.
NNP 2.5.5: Formulate plans of care, inclusive of pain management, using
pharmacological and nonpharmacological strategies.
NNP 2.5.6: Intervene according to established standards of care to resuscitate and
stabilize compromised newborns, infants, and toddlers.
NNP 2.5.7: Develop a plan of care that incorporates appropriate growth, development,
and anticipatory guidance for children born at any gestation to age 2.
NNP 2.8.1: Utilize trauma-informed care when working with neonates and children to
age 2 and their families.
NNP 2.8.2: Assess family and caregiver dynamics in development of immediate and
long-term plans of care.
NNP 2.8.3: Initiate consultations and referrals for social and medical needs.
NNP 2.8.4: Distinguish and document available community resources to assist families
and caregivers.
NNP 2.9.1: Coordinate successful transitions of care between inpatient and outpatient
care with complete documentation and communication.
Population Health
NNP 3.1.1: Appraise public and private resources which impact disease prevention,
care management, and outcomes of children born at any gestation.
NNP 3.3.1: Incorporate ethical, legal, and social factors (including social determinants
of health, equity, and inclusion) that contribute to infant morbidity and mortality in all
spheres of care when appraising health policy.
NNP 3.4.1: Analyze community and family resources within the context of complex
systems when planning care for children born at any gestation to age 2.
Scholarship for the Nursing Discipline
NNP 4.1.1: Apply knowledge of basic research principles to the care of children from
birth at any gestation to age 2.
NNP 4.1.2: Describe the barriers associated with research in the vulnerable
maternal/child population.
NNP 4.3.1: Integrate legal and ethical principles into the health care of children from
birth at any gestation to age 2.
50
Quality and Safety
NNP 5.1.1: Utilize evidence-based guidelines and standards to develop care strategies
for the child from birth at any gestation to age 2.
NNP 5.2.1: Engage in the collection of neonatal-specific quality measures and discuss
the impact of quality improvement projects in implementing best practice to support
safety.
Interprofessional Partnerships
NNP 6.2.1: Execute the roles of leader, patient and family advocate, educator,
consultant, and care coordinator within the neonatal interprofessional healthcare team.
NNP 6.4.1: Involve the child's family and support system, as defined by the family, as
vital members of the healthcare team.
Systems-Based Practice
NNP 7.1.1: Manage the transition of healthcare needs—including consultation and
referral respecting diversity, equity, and inclusivity—for patients from birth at any
gestation to age 2, as they transition between acute, convalescing, and primary care.
Informatics and Healthcare Technologies
NNP 8.1.1: Assess the health literacy and technological access of families and facilitate
communication methods to meet their needs.
Professionalism
NNP 9.1.1: Construct care strategies to deliver ethical care management that is
culturally sensitive, inclusive, and free of personal biases.
NNP 9.1.2: Describe areas in which implicit bias might impact care of families and
children.
NNP 9.2.1: Demonstrate competent and safe practice to the full scope of the NNP role,
including management of patients at birth, born at any gestation and to age 2.
NNP 9.3.1: Contribute to findings that can be utilized to improve NNP and patient
specific outcomes in the care of children from birth at any gestation to age 2.
NNP 9.5.1: Differentiate to families and the community of interest the role of the NNP as
compared to other members of the interdisciplinary team.
Personal, Professional and Leadership Development
NNP 10.2.1: Demonstrate critical advanced-practice thinking and decision-making
ability beyond the scope of the RN and within the scope of the NNP.
NNP 10.2.2: Engage in self-reflection and respond to professional feedback regarding
one’s growth in the NNP role along the novice to expert continuum.
51
Appendix B: Suggested Responsibilities and Activities
Suggested Student Responsibilities
• Discuss specific clinical objectives, schedules, and general guidelines with the
preceptor and faculty prior to the clinical rotation.
• Adhere to the standards and scope of professional practice.
• Communicate with the preceptor and faculty on clinical progress and learning
needs.
• Demonstrate independent learning, diagnostic reasoning skills, and the use of
available resources.
• Maintain and submit a log of clinical skills and activities.
• Complete self-evaluations and evaluations of the preceptor and clinical site as
required.
Suggested Preceptor Responsibilities
• Meet with the student prior to the beginning of the clinical experience to discuss
clinical objectives, schedules, guidelines, and unit standardized procedures and
protocols. The preceptor should inform the student of any institutional orientation
requirements.
• Assign an initial caseload of patients. Expansion of the caseload will depend on
the evaluation of the student’s readiness, knowledge, and skill level.
• Permit the student to perform all the required management activities for assigned
patients under appropriate supervision. See Suggested Student Activities below.
• Provide direct supervision when the student is involved in patient care and review
and provide feedback on the student’s documentation.
• Meet with the student on an ongoing basis to discuss specific learning objectives
and experiences.
• Communicate with faculty throughout the preceptorship to provide feedback on
student progression and any deficits.
• Contact the program director or appropriate faculty member in a timely fashion
with concerns or questions regarding the preceptor’s ability to fulfill
responsibilities or the student's performance.
• Provide written evaluation of the student’s clinical performance during and at the
end of the preceptorship.
Suggested Student Learning Activities:
• Participate in the resuscitation and stabilization of neonates in the delivery room.
• Admit patients to the nursery, obtaining perinatal and neonatal history,
performing physical examinations, developing the differential diagnosis, and
proposing the initial management plan.
• Provide ongoing management of infants in collaboration with the preceptor and
revise the management plan based on the evaluation of the infant's progress.
• Perform diagnostic tests and procedures as dictated by the status and needs of
the patient.
• Respond to emergency situations to stabilize an infant.
52
• Document infant’s’ clinical status, plan of care, and response to therapy in their
medical records.
• Evaluate the need for consultations and request them.
• Facilitate an understanding of infant’s’ current and future healthcare needs and
provide support to parents and staff.
• Develop discharge plans.
• Participate in postdischarge primary-care management
• Participate in high-risk newborn transport if this service is available and if the
hospital permits student participation.
• Provide staff development by participating in educational programs.
53
Appendix C: 2021 AACN Domains
In The Essentials: Core Competencies for Professional Nursing Education (2021), the
American Association of Colleges of Nursing (AACN) detailed 10 domains that act as
the “descriptive framework for the practice of nursing” (AACN, 2021, p. 10). They are
reprinted here with AACN’s permission.
Domain 1: Knowledge for Nursing Practice
Descriptor: Integration, translation, and application of established and evolving
disciplinary nursing knowledge and ways of knowing, as well as knowledge from other
disciplines, including a foundation in liberal arts and natural and social sciences. This
distinguishes the practice of professional nursing and forms the basis for clinical
judgment and innovation in nursing practice.
Domain 2: Person‐Centered Care
Descriptor: Person‐centered care focuses on the individual within multiple complicated
contexts, including family and/or important others. Person‐centered care is holistic,
individualized, just, respectful, compassionate, coordinated, evidence‐based, and
developmentally appropriate. Person‐centered care builds on a scientific body of
knowledge that guides nursing practice regardless of specialty or functional area.
Domain 3: Population Health
Descriptor: Population health spans the healthcare delivery continuum from public
health prevention to disease management of populations and describes collaborative
activities with both traditional and non‐traditional partnerships from affected
communities, public health, industry, academia, health care, local government entities,
and others for the improvement of equitable population health outcomes.
Domain 4: Scholarship for Nursing Practice
Descriptor: The generation, synthesis, translation, application, and dissemination of
nursing knowledge to improve health and transform health care.
Domain 5: Quality and Safety
Descriptor: Employment of established and emerging principles of safety and
improvement science. Quality and safety, as core values of nursing practice, enhance
quality and minimize risk of harm to patients and providers through both system
effectiveness and individual performance.
Domain 6: Interprofessional Partnerships
Descriptor: Intentional collaboration across professions and with care team members,
patients, families, communities, and other stakeholders to optimize care, enhance the
healthcare experience, and strengthen outcomes.
Domain 7: Systems‐Based Practice
Descriptor: Responding to and leading within complex systems of health care. Nurses
effectively and proactively coordinate resources to provide safe, quality, equitable care
to diverse populations.
54
Domain 8: Information and Healthcare Technologies
Descriptor: Information and communication technologies and informatics processes are
used to provide care, gather data, form information to drive decision making, and
support professionals as they expand knowledge and wisdom for practice. Informatics
processes and technologies are used to manage and improve the delivery of safe, high-
quality, and efficient healthcare services in accordance with best practice and
professional and regulatory standards.
Domain 9: Professionalism
Descriptor: Formation and cultivation of a sustainable professional nursing identity,
accountability, perspective, collaborative disposition, and comportment that reflects
nursing's characteristics and values.
Domain 10: Personal, Professional, and Leadership Development
Descriptor: Participation in activities and self‐reflection that foster personal health,
resilience, and well‐being, lifelong learning, and support the acquisition of nursing
expertise and assertion of leadership.
55
Appendix D: 2021 AACN CONCEPTS
AACN also created featured concepts for The Essentials: Core Competencies for
Professional Nursing Education. They “are not of ‘lesser importance’ than a domain.
Each of these concepts serves as a core component of knowledge, facts, and skills
across multiple situations and contexts within nursing practice,” according to AACN
(2021, p. 12). The featured concepts are reprinted here with AACN’s permission.
Clinical Judgment
As one of the key attributes of professional nursing, clinical judgment refers to the
process by which nurses make decisions based on nursing knowledge (evidence,
theories, ways/patterns of knowing), other disciplinary knowledge, critical thinking, and
clinical reasoning. This process is used to understand and interpret information in the
delivery of care. Clinical decision making based on clinical judgment is directly related to
care outcomes.
Communication
Communication, informed by nursing and other theories, is a central component in all
areas of nursing practice. Communication is defined as an exchange of information,
thoughts, and feelings through a variety of mechanisms. The definition encompasses
the various ways people interact with each other, including verbal, written, behavioral,
body language, touch, and emotion. Communication also includes intentionality,
mutuality, partnerships, trust, and presence. Effective communication between nurses
and individuals and between nurses and other health professionals is necessary for the
delivery of high quality, individualized nursing care. With increasing frequency
communication is delivered through technological modalities. Communication also is a
core component of team‐based, interprofessional care and closely interrelated with the
concept Social Determinants of Health (described below).
Compassionate Care
As an essential principle of person‐centered care, compassionate care refers to the way
nurses relate to others as human beings and involves “noticing another person's
vulnerability, experiencing an emotional reaction to this, and acting in some way with
them in a way that is meaningful for people.” Compassionate care is interrelated with
other concepts such as caring, empathy, and respect and is also closely associated with
patient satisfaction.
Diversity, Equity, and Inclusion
Collectively, diversity, equity, and inclusion (DEI) refers to a broad range of individual,
population, and social constructs and is adapted in the Essentials as one of the most
visible concepts. Although these are collectively considered a concept, differentiation of
each conceptual element leads to enhanced understanding. Diversity references a
broad range of individual, population, and social characteristics, including but not limited
to age; sex; race; ethnicity; sexual orientation; gender identity; family structures;
geographic locations; national origin; immigrants and refugees; language; any
impairment that substantially limits a major life activity; religious beliefs; and
56
socioeconomic status. Inclusion represents environmental and organizational cultures in
which faculty, students, staff, and administrators with diverse characteristics thrive.
Inclusive environments require intentionality and embrace differences, not merely
tolerate them. Everyone works to ensure the perspectives and experiences of others
are invited, welcomed, acknowledged, and respected in inclusive environments. Equity
is the ability to recognize the differences in the resources or knowledge needed to allow
individuals to fully participate in society, including access to higher education, with the
goal of overcoming obstacles to ensure fairness. To have equitable systems, all people
should be treated fairly, unhampered by artificial barriers, stereotypes, or prejudices.
Two related concepts that fit within DEI include structural racism and social justice.
Ethics
Core to professional nursing practice, ethics refers to principles that guide a person's
behavior. Ethics is closely tied to moral philosophy involving the study of or examination
of morality through a variety of different approaches. There are commonly accepted
principles in bioethics that include autonomy, beneficence, non‐maleficence, and
justice. The study of ethics as it relates to nursing practice has led to the exploration of
other relevant concepts, including moral distress, moral hazard, moral community, and
moral or critical resilience.
Evidence‐Based Practice
The delivery of optimal health care requires the integration of current evidence and
clinical expertise with individual and family preferences. Evidence‐based practice is
problem-solving approach to the delivery of health care that integrates best evidence
from studies and patient care data with clinician expertise and patient preferences and
values. In addition, there is a need to consider those scientific studies that ask: whose
perspectives are solicited, who creates the evidence, how is that evidence created,
what questions remain unanswered, and what harm may be created. Answers to these
questions are paramount to incorporating meaningful, culturally safe, evidence‐based
practice.
Health Policy
Health policy involves goal directed decision‐making about health that is the result of an
authorized public decision‐making process. Nurses play critical roles in advocating for
policy that impacts patients and the profession, especially when speaking with a united
voice on issues that affect nursing practice and health outcomes. Nurses can have a
profound influence on health policy by becoming engaged in the policy process on
many levels, which includes interpreting, evaluating, and leading policy change.
Social Determinants of Health
Determinants of health, a broader term, include personal, social, economic, and
environmental factors that impact health. Social determinants of health, a primary
component of determinants of health "are the conditions in the environment where
people are born, live, learn, work, play, worship, and age that affect a wide range of
health, functioning, and quality of life outcomes and risks."

