
1
NIH STRATEGIC PLAN FOR DATA SCIENCE
Introduction
As articulated in the National Institutes of Health (NIH)-Wide Strategic Plan
1
and the Department of
Health and Human Services (HHS) Strategic Plan,
2
our nation and the world stand at a unique moment of
opportunity in biomedical research, and data science is an integral contributor. Understanding basic
biological mechanisms through NIH-funded research depends upon vast amounts of data and has
propelled biomedicine into the sphere of “Big Data” along with other sectors of the national and global
economies. Reflecting today’s highly integrated biomedical research landscape, NIH defines data science
as “the interdisciplinary field of inquiry in which quantitative and analytical approaches, processes, and
systems are developed and used to extract knowledge and insights from increasingly large and/or
complex sets of data.”
NIH supports the generation and analysis of substantial quantities of biomedical research data (see, for
example, text box “Big Data from the Resolution Revolution
3
”), including numerous quantitative and
qualitative datasets emanating from fundamental research using model organisms (such as mice, fruit
flies, and zebrafish), clinical studies (including
medical images), and observational and
epidemiological studies (including data from
electronic health records and wearable devices).
Metadata, “data about data,” provides
information such as data content, context, and
structure, which is also valuable to the biomedical
research community as it affects the ability of
data to be found and used. One example of
metadata is bibliographic information such as a
publication’s authors, format (e.g., pdf), and
location (DOI, or digital object identifier) that are
contained within any reference citation.
By 2025, the total amount of genomics data alone
is expected to equal or exceed totals from the three other major producers of large amounts of data:
1
NIH-Wide Strategic Plan Fiscal Years 2016-2020: Available at: https://www.nih.gov/sites/default/files/about-
nih/strategic-plan-fy2016-2020-508.pdf
2
Department of Health and Human Services Strategic Plan 2018-2022: Available at:
https://www.hhs.gov/about/strategic-plan/index.html
3
Baldwin PR, Tan YZ, Eng ET, Rice WJ, et al. Big data in cryoEM: automated collection, processing and accessibility
of EM data. Curr Open Microbiology 2018;43:1–8.
Big Data from the Resolution Revolution
One of the revolutionary advances in microscope,
detectors, and algorithms, cryogenic electron
microscopy (cryoEM) has become one of the areas of
science (along with astronomy, collider data, and
genomics) that have entered the Big Data arena,
pushing hardware and software requirements to
unprecedented levels. Current cryoEM detector
systems are fast enough to collect movies instead of
single integrated images, and users now typically
acquire up to 2,000 movies in a single day. As is the
case with astronomy, collider physics, and genomics,
scientists using cryoEM generate several terabytes of
data per day.

2
astronomy, YouTube, and Twitter.
4
Indeed, next-generation sequencing data, stored at NIH’s National
Center for Biotechnology Information (NCBI), has been growing exponentially for many years and shows
no signs of slowing (see Fig. 1, below).
The generation of most biomedical data is highly distributed and is accomplished mainly by individual
scientists or relatively small groups of researchers. Moreover, data also exist in a wide variety of formats,
which complicates the ability of researchers to find and use biomedical research data generated by others
and creates the need for extensive data “cleaning.” According to a 2016 survey, data scientists across a
wide array of fields said they spend most of their work time (about 80 percent) doing what they least like
to do: collecting existing datasets and organizing data.
5
That leaves less than 20 percent of their time for
creative tasks like mining data for patterns that lead to new research discoveries.
Figure 1. Growth of NCBI Data and Services, 1989-2017 Credit: NCBI
4
Stephens, et al., Big Data: Astronomical or Genomical? PLOS Biology 2015 (July 7, 2015) Available at:
http://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.1002195
5
CrowdFlower 2016 Data Science Report. Available at: http://visit.crowdflower.com/rs/416-ZBE-
142/images/CrowdFlower_DataScienceReport_2016.pdf

3
A New Era for Biomedical Research
Adv
ances in storage, communications, and processing have led to new research methods and tools that
were simply not possible just a decade ago. Machine learning, deep learning,
artificial intelligence, and virtual-reality technologies are examples of data-
related innovations that may yield transformative changes for biomedical
research over the coming decade. The ability to experiment with new ways
to optimize technology-intensive research will inform decisions regarding
future policies, approaches, and business practices, and will allow NIH to adopt more cost-effective ways
to capture, access, sustain, and reuse high-value biomedical data resources in the future. To this end,
NIH must weave its existing data-science efforts into the larger data ecosystem and fully intends to take
advantage of current and emerging data-management and technological expertise, computational
platforms, and tools available from the commercial sector through a variety of innovative public-private
partnerships.
Th
e fastest supercomputers in the world today perform a quadrillion (10
15
) calculations each second:
known as the petascale level. The next frontier is exascale computing (which is 1,000 times faster than
petascale, or a quintillion (10
18
) calculations each second). Reaching exascale-level computing is a
technical milestone that is expected to have profound impacts on everyday life. At the exascale level of
computing speed, supercomputers will be able to more realistically mimic the speed of life operating
inside the human body, enabling promising new avenues of pursuit for biomedical research that involves
clinical data. These data-intensive programs may well be among the earliest adopters and drivers of
exascale computing: They include the All of Us Research Program and the Cancer Moonshot
SM
components of the Precision Medicine Initiative, the Human Connectome project, the Brain Research
through Advancing Innovative Neurotechnologies (BRAIN
) initiative, and many others.
Clinical Data and Information Security
Throughout the research enterprise, NIH must continue to balance the need for maximizing
opportunities to advance biomedical research with responsible strategies for sustaining public trust,
participant safety, and data security. Proper handling of the vast domain of clinical data that is being
continually generated from a range of data producers is a challenge for NIH and the biomedical research
community, including the private sector. Patient-related data is both quantitative and qualitative and
can arise from a wide array of sources, including specialized research projects and trials; epidemiology;
genomic analyses; clinical-care processes; imaging assessments; patient-reported outcomes;
environmental-exposure records; and a host of social indicators now linked to health such as
educational records, employment history, and genealogical records. NIH must develop, promote, and
practice robust and proactive information-security approaches to ensure appropriate stewardship of
patient data and to enable scientific advances stemming from authentic, trusted data sources. NIH will
ensure that clinical-data collection, storage, and use adheres to stringent security requirements and
applicable law, to protect against data compromise or loss. NIH will also comply with the
Health
Note: Please see Glossary
for definitions of terms
related to data science.

4
Insurance Portability and Accountability Act of 1996 (HIPAA) Security Rule and National Institute of
Standards and Technology (NIST) health-information security standards.
D
ata quality and integrity must be maintained at all stages of the research life cycle—from collection
through curation, use, dissemination, and retirement. It is essential that NIH implement comprehensive
security controls consistent with the risk of harm if data are breached or corrupted. NIH must also
continually revisit its approaches to keep pace with ever-increasing information security threats that
arise in the global information technology environment. This work must be done in close partnership
with private, public, and academic entities that have expertise in information security and related areas,
ensuring stringent security measures.
Current Data Science Challenges for NIH
A
s an initial step to strengthen the NIH approach to data science, in 2014, the NIH Director created a
unique position, the Associate Director for Data Science, to lead NIH in advancing data science across
the Agency, and established the Big Data to Knowledge
(BD2K) program. NIH’s past investment in the
BD2K software-development initiative launched in 2014 produced a number of tools and methods that
can now be refined and made available to help tackle a variety of challenges. These include data-
compression formats, suites of algorithms, web-based software, application-programming interfaces
(APIs), public databases, computational approaches, among others.
I
n subsequent years, NIH's needs have evolved, and as such the agency has established a new position
to advance NIH data science across the extramural and intramural research communities. The inaugural
NIH Chief Data Strategist, in close collaboration with the NIH Scientific Data Council and NIH Data
Science Policy Council, will guide the development and implementation of NIH’s data-science activities
and provide leadership within the broader biomedical research data ecosystem. This new leadership
position will also forge partnerships with federal advisory bodies (including the HHS Data Council and
the HHS Chief Information Officer Council); HHS Staff Divisions, including the Office of the Chief
Technology Officer (OCTO), the Office of the National Coordinator for Health Information
Technology (ONC), and the Office of the Chief Information Officer (OCIO); and other federal agencies
(National Science Foundation (NSF), Department of Energy (DOE), and others) as well as international
funding agencies; and with the private sector. These collaborations are essential to ensure synergy and
efficiency and to prevent unnecessary duplication of efforts.
A
s a result of the rapid pace of change in biomedical research and information technology, several
pressing issues related to the data-resource ecosystem confront NIH and other components of the
biomedical research community, including:
• The growing costs of managing data could diminish NIH’s ability to enable scientists to generate
data for understanding biology and improving health.
• The current data-resource ecosystem tends to be “siloed” and is not optimally integrated o
r
interconnected.

5
• Important datasets exist in many different formats and are often not easily shared, findable, or
interoperable.
• Historically, NIH has often supported data resources using funding approaches designed for research
projects, which has led to a misalignment of objectives and review expectations.
• Funding for tool development and data resources has become entangled, making it difficult to
assess the utility of each independently and to optimize value and efficiency.
• There is currently no general system to transform, or harden, innovative algorithms and tools
created by academic scientists into enterprise-ready resources that meet industry standards of ease
of use and efficiency of operation.
As a p
ublic steward of taxpayer funds, NIH must think and plan carefully to ensure that its resources are
spent efficiently toward extracting the most benefit from its investments. Because of these issues, NIH
has adopted a unified vision, and a corporate strategy for attaining that vision, that will best serve the
biomedical research enterprise in the coming decades.
Plan Content and Implementation
Thi
s document, the NIH Strategic Plan for Data Science describes NIH’s Overarching Go
als, Strategic
Objectives, and Implementation Tactics for modernizing the NIH-funded biomedical data-resource
ecosystem. In establishing this plan, NIH addresses storing data efficiently and securely; making data
usable to as many people as possible (including researchers, institutions, and the public); developing a
research workforce poised to capitalize on advances in data science and information technology; and
setting policies for productive, efficient, secure, and ethical data use. As articulated herein, this strategic
plan commits to ensuring that all data-science activities and products supported by the agency adhere
to the FAIR principles, meaning that data be Findable, Accessible, Interoperable, and Reusable (see text
box “What is FAIR?”).
6
6
Wilkinson MD et al. The FAIR Guiding Principles for scientific data management and stewardship. Sci Data.
2016;3:160018.

6
R
ecognizing the rapid course of evolution of
data science and technology, this plan maps
a general path for the next five years but is
intended to be as nimble as possible to
adjust to undiscovered concepts and
products derived from current investments
from NIH and elsewhere in the public and
private sectors. Frequent course corrections
are likely based upon the needs of NIH and
its stakeholders and on new opportunities
that arise because of the development of
new technologies and platforms.
A
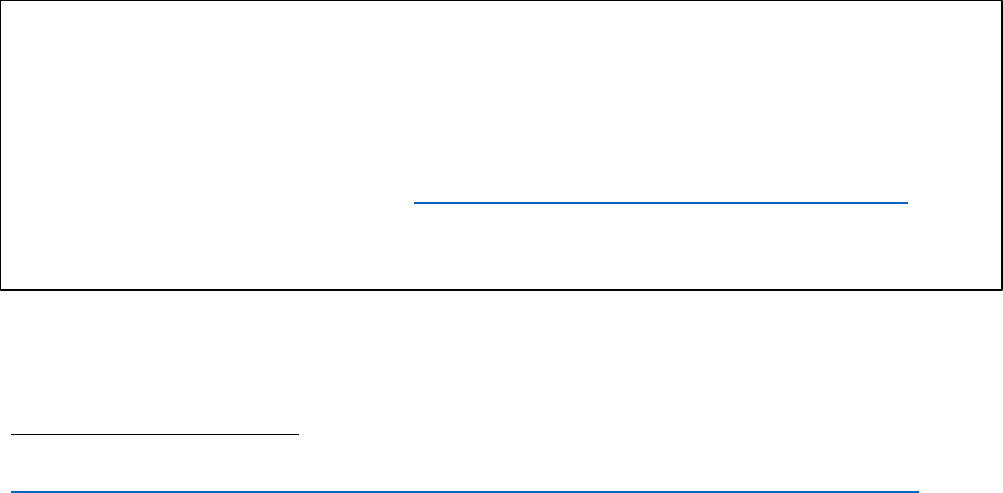
s outlined in the five Overarching Goals and correspondent Strategic Objectives (Fig. 2), NIH’s strategic
approach will move toward a common architecture, infrastructure, and set of tools upon which
individual Institutes and Centers (ICs) and scientific communities will build and tailor for specific needs.
A Software as a Service (SaaS) framework, in which software licensing and delivery are provided and
hosted by centralized resources, will greatly facilitate access to, analysis and curation of, and sharing of
all NIH-funded data. Adhering to NIH’s data-science vision outlined herein, and compatible with the NIH
mission, the NIH Chief Data Strategist, in conjunction with the NIH Scientific Data Council and NIH Data
Science Policy Council, will serve as leads for implementing this strategic plan. Outlines of
Implementation Tactics are presented in this strategic plan as a roadmap for how Overarching Goals and
Strategic Objectives will be achieved. Details of these Implementation Tactics will be determined by the
NIH Chief Data Strategist in collaboration with working groups established by the NIH Scientific Data
Council and NIH Data Science Policy Council, in consultation with the ICs, other federal and international
agencies, the research community, the private sector, and other key stakeholder groups. Evaluation is a
critical component of stewardship of federal resources, and NIH will also develop performance
What is FAIR?
Biomedical research data should adhere to FAIR principles, meaning that
it should be Findable, Accessible, Interoperable, and Reusable.
• To be Findable, data must have unique identifiers, effectively
labeling it within searchable resources.
• To be Accessible, data must be easily retrievable via open systems
and effective and secure authentication and authorization
procedures
.
• To
be Interoperable, data should “use and speak the same
language” via use of standardized vocabularies.
• To be Reusable, data must be adequately described to a new user,
have clear information about data-usage licenses, and have a
traceable “owner’s manual,” or provenance.
Data Infrastructure
•Optimize data
storage and
security
•Connect NIH data
systems
Modernized Data
Ecosystem
•Modernize data
repository
ecosystem
•Support storage
and sharing of
individual datasets
•Better integrate
clinical and
observational data
into biomedical
data science
Data Management,
Analytics, and Tools
•Support useful,
generalizable, and
accessible tools
and workflows
•Broaden utility of
and access to
specialized tools
•Improve discovery
and cataloging
resources
Workforce
Development
•Enhance the NIH
data-science
workforce
•Expand the
national research
workforce
•Engage a broader
community
Stewardship and
Sustainability
•Develop policies
for a FAIR data
ecosystem
•Enhance
stewardship
Figure 2. NIH Strategic Plan for Data Science: Overview of Goals and Objectives

7
measures and specific milestones that will be used to gauge the progress of this strategic plan and guide
any necessary course corrections. Examples of possible qualitative and quantitative metrics and
milestones appear at the end of each Goal section to give a frame of reference and help guide the
community’s thinking about developing optimal evaluation metrics and strategies.
Cross-Cutting Themes
The O
verarching Goals, Strategic Objectives, and Implementation Tactics
outlined in this plan are highly
integrated. The central aim is to modernize the data-resource ecosystem to increase its utility for
researchers and other stakeholders, as well as to optimize its operational efficiency. The many
connections between infrastructure, resources, tools, workforce, and policies call us to articulate a
number of cross-cutting themes, presented below, that layer across the intentions and actions outlined
in this document.
• Su
pport common infrastructure and architecture on which more specialized platforms can be built
and interconnected.
• Leverage commercial tools, technologies, services, and expertise; and adopt and adapt tools and
technologies from other fields for use in biomedical research.
• Enhance the nation’s biomedical data-science research workforce through improved training
programs and novel partnerships.
• Enhance data sharing, access, and interoperability such that NIH-supported data resources are FAIR.
• Ensure the security and confidentiality of patient and participant data in accordance with NIH
requirements and applicable law.
• Improve the ability to capture, curate, validate, store, and analyze clinical data for biomedical
research.
• With community input, develop, promote—and refine as needed—data standards, including
standardized data vocabularies and ontologies, applicable to a broad range of fields.
• Coordinate and collaborate with other federal, private and international funding agencies and
organizations to promote economies of scale and synergies and prevent unnecessary duplication.
Dat
a science holds significant potential for accelerating the pace of biomedical research. To this end,
NIH will continue to leverage its roles as an influential convener and major funding agency to encourage
rapid, open sharing of data and greater harmonization of scientific efforts. Through implementing this
strategic plan, NIH will enhance the scientific community’s ability to address new challenges in
accessing, managing, analyzing, integrating, and making reusable the huge amounts of data being
generated by the biomedical research ecosystem.

8
Overarching Goals, Strategic Objectives, and Implementation Tactics
Ensuring that the biomedical research data-resource ecosystem is FAIR (see text box
) is a laudable but
complex goal to achieve on a large scale, especially given the international expanse of biomedical
research data resources and their use. NIH as the world’s largest funder of biomedical research can play
a leadership role by developing practical and effective policies and principles related to the storage, use,
and security of biomedical data. In this strategic plan, NIH articulates specific priorities that address
developing reliable, accessible, and appropriately secured modes of storage; transforming a fragmented
set of individual components into a coordinated, efficient, and optimally useful ecosystem; reducing
unnecessary redundancies and increasing synergies and economies of scale; and strengthening
coordination and interactions—both within NIH and between NIH and its stakeholder communities.
Paramount is the need to establish organizing principles and policies for an efficient yet nimble funding
model for data science infrastructure that serves the needs of NIH and its stakeholders.
GOAL 1
Support a Highly Efficient and Effective Biomedical Research Data Infrastructure
NIH ICs routinely support intramural and extramural research projects that generate tremendous
amounts of biomedical data. Regardless of format, all types of data require hardware, architecture, and
platforms to capture, organize, store, allow access to, and perform computations. As projects mature,
data have traditionally been stored and made available to the broader community via public repositories
or at data generators’ or data aggregators’ local institutions. This model has become strained as the
number of data-intensive projects—and the amount of data generated for each project—continues to
grow rapidly.
Objective 1-1 | Optimize Data Storage and Security
Large-scale cloud-computing platforms are shared environments for data storage, access, and
computing. They rely on using distributed data-storage resources for accessibility and economy of
scale—similar conceptually to storage and distribution of utilities like electricity and water. Cloud
environments thus have the potential to streamline NIH data use by allowing rapid and seamless access,
as well as to improve efficiencies by minimizing infrastructure and maintenance costs. NIH will leverage
what is available in the private sector, either through strategic partnerships or procurement, to create a
workable Platform as a Service (PaaS) environment. Using unique approaches enabled by the
21
st
-
Century Cures Act (such as “Other Transactions Authority”), NIH will partner with cloud-service
providers for cloud storage, computational, and related infrastructure services needed to facilitate the
deposit, storage, and access to large, high-value NIH datasets (see text box “Science in the Cloud: The

9
NIH Data Commons”). NIH will evaluate which of these approaches are useful as we enter the
implementation phase of this strategic plan.
These negotiations may result in partnership agreements with top infrastructure providers from U.S.-
based companies whose focus includes support for research. Suitable cloud environments will house
diverse data types and high-value datasets created with public funds. NIH will ensure that they are
stable and adhere to stringent security requirements and applicable law, to protect against data
compromise or loss. NIH will also comply with the
Health Insurance Portability and Accountability Act of
1996 (HIPAA) Security Rule and National Institute of Standards and Technology (NIST) health-
information security standards. NIH’s cloud-marketplace initiative will be the first step in a phased
operational framework that establishes a SaaS paradigm for NIH and its stakeholders.
Implementation Tactics:
• Leverage existing federal, academic, and commercial computer systems for data storage and
analysis.
• Adopt and adapt emerging and specialized technologies (see text box “Graphical Processing Units”).
• Support technical and infrastructure needs for data security, authorization of use, and unique
identifiers to index and locate data.
Objective 1-2 | Connect NIH Data Systems
Science in the Cloud: The NIH Data Commons
One of the first steps NIH is taking to modernize the biomedical research data ecosystem is funding the NIH Data
Commons pilot: Its main objective is to develop the ability to make data FAIR through use of a shared virtual space
to store and work with biomedical research data and analytical tools. The NIH Data Commons will leverage
currently available cloud-computing environments in a flexible and scalable way, aiming to increase the value of
NIH-supported data by democratizing access and use of data and analytical tools and allowing multiple datasets to
be queried together. To begin, the NIH Data Commons will enable researchers to work with three test datasets: the
National Heart, Lung, and Blood Institute’s Trans-Omics for Precision Medicine (TOPMed) program, the NIH
Common Fund’s Genotype-Tissue Expression (GTEx) program, and various model-organism data repositories.

10
More than 3,000 different groups and individuals submit data
via NCBI systems daily. Among these are genome sequences
from humans and research organisms; gene-expression data;
chemical structures and properties, including safety and toxicity
data; information about clinical trials and their results; data on
genotype-phenotype correlations; and others. Beyond NIH-
funded scientists and research centers, many other individuals
and groups contribute data to the biomedical research data
ecosystem, including other federal agencies, publishers, state
public-health laboratories, genetic-testing laboratories, and
biotech and pharmaceutical companies. NIH will develop
strategies to link high-value NIH data systems, building a
framework to ensure they can be used together rather than
existing as isolated data silos (see text box, below, “Biomedical Data Translator”). A key goal is to
promote expanded data sharing to benefit not only biomedical researchers but also policymakers,
funding agencies, professional organizations, and the public.
Implementation Tactics:
• Link the NIH Data Commons (see text box, above) and existing, widely-used NIH databases/data
repositories using NCBI as a coordinating hub.
• Ensure that new NIH data resources are connected to other NIH systems upon implementation.
• When appropriate, develop connections to non-NIH data resources.
Graphical Processing Units
The workhorses of most computers are
central-processing units, or CPUs, which
perform computing functions as specified by
computer programs. Specialized versions of
these, called graphical processing units, or
GPUs, are dedicated exclusively to imagery, or
graphics. These elements have driven the
motion-picture and video-game industries,
and, more recently, have been adapted for
use in biomedical research with very large and
complex datasets such as molecular, cellular,
radiological, or clinical images.
Biomedical Data Translator
Through its Biomedical Data Translator program, the National Center for Advancing Translational Sciences
(NCATS) is supporting research to develop ways to connect conventionally separated data types to one
another to make them more useful for researchers and the public. The Translator aims to bring data types
together in ways that will integrate multiple types of existing data sources, including objective signs and
symptoms of disease, drug effects, and other types of biological data relevant to understanding the
development of disease and how it progresses in patients.
Goal 1: Evaluation
For this Goal,
potential measures of progress include, but are not limited to: quantity and user experiences of cloud
storage and computing used by NIH and by NIH-funded researchers; unit costs for cloud storage and
computing; number of technologies adapted for use by NIH-funded resources; quantity and ease-of use
of NIH data resources incorporated into the NIH Data Commons; and quantity of NIH data resources
linked together. NIH will also develop a data-security plan by evaluating lessons learned and best
practices adopted from other programs (i.e., All of Us, Cancer Data Commons, and others) and include
relevant standards in the plan. NIH will also conduct security-control assessments using NIH’s standard
“Su
pport a Highly Efficient and Effective Biomedical Research Data Infrastructure,”

12
GOAL 2
Promote Modernization of the Data-Resources Ecosystem
The current biomedical data-resource ecosystem is challenged by a number of organizational problems
that create significant inefficiencies for researchers, their institutions, funders, and the public. For
example, from 2007 to 2016, NIH ICs used dozens of different funding strategies to support data
resources, most of them linked to research-grant mechanisms that prioritized innovation and hypothesis
testing over user service, utility, access, or efficiency. In addition, although the need for open and
efficient data sharing is clear, where to store and access datasets generated by individual laboratories—
and how to make them compliant with FAIR principles—is not yet straightforward. Overall, it is critical
that the data-resource ecosystem become seamlessly integrated such that different data types and
information about different organisms or diseases can be used easily together rather than existing in
separate data “silos” with only local utility. Wherever possible, NIH will coordinate and collaborate with
other federal, private, and international funding agencies and organizations to promote economies of
scale and synergies and prevent unnecessary duplication.
Objective 2-1 | Modernize the Data Repository Ecosystem
To promote modernization of the data-repository ecosystem, NIH will refocus its funding priorities on
the utility, user service, accessibility, and efficiency of operation of repositories (see Current Data
Science Challenges for NIH). Wherever possible, data repositories should be integrated and contain
harmonized data for all related organisms, systems, or conditions, allowing for seamless comparison. To
improve evaluation of data-repository utility, and allow those who run them to focus on the particular
goals they need to achieve to best support the research community and operate as efficiently as
possible, NIH will distinguish between databases and knowledgebases (see text box “Databases and
Knowledgebases: What’s the Difference?”) and will support each separately from one another as well as
from the development and dissemination of tools used to analyze data (see
Goal 3 for NIH’s proposed
new strategies for tool development). Although a grey area does exist between databases and
Databases and Knowledgebases: What’s the Difference?
Databases are data repositories that store, organize, validate, and make accessible the core data related to a
particular system or systems. For example, core data might include genome, transcriptome, and protein
sequences for one or more organism. An example of a clinically-oriented database would be one linking
radiological images to patient genotypes. Databases typically require less human curation than do
knowledgebases, and curation for databases generally focuses on quality assurance/quality control (QA/QC)
rather than data interpretation or increasing information content.
Knowledgebases accumulate, organize, and link growing bodies of information related to core datasets.
Knowledgebases typically require significant human curation beyond the QA/QC and annotation needed for
databases. A knowledgebase may contain, for example, information about gene-expression patterns, splicing
variants, localization, and protein-protein interactions and pathway networks related to an organism or set of
organisms. A clinically-oriented knowledgebase could contain the up-to-date information on associations
between gene variants or radiological images and responses to therapeutics or other medical interventions.
Knowledgebases frequently contain information gleaned from the scientific literature through human curation.

13
knowledgebases, and some data types currently appropriate for a knowledgebase may eventually
harden and become core data more appropriate for a database, this distinction will allow improved
focus and coherence in the support and operation of modern data resources. It should be noted that the
same NIH-funded group could be supported to perform multiple functions—for example, to run a
knowledgebase (or database) and also to develop tools to be used on the information in that
knowledgebase or database—but these proposed activities should be evaluated and funded separately
to ensure that each is providing the best possible value and service to the research community and that
the existence of essential resources is not tied to functions that may not be as useful. Funding
approaches used for databases and knowledgebases will be appropriate for resources and focus on user
service, utility, interoperability, and operational efficiency rather than on research-project goals. As
such, NIH will establish procedures and metrics to monitor data usage and impact—including usage
patterns within individual datasets. The above principles and approaches are well aligned with those
being implemented by the European inter-governmental data-resource coordinating organization
ELIXIR
.
Implementation Tactics:
• Separate the support of databases and knowledgebases (see text box
, above).
• Use appropriate and separate funding strategies, review criteria, and management for each
repository type.
• Dynamically measure data use, utility, and modification.
• Ensure privacy and security.
• Create unified, efficient, and secure authorization of access to sensitive data.
• Employ explicit evaluation, lifecycle, sustainability, and sunsetting expectations (where appropriate)
for data resources.
Objective 2-2 | Support the Storage and Sharing of Individual Datasets
Currently, most datasets generated by biomedical researchers are small-scale datasets produced by
individual laboratories. In contrast, large, organized consortia, including various programs specific to NIH
ICs and the NIH Common Fund, generate large, high-value datasets that are relatively small in numbers
but used by thousands of researchers. Whereas these large datasets generally reside in dedicated data
resources, a current dilemma for NIH is determining how to store and make accessible all of the smaller
datasets from individual laboratories. NIH will create an environment in which individual laboratories
can link datasets, through intuitive and user-friendly interfaces, to publications in the NCBI’s PubMed
Central publication database. Part of that effort includes development of the NIH Data Commons Pilot,
the first trans-NIH effort to create a shared, cloud-based environment for data storage, access, and
computation.
Implementation Tactics:

14
• Link datasets to publications via PubMed Central and NCBI.
• Longer-term: Expand NIH Data Commons to allow submission, open sharing, and indexing of
individual, FAIR datasets.
Objective 2-3 | Leverage Ongoing Initiatives to Better Integrate Clinical and Observational Data
into Biomedical Data Science
NIH has several large-scale, ongoing efforts that are building high-value resources that include clinical
and observational data from individual volunteers and
patients (for one example, see text box, “TB Portals”). These
efforts also include the All of Us Research Program and
Cancer Moonshot
SM
, the National Heart, Lung and Blood
Institute’s Trans-Omics for Precision Medicine (TOPMed)
program, the Environmental Influences on Child Health
Outcomes (ECHO) program, and various datasets generated
by scientists conducting research in the NIH Clinical Center
(see text box, below, “Big Data for Health”). Other federal
datasets are likely to be invaluable for research discovery,
such as the Million Veteran Program and other data from the
Veteran’s Health Administration, the nation’s largest
integrated health system. NIH will leverage these and other related initiatives to integrate the patient
health data they contain into the biomedical data-science ecosystem in ways that maintain security and
confidentiality and are consistent
with informed consent, applicable
laws, and high standards for ethical
conduct of research (see
Clinical
Data and Information Security).
NIH will collaborate with the Office
of the National Coordinator for
Health Information Technology
(ONC), within the Department of
Health and Human Services, which
leads national health information
technology efforts (see text box,
below).
The NIH Clinical Center has in place
the Biomedical Translational
Research Information System
(BTRIS), which is a resource
Big Data for Health
Two signature NIH projects that aim to garner health insights from
human data are the All of Us Research Program and the Cancer
Moonshot. The All of Us Research Program aims to gather data over
time from 1 million or more people living in the United States, with
the ultimate goal of accelerating research and improving health.
Scientists plan to use All of Us Research Program data to learn more
about how individual differences in lifestyle, environment, and
biological makeup can influence health and disease. Participants in
the All of Us Research Program may be invited to use wearable
sensors that will provide real-time measurements of their health and
environmental exposures, significantly expanding this type of
research. The Cancer Moonshot aims to accelerate cancer research
to make more therapies available to more patients, while also
improving our ability to prevent cancer and detect it at an early
stage. Data-intensive strategies include mining past patient data to
predict responses to standard treatments and future patient
outcomes, developing a three-dimensional cancer atlas to view how
human tumors change over time, and a Cancer Research Data
Commons.
TB Portals
The National Institute of Allergy and Infectious
Diseases Tuberculosis (TB) Portals Program is a
multi-national collaboration for data sharing and
analysis to advance TB research. A consortium of
clinicians and scientists from countries with a heavy
burden of TB, especially drug-resistant TB, work
together with data scientists and information
technology professionals to collect multi-domain TB
data and make it available to clinical and research
communities.

15
available to the NIH intramural community that brings together clinical research data from the Clinical
Center and other NIH ICs. BTRIS provides clinical investigators and translational informaticists with
access to identifiable data for subjects on their own active protocols, while providing all NIH
investigators with access to data without personal identifiers across all protocols. Additionally, NIH
encourages researchers to use common data elements, or CDEs, which helps improve accuracy,
consistency, and interoperability among data sets within various areas of health and disease research.
The Office of the National Coordinator for Health Information Technology (ONC)
ONC reports directly to the Secretary of HHS. It is the principal federal entity responsible for the coordination and
implementation of nationwide efforts for the electronic exchange of health information. ONC’s mission is to improve
the health and well-being of individuals and communities through the use of technology and health information that
is accessible when and where it matters most. As part of this mission, ONC coordinates nationwide efforts to
implement and use the most advanced health information technology standards to promote the electronic exchange
of health information. ONC works closely with its federal partners to promote the exchange of data between federal
health agencies and the private sector. ONC’s federal partners include NIH, FDA, CDC, the Office for Civil Rights (OCR),
and CMS. ONC’s interoperability initiatives help make electronic health records more accessible for research, and NIH
continues to adopt these practices such as standardizing terminology, or vocabularies, for clinical care.
Implementation Tactics:
• Create efficient linkages among NIH data resources that contain clinical and observational
information.
• Develop and implement universal credentialing protocols and user-authorization systems to enforce
a broad range of access and patient-consent policies across NIH data resources and platforms.
• Promote use of the NIH Common Data Elements Repository.
Goal 2: Evaluation
For this Goal, “Promote Modernization of the Data-Resources Ecosystem
,” potential measures of
progress include, but are not limited to: data-resource use metrics (overall and individual datasets);
quantity and interoperability of databases and knowledgebases supported using resource-based funding
mechanisms; cost-efficiency improvements over baseline (e.g., cost per unit of use by researchers, cost
per amount of data stored, average cost per resource) of NIH-supported data resources; quantity and
use of datasets deposited (over baseline) and linked to publications in PubMed Central; linkages
between NIH clinical and observational data resources; adoption of new methods and technologies to
improve security and confidentiality of patient data; and usage of the NIH Common Data Elements
Repository/adherence to data standards.

16
GOAL 3
Support the Development and Dissemination of Advanced Data Management, Analytics, and
Visualization Tools
Extracting understanding from large-scale or complex biomedical research data requires algorithms,
software, models, statistics, visualization tools, and other advanced approaches such as machine
learning, deep learning, and artificial intelligence (see text box “Thinking Machines
7
”). Accomplishing
NIH’s goal of optimizing the biomedical data-science
ecosystem requires prioritizing development and
dissemination of accessible and efficient methods for
advanced data management, analysis, and
visualization. To make the best tools available to the
research community, NIH will leverage existing,
vibrant tool-sharing systems to help establish a more
competitive “marketplace” for tool developers and
providers than currently exists, striving for wide
availability and limited or no costs for users. By
separating the evaluation and funding for tool
development and dissemination from support for
databases and knowledgebases, innovative new
tools and methods should rapidly overtake and
supplant older, obsolete ones. The goal of creating a
more competitive marketplace, in which open-source programs, workflows, and other applications can
be provided directly to users, could also allow direct linkages to key data resources for real-time data
analysis.
Objective 3-1 | Support Useful, Generalizable, and Accessible Tools and Workflows
Historically, because data resources have generally been funded through NIH research grants, applicants
have emphasized development of new tools in order to meet innovation expectations associated with
conducting research. This strategy can shift the focus of data resources away from their core function of
providing reliable and efficient access to high-quality data. In addition, coupling review and funding of
data resources to tool development can inhibit the type of open competition among developers that
allows support of the most innovative and useful tools (see Current Data Science Challenges for NIH
). To
address these concerns, NIH will evaluate and fund tool development and access separately from
support of databases and knowledgebases, although tools that are necessary for data intake,
integration, management, access, or QA/QC could still be incorporated into database and
knowledgebase funding. NIH will also promote the establishment of environments in which high-quality,
open-source data management, analytics, and visualization tools can be obtained and used directly with
7
Dreyer KJ, Geis JR. When Machines Think: Radiology's Next Frontier. Radiology. 2017 Dec;285(3):713-718. doi:
10.1148/radiol.2017171183.
Thinking Machines
Artificial intelligence, machine learning, and deep
learning are computer algorithms that change as
they are exposed to more data. Many are adept at
recognizing objects in images, thus enabling
machines to find patterns in data in ways that are
not only cost-effective but also potentially beyond
human abilities. “Centaur radiologists,” hybrids of
human and computer expertise, will likely offer the
opportunity to interpret data from a range of
sources, including electronic health records. Such
hybrid person-machine interpretations will likely
have a formative role in customizing care to
individual patients.

17
data in the NIH Data Commons and/or other cloud environments. A key step will be leveraging through
partnerships, grants, or procurement expertise in systems integration/engineering to refine and harden
tools from academia to improve software design, usability, performance, security, and efficiency. The
use of Small Business Innovation Research or Small Business Technology Transfer (SBIR/STTR) grants
might provide a useful mechanism for bringing into the biomedical data science ecosystem expertise
from systems integrators and software engineers.
Implementation Tactics:
• Separate support for tool development from support for databases and knowledgebases.
• Use appropriate funding mechanisms, scientific review, and management for tool development.
• Establish programs to allow systems integrators/engineers from the private sector to refine and
optimize prototype tools and algorithms developed in academia to make them efficient, cost-
effective, and widely useful for biomedical research.
• Employ a range of incentives to promote data-science and tool innovation including “code-athons,”
challenges, public-private partnerships, and other approaches.
Objective 3-2 | Broaden Utility, Usability, and Accessibility of Specialized Tools
An important opportunity and challenge is to adopt for use in biomedical research tools that have been
developed by fields outside of the biomedical sciences. For example, the same software used by NASA
scientists to determine the depths of lakes from space is being tested for use in medical-image analysis
for mammography, X Rays, computerized tomography (CT) and magnetic resonance imaging (MRI)
scans, as well as for ultrasound measurements.
8
Specialized tools developed for one subfield of
biomedical research might also be adopted for different purposes by researchers in other areas.
It will also be important to develop and adopt better tools, and standards, for collecting and efficiently
assimilating data from disparate and dynamic sources that combine to inform us about the health of
individuals and populations. Novel data-science algorithms will likely create new knowledge and
innovative solutions relevant to health disparities and disease prevention. New approaches and tools
have the potential to transform data combined from various structured and unstructured sources into
actionable information that can be used to identify needs, provide services, and predict and prevent
poor outcomes in vulnerable populations. Metadata, which is information about data such as its
content, context, location, and format, affects the ability of data to be found and used/re-used, and thus
will be important in these efforts. Data provenance, or “version control” of data is also an important
consideration for both data generators and data users. Toward identifying and stratifying risk,
employing standardized data formats and vocabularies should advance our understanding of
8
NASA Technology Transfer Program: Hierarchical Image Segmentation: Available at
https://technology.nasa.gov//t2media/tops/pdf/GSC-TOPS-14.pdf

18
relationships between demographic information, social determinants of health, and health outcomes.
One especially ripe opportunity for use in community-based research is broader use of rapidly evolving
mobile-device technologies and information-sharing platforms. These resources, such as wearable
devices, can capture a wide variety of health and lifestyle-related information including geospatial and
biometric data and patient-reported outcomes from individual volunteers that could help transform our
understanding of both normal human biology and disease states.
Finally, there is a critical need for better methods to mine the wealth of data available in electronic
health records (see text box “Linking Genomic Data to Health: eMERGE”). These records present great
opportunities for advancing medical research and improving human health—particularly in the area of
precision medicine—but they also pose tremendous challenges (see
“Clinical Data and Information
Security”). For example, patient confidentiality must be assured, and the level of access granted by each
individual to researchers has to be
obtained, recorded, obeyed, and
enforced, in accordance with HIPAA and
NIST standards. Equally challenging is
the fact that electronic health records
are controlled by thousands of different
hospitals and other organizations using
dozens of different commercial
computer platforms that do not always
share a uniform language or data
standards. Because of these challenges,
NIH will support additional research to
find better ways to allow clinical data to be used securely, ethically, and legally, to advance medicine.
NIH will also work with other federal and state agencies, private healthcare and insurance providers, and
patient advocacy groups to find more efficient paths to realize the promise of electronic health records
and other clinical data for medical research.
Linking Genomic Data to Health: eMERGE
eMERGE is an NIH-funded national network organized and
funded by the National Human Genome Research Institute that
combines DNA biorepositories with electronic health record
systems for large scale, high-throughput genetic research in
support of implementing genomic medicine. Begun in 2007, the
project merges genetic data from patients with their electronic
health records and facilitates sharing of the data for biomedical
research. eMERGE currently involves 14 sites across the country
that collect, store, and share patient data for biomedical
discovery aiming to improve patient care.
Implementation Tactics:
• Adopt and adapt emerging and specialized methods, algorithms, tools, software, and workflows.
• Promote innovative contributions to biomedical data science from allied fields such as mathematics,
statistics, computer science, engineering, and physics (see text box, “NSF/NIGMS Mathematical
Biology Program,” below).
• Promote development and adoption of better mobile-device and data-interface tools through APIs
that integrate with certified health information technology to pull data and support data analysis.
• Support research to develop improved methods for clinical informaticists and other scientists to use
certified electronic health records
and other clinical data securely and ethically for medical research.

19
Objective 3-3 | Improve Discovery and Cataloging Resources
Data that is not easily located is likely to be underused and of little value to the broader research
community. NIH has invested in developing resources, such as the Data Discovery Index that is part of
the NIH Data Commons pilot, to enable data
reuse. Such a resource will exceed a mere
cataloging function and will also contain
platforms and tools by which biomedical
researchers can find and reuse data and that
will support data-citation metrics. NIH will
continue to invest in development of improved
approaches for making data findable and
accessible. For example, the NIH Data
Commons pilot is creating search and analysis
workspaces that support a broad range of
authenticated users, and where users with all
levels of expertise can access and interact with
data and tools. Collaboration will be integral to this approach, which, in addition to continued research
and development, must involve a community-driven process for identifying and implementing optimal
standards to improve indexing, understandability, reuse, and citation of datasets. NIH will also leverage
the U.S. Data Core for Interoperability effort, which addresses data standards and data provenance as
part of its aim to enhance interoperability of health information data.
NSF/NIGMS Mathematical Biology Program
Since 2007, The National Institute of General Medical Sciences
(NIGMS) and NSF have collaborated to support research in
mathematics and statistics on questions in the biological and
biomedical sciences. Both agencies recognize the need for
promoting research at the interface between the mathematical
sciences and the life sciences. This program is designed to
encourage new collaborations, as well as to support existing
ones. Topics under study vary widely and include, for example,
morphogenesis during development, infectious-disease
modeling, cell mechanics and signaling, and biomechanics
modeling.
Implementation Tactics:
• Promote community development and adoption of uniform standards for data indexing, citation,
and modification-tracking (data provenance).
Goal 3: Evaluation
For this Goal, “
Support the Development and Dissemination of Advanced Data Management, Analytics,
and Visualization Tools,” potential measures of progress include, but are not limited to: quantity and
ease-of-use of new software tools developed; citations of tool use; downloads of tools from tool
repositories; and quantity of tools adapted from other fields for use in biomedical research.

20
GOAL 4
Enhance Workforce Development for Biomedical Data Science
NIH also considers it essential to equip the biomedical research workforce with tools to enhance data-
science understanding and expertise. Innovative contributions to biology from computer science,
mathematics, statistics, and other quantitative fields have facilitated the shift in biomedicine described
throughout this document. NSF has been at the forefront of funding disciplines that contribute to data
science, and thus NIH will collaborate on joint initiatives of mutual interest related to training and
education of researchers at various career stages. NIH recognizes that data scientists perform far more
than a support function, as data science has evolved to be an investigative domain in its own right.
While NIH has supported quantitative training at various levels along the biomedical career path, more
needs to be done to facilitate familiarity and expertise with data-science approaches and effective and
secure use of various types of biomedical research data. There is also a need to grow and diversify the
pipeline of researchers developing new tools and analytic methods for broad use by the biomedical
research community. Finally, data-science approaches will be essential for NIH to achieve the
stewardship goals outlined in the NIH-wide strategic plan and are likely to facilitate the agency’s ability
to monitor demographic trends among its workforce and thus address diversity gaps (see text box,
below, “Data Science and Diversity”).
Objective 4-1 | Enhance the NIH Data-Science Workforce
Given the importance of data science for biomedical research, NIH needs an internal workforce that is
increasingly skilled in this area. This includes ensuring that NIH program and review staff who administer
and manage grants and coordinate the
evaluation of applications have sufficient
experience with and knowledge of data
science. To begin to address this need,
NIH will develop training programs for its
staff to improve their knowledge and
skills in areas related to data science. In
addition, NIH will recruit a cohort of data
scientists and others with expertise in
areas such as project management,
systems engineering, and computer
science from the private sector and academia for short-term (1- to 3-year) national service sabbaticals.
These “NIH Data Fellows” will be embedded within a range of high-profile, transformative NIH projects
such as All of Us, the Cancer Moonshot
SM
and the BRAIN initiative and will serve to provide innovation
and expertise not readily available within the federal government.
Data Science and Diversity
Data-driven approaches offer opportunities to address gaps in
scientific workforce diversity, by observing and influencing
system-wide patterns. NIH has applied this strategy to
understand factors driving recruitment and retention of
undergraduate students from underrepresented groups as well
as to study various approaches to mentoring. Additional
systems-based approaches to workforce modeling, including at
the faculty level at NIH-funded institutions, offer promise for
understanding effects on diversity in various contexts.
Implementation Tactics:
21
• Develop data-science training programs for NIH staff.
• Launch the NIH Data Fellows program.
Objective 4-2 | Expand the National Research Workforce
Modern biomedical research is becoming increasingly quantitative and it is essential that the next
generation of researchers be equipped with the skills needed to take advantage of the growing promise
of data science for advancing human health. NIH will work to ensure that NIH-funded training and
fellowship programs emphasize teaching of quantitative and computational skills and integrate training
in data-science approaches throughout their curricula and during mentored research. In keeping with
the National Library of Medicine’s (NLM) strategic plan, “A Platform for Biomedical Discovery and Data-
powered Health,”
9
NIH will partner with institutions to engage librarians and information specialists in
finding new paths in areas such as library science that have the potential to enrich the data-science
ecosystem for biomedical research.
The NLM Institutional Training Grants for Research Training in
Biomedical Informatics and Data Science (T15) program offers one funding vehicle.
Implementation Tactics:
• Enhance quantitative and computational training for undergraduates, graduate students, and
postdoctoral fellows.
• Enable the development of curricula and other resources toward enhancing rigor and reproducibility
of data science-based approaches.
• Promote training of data scientists in biomedical research areas.
• Improve the education of students on NIH training grants by enriching content in Responsible
Conduct of Research requirements with information about secure and ethical data use.
• Build on diversity-enhancing efforts in data science, such as the NIH BD2K Diversity Initiative.
10
• Engage librarians and information specialists in developing data-science solutions and programs.
• Employ data-driven methods to monitor workforce diversity.
Objective 4-3 | Engage a Broader Community
As a field, data science crosses boundaries between research and practice, as well as between science
and policy. NIH will promote knowledge exchange and development of best practices for the collection,
organization, preservation, and dissemination of information resources across communities. Part of this
effort is nurturing cultural change, emphasizing the role of data science in discovery and health, and
9
A Platform for Biomedical Discovery and Data-Powered Health: The National Library of Medicine Strategic Plan
2017–2027. Available at: https://www.nlm.nih.gov/pubs/plan/lrp17/NLM_StrategicReport2017_2027.html
.
10
Canner JE, McEligot AJ, Pérez ME, Qian L, Zhang X. Enhancing Diversity in Biomedical Data Science. Ethn Dis.
2017;27(2):107-116.
22
enabling citizen scientists access to data without compromising its privacy or security. NIH recognizes its
role in the larger data-science ecosystem and that NIH-generated biomedical data are used often by the
private sector, clinicians, and other public groups. As part of the BD2K effort, NIH encouraged
development of new or significantly adapted interactive digital media that engages the public, experts
or non-experts, in performing some aspect of biomedical research via crowdsourcing. NIH will work to
find additional ways to engage the public and healthcare providers in making use of biomedical data and
data-science tools. Doing so will help to expand the biomedical “sandbox” to researchers without access
to large-scale computational resources, such as non-research academic organizations, community
colleges, and citizen scientists. NIH will also consider new engagement models for enhancing data
security such as “bug bounty programs,” in which individuals can receive recognition and compensation
for reporting bugs, especially those pertaining to data exploits and vulnerabilities. Such programs have
been successful in the federal government—one example is “Hack the Pentagon,”
11
which enabled the
discovery of critical vulnerabilities within minutes. Such efforts require close collaboration with federal
partners such as the Departments of Justice, the National Institute of Standards and Technology, and
Homeland Security, as well as with private industry.
11
Carter Announces 'Hack the Pentagon' Program Results. Department of Defense news article. Available at:
Implementation Tactics:
• Give citizen scientists access to appropriate data, tools, and educational resources (see text box
“Citizen Science”).
• Find innovative solutions to data-science and data-resource challenges using community-
engagement models such as code-athons, contests, and crowdsourcing.
• Develop materials to train healthcare providers in data science-related clinical applications.
h
ttps://www.defense.gov/News/Article/Article/802828/carter-announces-hack-the-pentagon-program-results/
Citizen Science
Citizen science aims to bring science and science policy processes to the public, to ensure that science is responsive to
public concerns and needs and to harness an additional resource to capture data and innovation in a wide variety of
fields. One example is EyeWire, an online resource launched in 2012 that challenges players to map the three-
dimensional structure of neurons in the retina of a mouse using real electron-microscopy images. About 70,000 players
from more than 130 countries play this scientific “game,” which is helping researchers discover how neurons connect
to process visual information. NIH also funds the Experiential Citizen Science Training for The Next Generation
program
that promotes biomedical scientific careers among K-12 students and aims to increase participation of individuals and
groups underrepresented in the biomedical sciences.
Goal 4: Evaluation

23
For this Goal, “Enhance Workforce Development for Biomedical Data Science,” potential measures of
progress include, but are not limited to: quantity of new data science-related training programs for NIH
staff, participation in and outcomes from these programs; number of NIH Data Fellows recruited;
number of NIH-funded training programs that increase requirements for quantitative and computational
skills development; short- and long-term programmatic outcomes measures such as trainee-reported
self-efficacy in quantitative and computational skills, degree attainment, and post-training employment;
and demographic, geographic, and disciplinary diversity of NIH-funded quantitative scientists.

24
GOAL 5
Enact Appropriate Policies to Promote Stewardship and Sustainability
Creating and maintaining an efficient and effective biomedical data-science ecosystem requires policies
and practices appropriate for optimal governance, financial management, evaluation, and sustainable
stewardship of resources. Because cultural issues are central to implementing policies, appropriate
reward, review, and expectation systems are central to making data FAIR and for incentivizing
researchers to share their data and analysis tools widely for reuse by others. To ensure researchers
collecting data understand and comply with data-security and confidentiality standards and applicable
law, it will be important for NIH to collaborate with the research community on strategies to guide
general practice in data security and privacy matters and to collaborate with industry leaders who set
standards in the information-security arena.
Objective 5-1 | Develop Policies for a FAIR Data Ecosystem
Currently, most biomedical data do not adhere to FAIR principles and thus are difficult to find and
access. Moreover, complex or integrated analysis requires that data are interoperable and reusable
across multiple domains with high fidelity. Thus, through appropriate policies and practices and as a
core data-management activity, NIH will strive to ensure that all data in NIH-supported data resources
are FAIR. The NIH Data Commons Pilot will be a starting point toward accomplishing this objective.
While freely sharing high-value data is a critical goal for advancing research, NIH must ensure that its
policies are achievable and sustainable and do not impose unnecessary burdens or untenable
expectations on grantee institutions. Therefore, policies must reflect the data use and evaluation
metrics and methods that will be established in Objective 2-1
to guide what data need to be made
accessible and when they should be moved to less-accessible but less-expensive archive storage or
retired altogether. NIH will also promote community-guided development of model open data-use
licenses that will facilitate data sharing while simultaneously allowing protection of confidentiality and
intellectual property. In addition, the NIH Data Commons pilot is establishing ways to use controlled-
access data through appropriate authentication and protocols.
Implementation Tactics:
• Create rational and supportable data-sharing and data-management policies that ensure the
security and confidentiality of patient and participant data and comply with applicable law.
• Promote development of community standards that support FAIR principles for data storage.
• Develop model open-data use licenses to enable broad access to datasets.
• Optimize security management and access policies.
• Ensure appropriate standards and mechanisms are in place to grant trusted-partner status for
efficient data-access management.

25
Objective 5-2 | Enhance Stewardship
The rapidly growing amount of data generated by the biomedical research enterprise creates an urgent
need for developing clear guidelines for what data must be stored and shared, where and in what form
it must be stored, as well as practical solutions for sustaining valuable data resources and determining
priorities for data-resource funding. In addition, to produce the most scientific value for taxpayers’
investments and to provide researchers with the best access to data resources possible, NIH must work
with the community to improve the efficiency of operation of these resources and, wherever possible,
create synergies and economies of scale. Toward achieving these goals, NIH will collaborate with its
stakeholders—including academia, other U.S. and international funding agencies, journals, and the
private sector—to establish a wide range of metrics to dynamically measure data use, utility, and
modification, as well as measures of the operational efficiency of the resources themselves. Creating
incentives and expectations for depositing FAIR-compliant data in NIH-funded repositories, data
commons, or other NIH data systems, will enhance data sharing and reuse and allow NIH to accurately
assess data usage and lifecycles. This information will be essential for making informed decisions about
priorities for data-resource support. In addition, NIH will engage the broader data-science community in
testing the utility of the NIH Data Commons as it is developed. As it refines these systems, NIH will seek
input from entities with expertise in research ethics, privacy regulations and statutes, and data security
to ensure NIH-supported data resources maintain research-participant confidentiality.
Implementation Tactics:
• Develop standard use, utility, and efficiency metrics and review expectations for data resources and
tools.
• Establish sustainability models for data resources.
• Develop a reward and expectation system for investigators to make data FAIR and for ensuring
open-source data-analysis tools are available.
Goal 5: Evaluation
For this Goal, “Enact Appropriate Policies to Promote Stewardship and Sustainability
,” potential
measures of progress include, but are not limited to: establishment and use of open-data licenses;
development and performance of metrics to assess data-resource use, utility and efficiency of
operation; and usage of data-security protection guidelines by NIH-funded researchers using clinical
data.
26
Conclusion
Accessible, well-organized, secure, and efficiently operated data resources are critical enablers of
modern scientific inquiry. With publication of the NIH Strategic Plan for Data Science, NIH aims to
maximize the value of data generated through NIH-funded efforts to enable biomedical discovery and
innovation. Doing so is critical for keeping the United States at the forefront of biomedical research,
ensuring continued advances toward improving the nation’s health.
This strategic plan is highly interconnected but rests upon five pillars, its Overarching Goals:
• Support a Highly Efficient and Effective Biomedical Research Data Infrastructure
• Promote Modernization of the Data-Resources Ecosystem
• Support the Development and Dissemination of Advanced Data Management, Analytics, and
Visualization Tools
• Enhance Workforce Development for Biomedical Data Science
• Enact Appropriate Policies to Promote Stewardship and Sustainability
As articulated in this plan, NIH considers essential the need to coordinate and collaborate with other
federal, private, and international agencies and organizations in the data-resource ecosystem to
promote economies of scale and synergies and prevent unnecessary duplication. NIH’s goal is to
maximize the utility of the data-resource ecosystem for researchers and to ensure optimal scientific
return on investment for taxpayers. A central facet of the plan is engagement of industry partners who
have expertise in key areas related to information technology, complementing the research strengths of
NIH and the academic community, and helping ensure that we achieve the plan’s Overarching Goals and
Strategic Objectives in an efficient manner. As outlined above, NIH’s vision is to move toward a common
framework upon which individual ICs and scientific fields will build and adapt. The inaugural NIH Chief
Data Strategist, in conjunction with the NIH Scientific Data Council and NIH Data Science Policy Council,
will lead efforts to manage this new system and will take the lead on implementing this strategic plan, in
close collaboration with NIH IC leadership and staff. While general outlines of Implementation Tactics
are presented in this strategic plan as a roadmap for how the Overarching Goals and Strategic Objectives
will be achieved, implementation details will be determined by the NIH Chief Data Strategist in
collaboration with working groups established by the NIH Scientific Data Council and NIH Data Science
Policy Council, in consultation with the ICs, other federal and international agencies, the research
community, the private sector, and other key stakeholder groups.
Since evaluation is a critical component of stewardship of federal resources, NIH will also develop
performance measures and specific milestones that will be used to gauge progress and suggest
modifications. General examples of possible qualitative and quantitative metrics and milestones have
been presented in the context of each Overarching Goal section to give a frame of reference and help
guide the community’s thinking about developing optimal evaluation metrics and strategies.
27
NIH recognizes fully that technological advancement and unprecedented growth in biomedical data
have created great opportunities, but they have also introduced great challenges for protecting the
privacy and security of patient and other research data. NIH must work with its stakeholders and experts
in the private sector and other federal agencies to promote and practice robust and proactive
information-security procedures to ensure appropriate stewardship of patient and research-participant
data while at the same time enabling scientific and medical advances. Because the data-science
ecosystem is evolving rapidly, this strategic plan is intended to be nimble enough to make necessary
course corrections through an ongoing process of performance evaluation, needs assessment, and
research and technology landscape surveys. NIH’s corporate strategy for positioning itself within a highly
dynamic biomedical data-science enterprise will poise the agency to maximize the utility of data science
for discovery while minimizing duplication of effort and ensuring that its research investments are cost-
effective for American taxpayers.
Strategic Planning Process
The NIH Strategic Plan for Data Science was conceived by the NIH Science Data Council, with input from
the NIH Data Science Policy Council, HHS, scientists, policymakers, scientific and professional societies,
the general public, and IC and NIH leadership and staff. This process was augmented by analysis of
comments from a public Request for Information about the draft Strategic Plan. Results of that analysis
revealed that 822 unique comments were contributed from the following responder types:
• Academic institution
• Advocacy group
• Government agency
• Health professional
• Member of the public
• Other
• Patient community
• Private sector
• Professional society
• Scientific research organization
The majority of responses to the RFI were supportive of the Overall Goals and Strategic Objectives but
offered specific comments or suggestions. Frequently mentioned topics that were clarified relate to
workforce training, performance metrics, data security, data standards, the definitions of databases and
knowledgebases, open-source/access tools, and collaboration with other federal and international
agencies. The NIH Scientific Data Council staff reviewed all comments and appreciated the extensive
input from NIH’s broad array of stakeholders. Revisions were made to the Strategic Plan based on the
comments received, prioritizing those that were made most frequently, those that addressed key gaps
or opportunities, and those that made important clarifications. NIH envisions that implementation of
the NIH Strategic Plan for Data Science will be equally consultative with NIH stakeholders toward
28
enhancing the scientific community’s ability to address new challenges in managing, integrating,
accessing, analyzing, and making reusable the huge amounts of data being generated by the biomedical
research ecosystem.
29
Glossary
Algorithm—a process or set of rules to be followed in calculations or other problem-solving operations
Application-programming interface (API)—clearly defined method of communication between different
software components
Artificial intelligence—the power of a machine to copy intelligent human behavior
Biocuration—the process of organizing, representing, and making accessible biological data to both
humans and computers.
Cloud computing—an internet-enabled shared system of resources usable by many individuals and
groups
Common data element (CDE)—piece of data common to multiple datasets across different studies (may
be universal or domain-specific)
Crowdsourcing—a distributed model in which individuals or groups obtain services, ideas, or content
from a large, relatively open and often rapidly-evolving group of internet users
Database/Data repository—virtual data storage that stores, organizes, validates, and makes accessible
core data related to a particular system or systems
Dataset—collection of related sets of information composed of separate elements that can be
manipulated computationally as a unit
Data commons—a shared virtual space in which scientists can work with the digital objects of
biomedical research such as data and analytical tools
Data ecosystem—a distributed, adaptive, open system with properties of self-organization, scalability,
and sustainability inspired by natural ecosystems.
Data integrity—the accuracy and consistency of data stored in a database/data repository, data
warehouse, data mart or other construct
Data provenance—timeline of ownership, location, and modification of data, akin to “version control”
Data science—interdisciplinary field of inquiry in which quantitative and analytical approaches,
processes, and systems are developed and used to extract knowledge and insights from increasingly
large and/or complex sets of data
Data security—policies, processes, methods, and tools used to prevent access to electronic information
systems for malicious use or corruption of data.
Data standards—documented agreements on representation, format, definition, structuring, tagging,
transmission, manipulation, use, and management of data.
Data visualization—effort to help people understand the significance of data by placing it in a visual
context. Patterns, trends and correlations that might go undetected can be exposed and recognized
more easily with data-visualization techniques.
Deep learning—type of machine learning in which each successive layer uses output from the previous
layer as input; similar to communication patterns in a biological nervous system
Domain-specific—for biomedical data, designed and intended for use in studies of a particular topic,
disease or condition, or body system (compare to universal)
Electronic health record—digital version of a patient's paper chart. EHRs are real-time, patient-centered
records that make information available instantly and securely to authorized users (also referred to as
electronic medical records).
30
Enterprise system—computer hardware and software used to satisfy the needs of an organization
rather than individual users
Exascale computing—a computer system capable performing one quintillion (10
18
) calculations per
second
Extramural—research or other activities supported by NIH and conducted by external organizations, and
funded by grants, contracts, or cooperative agreements from NIH
Genotype—the genetic make-up of an individual organism
Hardening—process of optimizing a tool or algorithm to industry standards to ensure efficiency, ease of
use, security, and utility
Hardware—collection of physical parts of a computer system
Indexing—methods to allow data finding and retrieving
Interoperability—in computer systems, the ability to exchange and make use of information from
various sources and of different types
Intramural—research or other activities conducted by, or in support of, NIH employees on its Bethesda,
Maryland, campus or at one of the other NIH satellite campuses across the country
Knowledgebase—virtual resource that accumulates, organizes, and links growing bodies of information
related to core datasets
Machine learning—a field of computer science that gives computers the ability to learn without being
explicitly programmed by humans
Metadata—data that describe other data. Examples include title, abstract, author, and keywords
(publications); organization and relationships of digital materials; and file types or modification dates.
NIH IC—NIH Institute or Center
'Omics—collective characterization and measurement of pools of biological molecules that translate
into the structure, function, and dynamics of an organism or organisms. Examples include genomics,
proteomics, metabolomics, and others.
Ontology—A set of terms or concepts defining the properties or identities of subjects (e.g., genes,
proteins, conditions) and relationships between them; similar to a standardized vocabulary
Petascale computing—a computer system capable performing one quadrillion (10
15
) calculations per
second. It is currently used in weather and climate simulation, nuclear simulations, cosmology, quantum
chemistry, lower-level organism brain simulation, and fusion science.
Phenotype—the set of observable characteristics of an individual resulting from the interaction of its
genotype with the environment
Platform—group of technologies (software and hardware) upon which other applications, processes, or
technologies are developed
Platform as a Service (PaaS)—a type of cloud computing that allows users to develop, run, and manage
applications without the complexity of building and maintaining an overarching infrastructure
Retirement (of data)—the practice of shutting down redundant or obsolete business applications while
retaining access to the historical data
Software—programs and other operating information used by a computer
Software as a Service (SaaS)—software licensing and delivery model in which software is licensed on a
subscription basis and is centrally hosted

31
System integrator/system engineer—individual who refines and hardens tools from academia to
improve user design, authentication and testing, and optimize productivity, efficiency, and
outcomes/performance
Trusted partner—a public or private, national or international organization that is able to meet core NIH
standards for establishing data-quality and data-management service protocols, based on the
programmatic need of one or more NIH IC
Unique identifiers—an alphanumeric string (such as 1a2b3c) used to uniquely identify an object or
entity on the internet
Universal—for biomedical data, usable in research studies regardless of the specific disease or condition
of interest (compare to domain-specific)
Wearables—devices that can be worn by a consumer that collect data to track health
Workflow—defined series of tasks for processing data

