
Revision 2, October 2022
This guidance document offers service providers a practical guide to reviewing Pressure
Ulcers. It should be read in conjunction with the HSE Incident Management Framework.
Connect with us at:
@National QPS

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 1
Reader Information
Acknowledgments:
All who contributed to the development, review and update of this tool
for the review of Pressure Ulcers. (Please refer to Appendix 6 and
Appendix 7 of this document)
Developed by:
National Incident Management (IM) Team, QPSD, in conjunction with
the Pressure Ulcer Review Tool Development and Review Groups.
Title:
Pressure Ulcers: A Practical Guide for Review
Version Number:
Version 2
Published Date:
October 2022
Subject:
Pressure Ulcers Review Tool
ISBN Number:
Cite this document as:
Pressure Ulcers: A Practical Guide for Review, Version 2, 2022, Incident
Management Team, Quality and Patient Safety Directorate.
For further information
contact:
Incident Management Team, QPSD, QRS.Tullamore@hse.ie
Or https://www.hse.ie/eng/about/who/nqpsd/qps-incident-
management/
Associated documents:
Incident Management Framework:
https://www.hse.ie/eng/about/who/nqpsd/qps-incident-
management/
National Incident Management System:
https://www.hse.ie/eng/about/who/nqpsd/qps-incident-
management/nims/national-incident-management-system-nims-.html
Revision date:
October 2022
Access:
https://www.hse.ie/eng/about/who/nqpsd/qps-incident-
management/
Version Control
Date
Revision
Created by
Reviewed by
Final document
approved by
2018
1
QAVD, HSE
National Director QAV
October
2022
2
National QPSD Incident
Management (IM) Team
National Clinical
Director QPSD/AND IM
Connect With Us
Email address: NQPS@hse.ie
Twitter: @NationalQPS
Telephone: (021) 4921501
Website: https://www.hse.ie/eng/about/who/nqpsd/

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 2
TABLE OF CONTENTS
Introduction ............................................................................................................................... 3
Aim ............................................................................................................................................ 4
Scope ......................................................................................................................................... 4
Abbreviations ............................................................................................................................ 5
Pressure Ulcer Staging System .................................................................................................. 6
Incident Management Process: Pressure Ulcers....................................................................... 7
Step 1: Pressure Ulcer Prevention – including Pressure Ulcer Risk Assessment ...................... 8
Step 2: Identification and Actions Required ............................................................................. 9
Step 3: Initial Reporting and Notification ................................................................................ 10
Step 4: Assessment and Categorisation of the Incident ......................................................... 12
Step 5: Review and Analysis ................................................................................................... 19
Step 6: Improvement Planning and Monitoring ..................................................................... 21
References ............................................................................................................................... 22
Appendix 1. HSE Pressure Ulcer Category/Staging System Recommendation....................... 24
Appendix 2 SSKIN bundle ........................................................................................................ 26
Appendix 3 Preliminary Assessment to Assist Review Decision Making ................................ 27
Appendix 4. Conducting a Concise Review Guidance ............................................................. 29
Appendix 5. Pressure Ulcer Review Report Template ............................................................ 34
Appendix 6. Membership of the Pressure Ulcer Review Guide Development Group (2018) 41
Appendix 7. Membership of the Pressure Ulcer Review Guide Review Group (2022) .......... 41
Use of the Term “Service User” in this document
*Note: The term Service User is used in this document to include any persons who use health
and social care service within HSE and HSE-funded acute hospitals, mental health and social
care inpatient/residential facilities and the community
The term Service User also includes their appropriate Relevant Person who has been legally
assigned, or who has been nominated in writing to the health services provider, as a person to
whom clinical information in relation to the patient may be disclosed.
Relevant Persons is defined in the Civil Liability (Amendment) Act 2017 as:
“Relevant person”, in relation to a patient, means a person— (a) who is— (i) a parent,
guardian, son or daughter, (ii) a spouse, or (iii) a civil partner of the patient, (b) who is
cohabiting with the patient or (c) whom the patient has nominated in writing to the health
services provider as a person to whom clinical information in relation to the patient may be
disclosed
1
.
1
Note : This definition must not be conflated with the definition of “relevant person” in the Assisted Decision-Making
(Capacity) Act 2015

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 3
Introduction
The HSE Patient Safety Strategy
2
highlighted Pressure Ulcers as one of the Common Causes of Harm and
a priority area for patient safety improvement. A pressure ulcer is a “localised injury to the skin and/or
underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination
with shear” (1). These wounds occur frequently among individuals who have difficulty moving, or cannot
reposition themselves, such as the frail elderly, individuals undergoing surgery, or individuals with spinal
cord injury. However, any Service User, of any age, could develop a pressure ulcer if they are exposed
to prolonged, unrelieved pressure and shear forces (2).
Pressure ulcers are common. Within acute and long stay settings in Ireland, the mean pressure ulcer
prevalence is estimated at 12.04% (3). This figure reflects the international data where an overall
European mean PU prevalence of 13.1% and a European median PU prevalence rate of 10.8% among
hospitalised patients (standard deviation (SD): 7%; range: 4.6–27.2%) has been reported (3). Prevalence
rates of between 6% and 18.5% have recently been reported in acute care settings (4) and between 3.4–
32.4% in long term care settings (5). A more recent study by the OECD indicated that the prevalence of
pressure injuries of all stages in long-term care facilities was between 0.9% and 13.1% among OECD
countries for which data were available (OECD, 2020 (6))
A study of the global burden of pressure ulcers from 1990 to 2019 (7) identified that the age-
standardised rates of prevalence, incidence, and years lived with disability (YLDs) in 2019 are 11.3 (95%
UI 10.2 to 12.5), 41.8 (37.8 to 46.2), and 1.7 (1.2 to 2.2) per 100,000 population, and compared with
1990, it has decreased by 10.6% (95% UI 8.7% to 12.3%), 10.2% (8.2 to 11.9%), and 10.4% (8.1 to 12.5%),
respectively. In addition, this study highlighted that the global prevalence rate of pressure ulcers
increases with age, peaking at the > 95 age group among men and women.
Pressure ulcers pose significant physical and psychological challenges for individuals, impacting
negatively on activities of daily living with severe, intractable pain, being one of the most common and
difficult aspects of living with a pressure ulcer (8-12). From a financial perspective, pressure ulcers not
only impact on the individual, but also on health services and by proxy, society as a whole. Recent data
suggest that the cost of pressure ulcers is estimated at between 2 and 4% of total health expenditure
(13).
From an Irish perspective, a recent study (14) estimated the financial burden of wounds in general, at
5% (95% CI: 3% to 6%) of total public health expenditure in Ireland for 2017. Given the high prevalence
and incidence of pressure ulcers, it is likely that these wounds significantly contribute to this
expenditure. Most pressure ulcers can be avoided, providing individuals at risk are correctly identified
and appropriate measures are put into place to combat risk. Despite this, the development of pressure
ulcers often arises because there has been a failure to implement appropriate prevention strategies.
Annually, in the UK, of the 6 most common adverse events, the greatest burden was exerted by pressure
ulcers equating to 13,780 healthy life years lost (13). Worryingly, individuals can die as a direct result of
2
https://www.hse.ie/eng/about/who/nqpsd/patient-safety-strategy-2019-2024.pdf

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 4
a pressure ulcer, indeed, global mortality directly attributable to pressure ulcers increased by 32.7%
between the years 2000 to 2010 (15)
A proportionate and responsive review of all stages of pressure ulcers when identified can assist in
detecting factors that caused and contributed to the development of the pressure ulcer. Such
information can then be used to implement improvement initiatives that could prevent subsequent
tissue damage to the individual and prevent other Service Users in developing a pressure ulcer. It also
gives assurance that appropriate governance structures and processes are in place, as required by the
HSE Incident Management Framework.
3
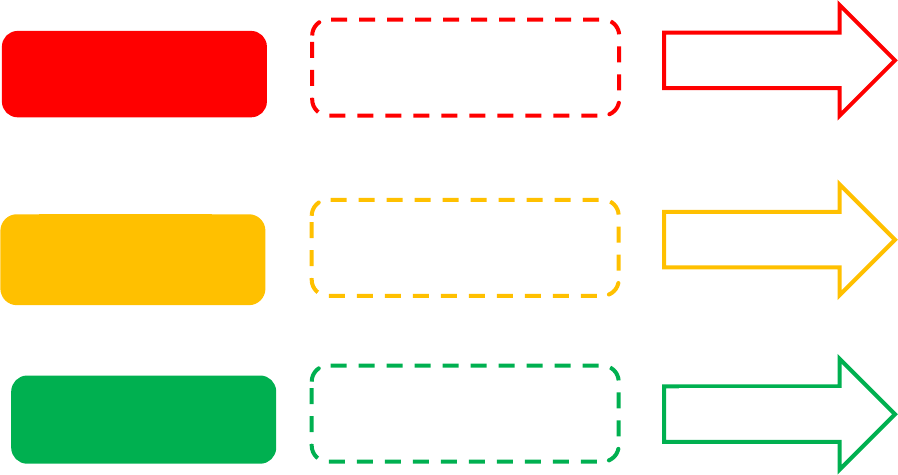
The HSE Incident Management Framework describes the following six steps in the management of
incidents:
• Prevention through supporting a culture where safety is a priority
• Identification and immediate actions required (for Service Users directly affected and to
minimise risk of further harm to others)
• Initial reporting and notification
• Assessment and categorisation
• Review and analysis
• Improvement planning and monitoring
Aim
The aim of this document is to give services a practical guide to reviewing pressure ulcers which aligns
to the six steps described in the HSE Incident Management Framework (see Figure 1).
Scope
The scope of this document relates to the review of pressure ulcers identified and reported for
Service Users within HSE and HSE-funded acute hospitals, mental health and social care
inpatient/residential facilities and the community. This document should be read in conjunction
with the HSE Incident Management Framework.
This guideline is to be applied by staff in HSE and HSE-funded acute hospitals, mental health and
social care inpatient/residential facilities and the community.
3
For the most current version of the Incident Management Framework and templates please access:
https://www.hse.ie/eng/about/who/nqpsd/qps-incident-management/
Note: The Incident Management Framework and associated templates are regularly reviewed and improved.
Please always refer to the National QPSD Incicent Management Team website to ensure that the most up to
date framework and templates are utilised.

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 5
Abbreviations used in this Guide
A full list of abbreviations and definitions is available in the Incident Management Framework which
should be read in conjunction with this Concise Review Tool. The following are abbreviations used in
this document.
CHO Community Healthcare Organisation
EPUAP European Pressure Ulcer Advisory Panel
HIQA Health Information and Quality Authority
HSCP Health and Social Care Professional
HSE Health Service Executive
IMF Incident Management Framework
LAO Local Accountable Officer e.g. line manager
MDT Multidisciplinary Team
NIRF National Incident Report Form
NIMS National Incident Management System
NPUAP National Pressure Ulcer Advisory Panel
NQPSD National Quality and Patient Safety Directorate
OECD Organisation for Economic Co-operation and Development
PPPIA Pan Pacific Pressure Injury Alliance
PUTZ Pressure Ulcer to Zero
QI Quality Improvement
QPS Quality and Patient Safety
QPSD Quality and Patient Safety Directorate
SAO Senior Accountable Officer e.g. Head of Service or Hospital Manager
SIMT Serious Incident Management Team
SRE Serious Reportable Event
TVN Tissue Viability Nurse

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 6
Pressure Ulcer Staging System
The HSE Wound Management Guideline (2018)
4
describes the following Pressure Ulcer Staging System
(see Appendix 1):
Stage I: Intact skin with non – blanchable redness of a localised area usually over a bony prominence.
Discolouration of the skin, warmth, oedema, hardness or pain may also be present. Darkly pigmented
skin may not have visible blanching. The area may be painful, firm, soft, warmer or cooler as compared
to adjacent skin.
Stage II: Partial thickness skin loss of dermis presenting as a shallow ulcer with a red pink wound bed,
without slough. May present as an intact or open/ ruptured serum filled blister filled with serous or sero-
sanguineous fluid. Presents as a shiny or dry shallow ulcer without slough or bruising.
Stage III: Full thickness skin loss. Subcutaneous fat may be visible but bone, tendon or muscles are not
exposed. Slough may be present but does not obscure the depth of tissue loss. The stage may include
undermining or tunnelling.
Stage IV: Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be
present. This stage often includes undermining and tunnelling. Exposed bone / muscle is visible or
directly palpable.
Suspected deep pressure and shear induced tissue damage, depth unknown
For Service Users with non-blanchable redness and purple/maroon discoloration of intact skin combined
with a history of prolonged, unrelieved pressure/shear, this skin change may be an indication of
emerging, more severe pressure ulceration i.e. an emerging Stage III or IV Pressure Ulcer. Clear
recording of the exact nature of the visible skin changes, including recording of the risk that these
changes may be an indication of emerging more severe pressure ulceration, should be documented in
the Service User’s health record. These observations should be recorded in tandem with information
pertaining to the Service User’s history of prolonged, unrelieved pressure/shear.
It is estimated that it could take 3-10 days from the initial insult causing the damage, to become a Stage
III or IV Pressure Ulcer.
5
Stable eschar (dry adherent, intact without erythema or fluctuance) on the heel serves as the body’s
biological cover and should not be removed. It should be documented as at least Category / Stage III
until proven otherwise.
See Appendix 1 for illustration of the HSE Pressure Ulcer Category/Staging System Recommendations.
4
HSE National Wound Management Guidelines available at: https://healthservice.hse.ie/about-us/onmsd/quality-nursing-
and-midwifery-care/hse-national-wound-guidelines-2018.html

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 7
Incident Management Process: Pressure Ulcers
1. Pressure Ulcer
Prevention including Risk Assessment
2. Immediate
Actions
3. Initial
Notification
and
Reporting
4. Assessment
and
Categorisation
5. Review
and Analysis
6. Improvement
Planning and
Monitoring
Implement any
immediate
actions required
to reduce risk of
further
progression or
development of
new pressure
ulcers
Provide support to Service User
and staff involved
Attend to any
clinical/care needs
Pressure
Ulcer
Identified
Notify
Line
Manager
Complete an
incident report
form
Ensure Open
Disclosure and
consider any external
reporting
requirements
Categorise
the Incident
Consider whether further review
is required or for consideration in
Aggregate Review
Establish
the
Review
Conduct the review. Involve
relevant persons e.g. staff and
Service Users
Submit the report for signoff via
agreed process
Develop
Action Plan
Share Learning
Monitor implementation of
action plan
Within the service and consider
the need to share more broadly
Maintain openness and transparency with all those affected throughout
Figure 1: Adapted from HSE Incident Management Framework

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 8
Step 1: Pressure Ulcer Prevention – including Pressure Ulcer
Risk Assessment
In 2021, 6,529 pressure ulcer incidents reported through the National Incident Management System
5
were acquired by services users while in the care of the HSE. Of these, 4,824 were reported as acquired
by Service Users in acute hospitals with 1,676 reported as relating to Service Users in the care of CHOs.
A moderate level of harm was reported in 1,799 of these reported incidents with an additional four
pressure ulcer incidents classified as resulting in extreme or major harm.
The HSE National Wound Management Guidelines (2018) provide a standardised approach for wound
care in the Irish healthcare setting to support safe, quality care for Service Users, who access healthcare
across the HSE and HSE funded agencies. For more in-depth guidance on wound care please consult
these guidelines
6
. All inpatient, residential and community care services should have local guidelines in
place on pressure ulcer prevention and management, centred on the HSE National Wound Management
Guidelines.
Pressure ulcer prevention is based on the principle that prevention strategies are planned and based on
the individual risk factors that the Service User presents with. Pressure ulcer prevention strategies are
informed by risk assessment and clinical judgement. Risk assessment is therefore the first step in the
prevention process (17). Evidence suggests that the best practice in Pressure Ulcer prevention is by
incorporating a SSKIN
7
bundle into the Service Users care (Appendix 2) (18-21). The SSKIN bundle can be
applied across all areas of care and can be instigated where a Service User is deemed at risk of pressure
ulcer development as indicated by clinical judgement and/or by use of an assessment tool. Key to the
success of implementing the SSKIN bundle is to apply each element to each Service User in the same
way, as required, every time. This helps build reliability into prevention processes.
Implementation of the SSKIN bundle in clinical services is a key component of the HSE QPSD Pressure
Ulcer to Zero Collaborative (PUTZ). PUTZ aims to reduce facility
acquired pressure ulcers by 50% during the lifetime of each phase of
the collaborative. To achieve this aim the collaborative provides
teams with the support and educational resources needed to undertake improvements. It also enables
staff to put in place reliable systems so that improvements can be maintained, and become continuous
during and after the Collaborative period. PUTZ and SSKIN resources are available to the public and HSE
staff to support pressure ulcer prevention, along with further information through the NQPSD website
at:https://www.hse.ie/eng/about/who/nqpsd/patient-safety-programme/pressure-ulcers-to-zero-putz-
.html
5
Data extracted from NIMS on 13/4/22. The National Incident Management System (NIMS) is a dynamic system and is the
key platform for HSE and HSE-funded healthcare providers to report incidents on. Additionally, the NIMS system is the source
of data in terms of incident management as a quality indicator and is also used to inform the National Service Plan KPIs. More
information is available at https://www.hse.ie/eng/about/who/nqpsd/qps-incident-management/nims/national-incident-
management-system-nims-.html or NIMS helpdesk at [email protected].
6
HSE National Wound Management Guidelines available at: https://healthservice.hse.ie/about-us/onmsd/quality-nursing-
and-midwifery-care/hse-national-wound-guidelines-2018.html
7
The SSKIN bundle focusses on key aspecs of preventative care: Surface, Skin Inpection, Keep Moving, Incontinence and
Nutrition

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 9
Step 2: Identification and Actions Required
(For Service Users directly affected and to minimise risk of further harm to others)
There are a number of immediate actions that should be completed in the period following the
identification of a pressure ulcer to both prevent further damage and the development of new pressure
ulcers.
1. Ensure that a Pressure Ulcer Risk Assessment has been completed
2. Ensure the SSKIN bundle/Pressure Ulcer Prevention Care Plan is appropriate to the Service
User’s current risk status.
3. Continue vigilance with skin inspection and ensure a wound assessment / management care
plan is in place for each area of skin damage.
4. Document findings and actions taken in relation to the on-going management of the pressure
ulcer in the Service User’s care record.
5. Ensure the Service User is made aware of the pressure damage (Open Disclosure
8
) and is given
information in relation to next steps.
a. This is essential as it significantly contributes to the maintenance of confidence in, and
trust between, the Service User and the service providers.
b. A record of the salient points of the Open Disclosure discussion and details of the
apology and/or expression of regret provided to the Service User should be made in the
Service User’s healthcare record.
6. Continue, with the involvement of the multidisciplinary team (MDT), to evaluate the
effectiveness of equipment, repositioning frequency, incontinence management and nutritional
interventions.
7. Continue to evaluate the effectiveness of wound management strategies.
8
The most up to date HSE Open Disclosure Policy and related information may be accessed at
https://www.hse.ie/eng/about/who/nqpsd/qps-incident-management/open-disclosure/national-open-disclosure-policy-and-
guidelines.html

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 10
Step 3: Initial Reporting and Notification
There is a requirement to report the following pressure ulcer incidents via the National Incident
Management System (NIMS)
9
,
10
.
a) All newly acquired pressure ulcers, regardless of stage, occurring within a publically funded
health service (See Note 1 below);
b) Existing pressure ulcers which progress/deteriorate to a Stage III or IV Pressure Ulcer;
c) Non-blanchable redness and purple/maroon discoloration of intact skin combined with a history
of prolonged, unrelieved pressure/shear (see Note 2 below).
Note 1: Pressure Ulcer Present on Admission
There is no requirement to report pressure ulcers which are present on admission to a facility or present
at the time of first contact in the community. Rather these should be noted in the healthcare record of
the Service User and their care plan should reflect any actions required to prevent further deterioration.
This is because the pressure ulcer should already been reported on NIMS by the service in which the
Service User was previously being cared for (see below).
Remember: When referring a Service User externally to another healthcare facility, or internally to
another ward, the referring service/team must document on the Service User’s accompanying
documentation and healthcare records that the pressure ulcer has been reported at local and national
level.
Note 2: Pressure Ulcer Staging and NIMS
In cases where there is suspected deep pressure and shear induced tissue damage, depth unknown, it
is estimated that it could take 3-10 days from the initial insult causing the damage, to become a Stage
III or IV Pressure Ulcer. In such circumstances when completing Section G of the National Incident Report
Form (NIRF) (NIRF 01, Person), in the section Musculoskeletal/Soft Tissue, select ‘Other’ and enter ‘Non-
blanchable redness and purple/maroon discoloration of intact skin’.
When the Pressure Ulcer is stageable, if the Service User is still a patient in the department/ service in
which the initial NIRF was completed, then the original NIRF and the associated incident on NIMS are
updated to denote the staging of the pressure ulcer.
However, if during the period from initial insult to staging of the pressure ulcer, the Service User is
moved from the department/service, the need for the completion of incident reporting to capture the
staging of the pressure ulcer, should form part of the handover of care.
When the pressure ulcer becomes stageable, a further NIRF form should be completed by the receiving
department/service denoting the stage of the pressure ulcer. This second NIRF (and any subsequent
NIRFs related to this pressure ulcer) should be linked to the original NIRF on NIMS so that it is captured
on NIMS that the incidents are related.
9
Reporting on NIMS via National Incident Report Form (NIRF) or directly on to NIMS (where electronic point of entry is
available).
10
To aid with local data capture and audit of pressure ulcers, local pressure ulcer data collection systems may also be utilised
as stipulated and guided by local, service level requirements. However, these systems should not replace the requirement to
report pressure ulcer incidents via NIMS.

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 11
The staff member who identified the pressure ulcer is responsible for:
Notifying the line manager within the area where the pressure ulcer occurred/was identified.
Completing an NIRF as soon as is practicable after the pressure ulcer is identified, but within 24
hours of the identification of the pressure ulcer.
o All information must be provided in full, as required on the NIRF and must be factual and
objective. This is important as it assists in supporting a just and fair culture.
o It is important in completing a NIRF relating to a facility/community acquired pressure ulcer or
progression of an existing pressure ulcer to include detail of the staging that is relevant. This is
important as Stage III & IV Pressure Ulcers are designated as Serious Reportable Events. If
necessary, consult a health care professional with specialist pressure ulcer knowledge e.g.
Clinical Nurse Manager, Medical Staff, Tissue Viability Specialist (TVN) to ensure that the correct
Stage of the Pressure Ulcer is applied.
Local services must clearly identify, and communicate to staff, the route for submission of the NIRF
for input onto the NIMS. Stage III or IV Pressure Ulcers, if acquired since admission to the service,
are also classified as Serious Reportable Events (SREs) and must be identified on NIMS as SREs and
reported externally as set out by the relevant regulatory bodies
11
.
The Mental Health Commission
12
requires any serious reportable event involving a resident to be
reported within 48 hours and, as part of the obligation for quarterly statutory notifications in
designated centres (NF39), Residential Services are also required to notify pressure ulcers Stage II
and higher to the Health Information and Quality Authority (HIQA)
13
. Deaths related to pressure
ulcers in any service are reportable to the Coroner.
11
Refer to the Incident Management Framework Guidance document (Section 6) for external reporting requirements.
12
Mental Health Commission (2020) requires any serious reportable event involving a resident to be reported within 48
hours, guidance available at https://www.mhcirl.ie/sites/default/files/2021-08/MHC-QSN-Guidance-November-2020.pdf
13
HIQA, Monitoring Notifications handbook available at https://www.hiqa.ie/sites/default/files/2018-02/Monitoring-
Notification-Handbook-DCOP_Guidance.pdf

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 12
Step 4: Assessment and Categorisation of the Incident
The purpose of assessing and categorising incidents is to determine the level and approach of review
that is required. Categorisation is based on the level of harm sustained as a consequence of the pressure
ulcer and is in line with the categorisation of incidents described in the HSE Incident Management
Framework.
The level and approach of review must be proportionate to the harm sustained as a result of a pressure
ulcer.
Based on the outcome of this assessment, pressure ulcer incidents are categorised as follows:
Category 1 Incident Major/Extreme
Pressure Ulcers of any grade which are
o associated with septicaemia resulting in death
Or
o Resulting in permanent disability such as an amputation.
Category 2 Incident Moderate
Stage III & IV Pressure Ulcers
o not associated with septicaemia resulting in death
Or
o not resulting in a permanent disability
Note: Category 1 and Category 2 are also classified as Serious Reportable Events (SREs) if acquired since
contact/admission to either the community or acute services.
Category 3 Incident Minor/Negligible
Stage I & II Pressure Ulcers
Note: However, it is important that services continue to monitor and assess these pressure ulcers to
identify any deterioration.
QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 13
Decision making in relation to the review of Pressure Ulcer Incidents
Based on the categorisation of the incident, a graduated and proportional level of review (i.e.
Comprehensive, Concise and Aggregate) should be considered in line with the HSE Incident
Management Framework.
The incident category applied to the pressure ulcer will point you to the appropriate review process to
follow.
Category 1
Incident
Go to Page 14
Category 2
Incident
Category 3
Incident
Go to Page 16
Go to Page 18
Consider Comprehensive
Review
Consider Concise
Review
Consider Aggregate
Review

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 14
Decision Making for Category 1 Pressure Ulcer Incidents
In line with the HSE Incident Management Framework, Category 1 incidents, when identified, must be
notified to the Senior Accountable Officer (SAO) within 24 hours. The arrangement for notification must
be clearly defined within each organisation. The SAO is required to convene a meeting
14
of the Serious
Incident Management Team (SIMT) within 5 working days to make a decision in relation to review.
Category 1 pressure ulcer incidents are SREs and therefore must also be categorised as an SRE on NIMS.
Preparing for Decision Making by the SIMT
In order to assist decision making at the SIMT, the Quality and Patient Safety (QPS) Advisor arranges for
collection of data relating to the pressure ulcer required by the Preliminary Assessment to Assist Review
Decision Making form (Part A) (Appendix 3). The data required to complete this form should be accessed
from relevant sources e.g.
The line manager in whose area of responsibility the pressure ulcer occurred
Clinically relevant persons e.g. Tissue Viability Lead
15
, Health and Social Care Professional (HSCP)
etc.
National Incident Report Form
Service User’s healthcare record
Engagement with:
o staff who were either on duty or involved in the Service User’s care prior the incident
o the Service User
Decision Making by the SIMT
Using the data collected in Part A, the SIMT should determine if there was evidence of the following:
Failure to adequately or consistently apply one or more of the following interventions increased the
likelihood that the service user would develop a pressure ulcer:
evaluate the Service User’s clinical condition and pressure ulcer risk factors and/or
plan and implement interventions that are consistent with the Service User’s needs and goals, and
recognised standards of practice and/or
monitor and evaluate the impact of the interventions or revise the interventions as appropriate.
Based on this determination, a decision is taken in relation to the conduct of a review. A Comprehensive
Review approach to review is generally accepted as most appropriate for Category 1 incidents. However,
a Concise approach to review may be considered for some Category 1 incidents (Refer to the Incident
Management Framework for further guidance on the level of review to be adopted).
14
In line with the IMF, the SIMT meets on a scheduled basis to monitor and gain assurance in relation to the ongoing
management of all Category 1 incidents within the service. The SIMT must also convene on an unscheduled basis within 5
working days of a Category 1 incident.
15
This may be a local clinical manager such as Clinical Nurse Manager 2, Assistant Diretcor of Nursing, Person-in-Charge or a
person with specialist knowledge in tissue viability
Category 1
Incidents
(Major/Extreme
Harm)

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 15
Where a decision to review using a Comprehensive or Concise approach is taken, this is noted in Part B
of the Preliminary Assessment to Assist Review Decision Making form along with other required
information and the SAO moves to establish the review. The SAO is now the Commissioner of the
Review. The decision to review along with detail of the approach being undertaken must be recorded
on the NIMS review screens
16
.
Where a decision not to review using a Comprehensive or Concise approach is taken, the completed
Preliminary Assessment to Assist Review Decision Making form (Part A and Part B) must be submitted to
the relevant Quality and Safety Committee (or equivalent) for review and ratification of the decision.
The decision not to review, when ratified by the Quality and Safety Committee (or equivalent), must be
recorded on the NIMS review screens.
16
More information on recording on the NIMS review screens is available on the NQPSD Incident Management Team
webpage at https://www.hse.ie/eng/about/who/nqpsd/qps-incident-management/nims/national-incident-management-

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 16
Decision making for review of Category 2 Pressure Ulcer Incidents
Category 2 pressure ulcer incidents are classified as SREs and must be reported as an SRE on NIMS.
Unlike Category 1 incidents, there is not a requirement to notify the SAO within 24 hours
17
nor is there
a requirement to convene a SIMT to make decisions about review. Decisions relating to review are taken
by the QPS Advisor (or equivalent) in consultation with Local Accountable Officer (LAO) as soon as
possible after the identification of a Category 2 pressure ulcer.
Preparing for decision making
In order to assist decision making, the service where the incident occurred is responsible for the
collection of data relating to the pressure ulcer as required by the Preliminary Assessment to Assist
Review Decision Making form (Part A) (Appendix 3). The data required to complete this form should be
accessed from relevant sources e.g.
The line manager in whose area of responsibility the pressure ulcer occurred
Clinically relevant persons
18
e.g. Tissue Viability Lead, Health and Social Care Professional etc.
National Incident Report Form
Service User’s healthcare record
Engagement with
o staff who were either on duty or involved in the Service User’s care prior the incident
o the Service User
The Preliminary Assessment to Assist Review Decision Making form should be returned to the relevant
QPS Advisor or equivalent and having reviewed the data in Part A, an assessment is made by the QPS
Advisor (or equivalent) in conjunction with the LAO, as to whether there is evidence of the following:
Failure to adequately or consistently apply one or more of the following interventions increased the
likelihood that the service user would develop a pressure ulcer:
evaluate the Service User’s clinical condition and pressure ulcer risk factors and/or
plan and implement interventions that are consistent with the Service User’s needs and goals, and
recognised standards of practice and/or
monitor and evaluate the impact of the interventions or revise the interventions as appropriate.
Decision making
Where it is agreed that there was evidence of a failure to adequately or consistently apply one or more
of the interventions required to avoid the development of a pressure ulcer a concise approach to review
is generally considered appropriate.
Where a decision to review using a concise approach is taken, it is noted in Part B of the form along with
other required information and the LAO proceeds to commission and establish the review.
17
It is however recommended that as Grade III and IV Pressure Ulcers are designated as SREs, that the SAO receive a monthly
report in relation to the number of these reported in the previous month.
18
This may be a local clinical manager such as CNM2, ADON, Person-in-Charge or a person with specialist knowledge in tissue
viability
Category 2
Incidents
(Moderate
Harm)

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 17
If, in exceptional circumstances, it is considered that a comprehensive approach is indicated this must
be referred by the LAO to the SAO who is responsible for commissioning comprehensive reviews. The
decision to review along with detail of the process to be undertaken must be recorded on the NIMS
review screens
19
.
Where a decision is taken not to review using either a Comprehensive or Concise approach, the
completed Preliminary Assessment to Assist Review Decision Making form (Part A and Part B) must be
submitted to the relevant Quality and Safety Committee (or equivalent) for review and ratification of
the decision. The decision not to review, when ratified by the Quality and Safety Committee (or
equivalent), must be recorded on the NIMS review screens.
19
More information on recording on the NIMS review screens is available on the NQPSD Incident Management Team
webpage at https://www.hse.ie/eng/about/who/nqpsd/qps-incident-management/nims/national-incident-management-

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 18
Decision Making for Category 3 Pressure Ulcer Incidents
In the main Category 3 pressure ulcer incidents should be collated and analysed on an aggregate basis.
See Point 1 in Step 5, Review and Analysis, for details of this.
Whilst there is not a requirement to review these incidents individually, if it is considered that an
individual Category 3 incident presents an opportunity for learning, a concise review should be
considered.
Category 3
Incidents
(Minor/Negligible
Harm)

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 19
Step 5: Review and Analysis
The purpose of a review is to find out what happened, why it happened and what learning can be gained
in order to minimise the risk of pressure ulcers occurring in the future. The review and analysis of
pressure ulcers should be considered a key tool for quality improvement. There is a need not just to
understand what happened in relation to the pressure ulcer but also to understand why it happened
i.e. the cause and the factors that contributed to the pressure ulcer.
Review of Individual Pressure Ulcer Incidents
In line with the HSE Incident Management Framework, there are two levels of review that relate to the
conduct of review of individual cases. These are as follows:
Comprehensive Review: Comprehensive Reviews use the Review Team Approach. Guidance on the
methodology for this approach can be found in the HSE Incident Management Framework.
Concise Review: Concise Reviews use the Pressure Ulcer Concise Review Tool (Appendix 3). This tool
is specific to pressure ulcer incidents and was co-designed by Tissue Viability Specialists and QPS
Advisors experienced in the conduct of systems based reviews. The tool commences with the
conduct of a Preliminary Assessment of the pressure ulcer to enable decision making in relation to
the requirement for a review. Where a decision is taken to conduct a review, guidance on the
conduct of the concise review and the Review Report template is also provided (Appendices 4 and
5).
NIMS: To assist with aggregate analysis of Pressure Ulcer Reviews the Reporting Screens on NIMS
must be completed in full for Comprehensive and Concise Reviews. A copy of the report must also
be uploaded onto NIMS.
In relation to undertaking an Aggregate Review two types of aggregate reviews can be carried out:
1. An ‘all pressure ulcer’ aggregate review: The NIRF 01 (NIRF Person) contains data relating to
pressure ulcers in the Clinical Care Section. Services should seek to pull an ‘all pressure ulcers’
report from NIMS on a periodic basis for review at their appropriate MDT meeting/ Quality and
Safety Committee (or equivalent)
20
.
2. Concise Reports Aggregate Review: Due to the structured nature of the Concise Review
process, consideration should also be given to the conduct of aggregate analysis of Concise
Reviews completed within a service/service area. The outcome of such an analysis can
contribute to a greater understanding of the issues underlying pressure ulcers within the Service
User population. This can be done at service level, regional level, care group level and/or
national level. For this reason, it is important that completed Concise Reports are uploaded to
NIMS, and the Reporting Screens on NIMS are completed in full. Guidance on the methodology
20
More information on generating reports from NIMS is available on the NQPSD Incident Management Team webpage at
https://www.hse.ie/eng/about/who/nqpsd/qps-incident-management/nims/national-incident-management-system-nims-

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 20
for for aggregate analysis can be found in the HSE Incident Management Framework. Key
learning points from any Comprehensive Review conducted can also be incorporated into this
aggregate analysis.
Whatever approach to review is taken a report will be developed which will set out details of the case,
identify the Statement of Findings and the Factors which contributed to the development of the pressure
ulcer and set out recommendations for areas where improvement has been identified as being
required
21
(Appendix 5).
Recommendations must be linked to the Factors that contributed to the pressure ulcer and must be:
Framed in a manner that conform with CLEAR
22
principles
Capable of supporting any changes in practice required
Where possible aimed at changing systems in a manner that supports people to behave in a safe
and consistent manner rather than relying on people to behave in a specific manner.
Discussed with the Review Commissioner to ensure that they are both implementable and
consistent with the policy framework within which the service operates.
When the draft report is available it will be provided to relevant staff and the Service User to confirm
factual accuracy and provide comment within a specified timeframe in line with the Incident
Management Framework. This should be carried out in a supportive manner. It is one of the final tasks
prior to completion of the incident management cycle and it is important that appropriate consideration
is given to how this is done.
In line with the Incident Management Framework, following acceptance of the report by the
Commissioner, the Service User Designated Support Person should contact the service user to inform
them that the report is finalised and offer them a meeting to discuss this. The service user should be
offered an opportunity to receive a copy of the report in advance of the meeting and so have had a
chance to review it. Staff should also be advised of the outcome of the review in a manner that is
supportive and can be provided with a copy of the report.
Following the finalisation of the report, an action plan is developed to ensure that recommendations
made in the report are implemented. A copy of the report is also submitted to the relevant QPS Advisor
(or equivalent) for inclusion in aggregate analysis to inform learning and to enable the completion of the
review screens on NIMS. The final report and action plan is also submitted to the relevant Quality and
Safety Committee (or equivalent) for their information and consideration as part of the service’s overall
quality improvement plans.
Refer to the HSE Incident Management Framework for details on the governance and approval process
for review reports.
21
See Appendix 5 for report template and also link to template available at https://www.hse.ie/eng/about/who/nqpsd/qps-
incident-management/incident-management/incident-management.html
22
CLEAR is an acronym used to describe the key elements/features that a recommendation should have to support successful
implementation i.e. Case for Change, Learning Orientated, Evidence, Assign, Review. Reference Section 14, HSE Incident
Management Framework

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 21
Step 6: Improvement Planning and Monitoring
It is the responsibility of the person commissioning the review to ensure that an action plan to
implement any recommendations is developed. It is recommended that rather than monitor action
plans for individual reviews, that action plans developed are interfaced with relevant service
improvement plan and that the implementation of this plan be monitored.
To facilitate monitoring, actions developed must be assigned to named individuals with a due date for
completion. Where there is evidence that actions are behind schedule appropriate corrective action
must be taken to address this. Improvement plans must therefore be owned by the service and
reviewed and updated regularly. If an action is identified which is outside the control of the service a
formal system of escalation should be applied so that the action can be referred to the appropriate
level/location for implementation.
An action plan could focus on the introduction of, or audit of the use of the SSKIN Bundle to confirm
that suitable measures for pressure ulcer prevention are in place and are being used appropriately.
Improvement planning should consider how reliable SSKIN bundle processes can be implemented into
the daily routine to support pressure ulcer prevention. For example if an issue with nutrition is
identified through audit of the SSKIN Bundle it is recommended that collaboration with the Dietetics
Department (where available) and Practice Development should be initiated. The purpose of this
should be to embed understanding and continuous correct use of the local nutritional screening tool–
e.g. MUST
23
screening tool.
Effective measurement systems should be established to monitor for safe care and positive outcomes.
Daily recording of newly acquired or newly transferred pressure ulcers can be recorded on a safety
cross and publically displayed. This visual information promotes awareness and ownership for
multidisciplinary staff and facilitates a reliable reporting mechanism from a governance perspective.
For further information on the Safety Cross and for further guidance and support on other quality
improvement and pressure ulcer prevention measures visit the PUTZ website at
https://www.hse.ie/eng/about/who/nqpsd/patient-safety-programme/pressure-ulcers-to-zero-putz-
.html
To guide and support the improvement process, application of the HSE’s Framework for Improving
Quality
24
can assist in influencing and guiding the planning and delivery of care in services to help
improve Service User experience and outcomes. The framework describes six drivers of quality that
need to be considered in every improvement effort to ensure successful, continuous and sustainable
improvements in the quality of care even in the busiest environments.
23
MUST: Malnutrition Universal Screening Tool
24
Available at https://www.hse.ie/eng/about/who/nqpsd/

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 22
References
1. European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan
Pacific Pressure Injury Alliance. (2019), Prevention and Treatment of Pressure Ulcers/Injuries:
Clinical Practice Guideline. The International Guideline. Emily Haesler (ed.).
2. Moore, Z. E. H. & Cowman, S. (2014).Risk assessment tools for the prevention of pressure
ulcers. Cochrane Database of Systematic Reviews 2
3. Moore, Z., Avsar, P., Conaty, L., Moore, D.H., Patton, D.,and O'Connor, T., (2019) The
prevalence of pressure ulcers in Europe, what does the European data tell us: a systematic
review, Journal of Wound Care 28(11), 710-719
4. Tubaishat A, Papanikolaou P, Anthony D, Habiballah L. (2018), Pressure Ulcers Prevalence in
the Acute Care Setting: A Systematic Review, 2000-2015. Clin Nurs Res. Jul; 27(6):643-659.
5. Anthony, D., Alosoumi, D. and Safari, R., (2019). Prevalence of pressure ulcers in long-term
care: a global review. Journal of Wound Care, 28(11), 702-709.
6. de Bienassis, K., Llena-Nozal, A. and Klazinga, N.S., (2020). “The Economics of Patient Safety
Part III: Long-Term Care.” (121). https://www.oecdilibrary.org/content/paper/be07475c-en.
7. Zhang, X., Zhu, N., Li, Z. et al. (2021), The global burden of decubitus ulcers from 1990 to 2019.
Sci Rep 11, 21750, https://doi.org/10.1038/s41598-021-01188-4
8. Spilsbury, K. et al. (2007), Pressure ulcers and their treatment and effects on quality of life:
hospital inpatient perspectives. Journal of Advanced Nursing 57, 494-504
9. Gorecki, C. et al. (2009), Impact of pressure ulcers on quality of life in older patients: a
systematic review. Journal of the American Geriatrics Society 57, 1175-1183
10. Gorecki, C., Closs, S. J., Nixon, J. & Briggs, M. (2011), Patient-reported pressure ulcer pain: A
mixed-methods systematic review. Journal of Pain and Symptom Management 42, 443-459
11. Gorecki, C., Nixon, J., Madill, A., Firth, J. & Brown, J. M. (2012), What influences the impact of
pressure ulcers on health-related quality of life? A qualitative patient-focused exploration of
contributory factors. Journal of Tissue Viability 21, 3-12.
12. Pressure ulcers: A Population Health Issue Fact sheet 2019
https://ewma.org/fileadmin/user_upload/Pressure_ulcers_and_patient_safety_Fact_sheet_Fi
nal_6_Nov_2019_FINAL_proofRead.pdf
13. Slawomirski, L., A. Auraaen and N. Klazinga (2017), "The economics of patient safety:
Strengthening a value-based approach to reducing patient harm at national level", OECD
Health Working Papers, No. 96, OECD Publishing, Paris,
14. Gillespie P, Carter L, McIntosh C, Gethin G. (2019), Estimating the health-care costs of wound
care in Ireland. Journl of Wound Care. Jun 2;28(6):324-330
15. Lozano, R., Naghavi, M. & et al. (2010).Global and regional mortality from 235 causes of death
for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease
Study 2010. The Lancet 380, 2095-2128
16. Gray, M., Black, J. M., Baharestani, M. M., Bliss, D. Z., Colwell, J. C., Goldberg, M., Kennedy-
Evans, K. L., Logan, S. and Ratliff, C. R. (2011). Moisture-associated skin damage: overview and
pathophysiology. J Wound Ostomy Continence Nurs, 38, 233-41.
17. Moore ZEH, Patton D. (2019), Risk assessment tools for the prevention of pressure ulcers.
Cochrane Database of Systematic Reviews, 1. Art. No.: CD006471.
18. Gibbons W, Shanks HT, Kleinhelter P, Jones P., (2006), Eliminating facility-acquired pressure
ulcers at Ascension Health Jt Comm J Qual Patient Saf. Sep;32(9):488-96.
19. Anderson M, Finch Guthrie P, Kraft W, Reicks P, Skay C, Beal AL, et al. (2015), Universal
pressure ulcer prevention bundle with WOC nurse support. J Wound Ostomy Continence Nurs;
42(3):217e25
QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 23
20. Chaboyer W, Bucknall T, Webster J, McInnes E, Gillespie BM, Banks M, et al. (2016), The effect
of a patient centred care bundle intervention on pressure ulcer incidence (INTACT): A cluster
randomised trial. Int J Nurs Stud. 64:63-71.
21. Tayyib N, Coyer F, Lewis PA., (2016), Implementing a pressure ulcer prevention bundle in an
adult intensive care. Intensive Crit Care Nurs. 37:27-36.
Additional References:
HSE Incident Management Framework and Guidance, 2020: For the most current version of
the Incident Management Framework please access:
https://www.hse.ie/eng/about/who/nqpsd/qps-incident-management/
HSE Wound Management Guidelines (2018) available at: https://healthservice.hse.ie/about-
us/onmsd/quality-nursing-and-midwifery-care/hse-national-wound-guidelines-2018.html
National HSE Open Disclosure Guidelines, available at
https://www.hse.ie/eng/about/who/nqpsd/qps-incident-management/open-
disclosure/national-open-disclosure-policy-and-guidelines.html
HSE Patient Safety Strategy (2019-2024) https://www.hse.ie/eng/about/who/nqpsd/patient-
safety-strategy-2019-2024.pdf

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 24
Definition: “A pressure ulcer is a localised injury to the skin and / or underlying tissue usually over a bony prominence, as a result of
pressure, or pressure in combination with shear. A number of contributing or confounding factors are also associated with pressure
ulcers; the significance has yet to be elucidated”
Category / Stage I
Category/Stage II
Category/Stage III
Category/Stage IV
Suspected deep pressure and shear induced tissue damage, depth unknown
25
Reference: HSE National Wound Management Guidelines available at: https://healthservice.hse.ie/about-
us/onmsd/quality-nursing-and-midwifery-care/hse-national-wound-guidelines-2018.html
Appendix 1. HSE Pressure Ulcer Category/Staging System Recommendation
25
Category/ Stage I: Intact skin with non – blanchable redness of a localised area
usually over a bony prominence. Discolouration of the skin, warmth, oedema,
hardness or pain may also be present. Darkly pigmented skin may not have
visible blanching. The area may be painful, firm, soft, warmer or cooler as
compared to adjacent skin. (EPUAP 2009)
.
Category / Stage II: Partial thickness skin loss of dermis presenting as a
shallow ulcer with a red pink wound bed, without slough. May present as an
intact or open/ ruptured serum filled blister filled with serous or sero-sanginous
fluid. Presents as a shiny or dry shallow ulcer without slough or bruising.
(EPUAP 2009).
Category / Stage III: Full thickness skin loss. Subcutaneous fat may be visible
but bone, tendon or muscles are not exposed. Slough may be present but does
not obscure the depth of tissue loss. The stage may include undermining or
tunnelling (EPUAP 2009).
Category / Stage IV: Full thickness tissue loss with exposed bone, tendon or
muscle. Slough or eschar may be present. This stage often includes undermining
and tunnelling. Exposed bone / muscle is visible or directly palpable (EPUAP
2009).
In individuals with non-blanchable redness and purple/maroon discoloration of
intact skin combined with a history of prolonged, unrelieved pressure/shear,
this skin change may be an indication of emerging, more severe pressure
ulceration i.e. an emerging Category/Stage III or IV Pressure Ulcer. Clear
recording of the exact nature of the visible skin changes, including recording
of the risk that these changes may be an indication of emerging more severe
pressure ulceration, should be documented in the patients’ health record.
These observations should be recorded in tandem with information pertaining
to the patient history of prolonged, unrelieved pressure/shear.
It is estimated that it could take 3-10 days from the initial insult causing the
damage, to become a Category/Stage III or IV Pressure Ulcer (Black et al,
2015).
.
Stable eschar (dry adherent, intact without erythema or fluctuance) on the heel serves as the
body’s biological cover and should not be removed. It should be documented as at least
Category / Stage III until proven otherwise.

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 27
Appendix 3 Pressure Ulcer Preliminary Assessment to Assist Review
Decision Making
26
Part A, Case report: To be completed in advance of the SIMT/Review Decision Making
Meeting.
To be completed in the event of a Stage III/ IV facility/community acquired Pressure Ulcer or any
other stage of Pressure Ulcer that results in a Category 1 Incident
26
link to template available at https://www.hse.ie/eng/about/who/nqpsd/qps-incident-management/incident-
management/incident-management.html
Section 1: Details of Service User
(affix service user label to a copy of this form for retention in healthcare record)
NIMS Reference No:
Date entered on NIMS:
Date notified to SAO/LAO:
Date of SIMT/ QPS meeting:
Medical History (brief summary)
Location of service:
Ward/Unit/Care Setting:
Date of Admission/First Contact:
MRN: (if applicable)
Treating Consultant /GP
Reason for admission/First Contact:
Any other relevant details:
SECTION 2: PRESSURE ULCER DETAILS
Date of first observation of Pressure Ulcer(s):
Total number Stage III Pressure Ulcers present:
Total number Stage IV Pressure Ulcers present:
Tick the specific anatomical site(s) AND state category/stage of each pressure ulcer at each site:
Sacrum
Left
Buttock
Left
Hip
Ears
Other
Left
heel
Right
Buttock
Right
Hip
Other (state site):
Right
heel
Scalp
Spine
Actions Taken by the Service since the Pressure Ulcer was identified and prior to this review:
Detail engagement with the Service User since the identification of
the Pressure Ulcer and prior to the review:
Process
Tick if Yes
Open Disclosure?
Date of Open Disclosure
Designated Support Person identified for
Service User?
Name:

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 28
SECTION 3: ISSUES RELATING TO THE SERVICE USER
Did the Service User have any of the following risk factors for pressure ulcer development
prior to the initial observation of the pressure ulcer?
Yes
No
Sensory impairment (neurological disease resulting in reduced sensation and insensitivity to
pain
Reduced level of consciousness
Deterioration in Service User’s condition whereby the Service User may have been
hypotensive, hypothermic, hypoxic, pyrexia, septic etc.
Has the Service User had a period of prolonged collapse / injury / immobilisation prior to
presentation to hospital which may correlate with presentation of tissue damage?
Severe chronic or terminal illness (multi-organ failure, poor perfusion and immobility)
Previous history of a pressure ulcer at site of current pressure ulcer ulceration
Diagnosed or suspected Peripheral Vascular Disease
Sustained pressure from medical related device e.g. from orthopaedic casting, tubing etc.
Was the Service User a) fully mobile, b) limited movement dependant on others, c) bed
bound d) chair bound?
Enter a, b, c or d
Yes
No
N/a
Has the Service User had a period of prolonged collapse/injury/immobilisation which may
correlate with presentation of tissue damage?
Is the Service User unable to maintain position?
Has the Service User declined repositioning?
Is the Service User unable to be repositioned satisfactorily due to medical condition e.g.
fractures, respiratory disease, spinal precautions, pain etc.?
Was the Service User a) fully continent, b) urinary incontinence only, c) urine and faecal
incontinence or d) catheterised and faecal incontinence?
Enter a, b, c or d
Yes
No
Does the Service User have Moisture Associated Skin Damage?
Has the Service User a body weight BMI <20 or BMI > 35?
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required:
SECTION 4: ISSUES RELATING TO THE ENVIRONMENT & EQUIPMENT
Was all equipment identified as required to prevent pressure ulcer prevention available and in use?
Equipment
Indicated
Type
Date Ordered
Date Available
In use at time
PU identified?
Yes
No
Yes
No
Mattress
Cushion
Heel
Protectors
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required.

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 29
SECTION 5: ISSUES RELATING TO STAFFING
What is the approved staffing and skill mix on the
ward/unit? (applicable to hospitals and
residential units only)
Nurse: Enter No.
HCA: Enter No.
Student: Enter No.
If a hospital/residential unit, what is the bed capacity for the ward/unit?
Select
Have there been any issues in relation to staffing/skill mix in the past week that have
impacted on the provision of pressure ulcer prevention interventions required by this
Service User?
Yes
No
If Yes, please detail:
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required:
SECTION 6: ISSUES RELATING TO TASK & TEAM
A. TASK FACTORS
Yes
No
Is there documented evidence that skin was inspected within 6 hours of presentation to
Emergency Department, admission to the ward or on first community visit?
Was a pressure ulcer risk assessment carried out within 6 hours of presentation to the Emergency
Department, admission to the ward or on first community home visit?
What risk assessment scoring system was used e.g. Waterlow, Braden/Other?
Enter Name
What was the pressure ulcer risk assessment score on admission?
Enter Score
Yes
No
Was there evidence of on-going pressure ulcer risk assessment prior to the development of the
pressure ulcer?
What was the pressure ulcer risk assessment score on the date the pressure
ulcer was identified?
Enter Score
Yes
No
Was there evidence that a pressure ulcer prevention plan was in place (e.g. SSKIN bundle or
specific pressure ulcer care plan?
Is there evidence that the pressure ulcer prevention plan in place (e.g. SSKIN bundle or specific
pressure ulcer care plan) was completed in full as appropriate to the date the Service User was
assessed as ‘at risk’?
Was the frequency of skin inspection stated on the care plan?
Was a wound assessment chart documenting the pressure ulcer assessment and management
plan completed?
What date was the first identification of skin damage documented in the
nursing notes?
Enter date
Yes
No
N/A
Has the Service User been > 2 hours in Theatre up to 6 days prior to identification of the
pressure ulcer?
Was there evidence of on-going pressure ulcer risk assessment prior to the development of
the pressure ulcer?
If the Service User was dependant, was there evidence of a written repositioning schedule
when the Service User was sitting/in bed?
Was the frequency of repositioning appropriate to the risk identified?
If the Service User was incontinent, had the Service User an Elimination Care Plan in place?
If the Service User was incontinent Is there evidence that a skin cleanser and skin barrier
protector were used as part of the skin care regimen?

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 30
Did the Service User have a nutritional risk assessment?
Date nutritional risk assessment carried out:
Enter date
Yes
No
N/A
If indicated from the nutritional risk assessment has the Service User been offered nutritional
support (such as fortified diet advice or supplements)?
Was Service User/carer information in relation to pressure ulcer prevention provided?
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required:
B. TEAM FACTORS
Yes
No
N/A
If available, was the TVN involved in the pressure ulcer management plan?
Is there evidence that the medical team / GP were aware of the Service User’s elevated risk
status for pressure damage/developing skin damage?
If the Service User had reduced mobility were they referred to physiotherapy for additional
advice or mobility rehabilitation?
If the Service User had nutritional or feeding needs identified were they referred to the
Dietician/ Speech & Language Therapist for additional advice / support?
If the Service User was identified as requiring specialist advice for seating/equipment were
they referred to the Occupational Therapist?
Was there evidence that the Service User’s family/carers were involved in the care plan and
agreed with it? (Note: as appropriate and with appropriate Service User’s consent)
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required:
SECTION 7: ISSUES RELATING TO POLICIES AND PROCEDURES
Yes
No
Does the service have local a pressure ulcer prevention policy or equivalent in place?
If yes, is this accessible to all relevant staff?
Is this policy in line with current National Wound Care Guidelines?
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required:
SECTION 8: ISSUES RELATING TO STAFF TRAINING AND EDUCATION
Yes
No
Is there evidence that all staff providing care in the ward/unit/home been trained in the
pressure ulcer prevention polices of the service?
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required:

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 31
(Note Sections 2 – 9 of this Preliminary Assessment Form may be used as Part 1 of the Review
Report if a decision is made to undertake a Concise Review of the Pressure Ulcer)
SECTION 9: ISSUES RELATING TO COMMUNICATION
Yes
No
Is there documented evidence that the Service User’s pressure ulcer risk was communicated
to the Service User?
Is there documented evidence that the Service User’s pressure ulcer risk was communicated
to relevant staff?
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required:
Preliminary Assessment Form completed by:
Date:

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 32
Part B – Record of Decision (to be completed at the SIMT/Review Decision
Making Meeting.
The decision to commission a CONCISE REVIEW or a COMPREHENSIVE REVIEW should be considered in the
event of CATEGORY 1 or CATEGORY 2 harm pressure ulcer incidents. Part A of this form seeks to identify
whether or not the key elements required for pressure ulcer prevention were in place. Part A should
therefore be considered in making the decision to conduct a review or to decide if a review is not
required.
Consideration therefore should be given to whether the case report indicates that one or more of the
following issues might pertain:
Failure to adequately or consistently apply one or more of the following interventions increased the
likelihood that the service user would develop a pressure ulcer:
evaluate the Service User’s clinical condition and pressure ulcer risk factors and/or
plan and implement interventions that are consistent with the Service User’s needs and goals, and
recognised standards of practice and/or
monitor and evaluate the impact of the interventions or revise the interventions as appropriate.
In cases where all key elements were in place and the pressure ulcer occurred despite this, it may indicate
the pressure ulcer was not preventable and that a review is not required.
RECORD OF DECISION TO CONDUCT A REVIEW
27
Document on NIMS the decision to review the incident and as the incident review progresses, update all fields on the NIMS
Review Screen to capture and track the management of the incident.
Incident Details
NIMS Ref No:
Date of Incident:
Date Notified to SAO/LAO:
Date entered on NIMS:
Date of SIMT /Relevant Meeting:
Case Officer/ QPS Manager:
Section A. Decision to Conduct a Review under the Incident Management Framework
Please indicate the decision in relation to the level of review to be conducted
27
:
Comprehensive Review
If a Comprehensive Review is selected please proceed to
Section C of this form
Concise Review
If a Concise Review is selected please proceed to Section C
of this form
No Review *
If No Review is selected please proceed to Section B of this
form

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 27
Section C.
Comprehensive Review
If the decision is to commission a Comprehensive Review, this will be by way of a Review Team
Approach and the Systems Analysis review Report Template as detailed in the HSE Incident
Management Framework is utilised.
The Final Report of the Comprehensive Review must be accepted by the SAO within 125 days of
identification of the incident.
Concise Review
If the decision is to commission a Concise Review, please complete the Pressure Ulcer Review
Report Template
The Final Report of the Concise Review must be accepted by the SAO/Local Accountable Officer (as
appropriate to incident categorisation) within 125 days of identification of the incident.
Section B. No Review
If the decision is NOT to commission a Comprehensive Review or Concise Review, please set out
below the reason or rationale for this decision and the evidence upon which it was based:
* Decisions not to review must be:
Communicated to persons affected i.e. Service User and staff.
Submitted for review and ratification by the Quality & Safety Committee, along with Part A
Complete NIMS Review Screens and this should include the reason and rationale for no
further review.
These incidents should be included in an Aggregate Review process.
Sign Off: (as applicable to the level of review chosen)
Name of SAO/LAO:
Signature of SAO/LAO:
Date:
Ratification by QPS Committee (or equivalent)
Having reviewed the Preliminary Assessment and discussed the incident the QPS Committee
agrees/disagrees (circle as appropriate) with the recommendation that No Review is required.
Name of Chair:
Signature of Chair:
Date:
In cases where the QPS Committee feels that a review is required the case is referred back to the
SAO (Category 1 incidents) or LAO (Category 2 incidents) for commissioning.

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 28
Terms of Reference
Please include at a minimum detail of the purpose and scope of the review and that it will adhere to
the principles of natural justice and fair procedures e.g.
That the purpose of the review is to identify what happened, why it happened and to identify
recommendations to reduce the risk of recurrence.
The scope of the review i.e. from X time e.g. admission to Y time e.g. time pressure ulcer
identified or from the point where the skin was last intact to the point that the pressure ulcer
was identified.
That the process will adhere to the principles of natural justice and fair procedures
Composition of the Review Team
Whilst it is not necessary to identify by name members of the Review Team at this stage the
composition by title/profession should be listed here
Contacts in relation to the review process.
Commissioner of the Review
Name
Title
Email
Telephone
Service User Designated Support Person
Name
Title
Email
Telephone
Staff Liaison
Name
Title
Email
Telephone
28
Once these are established. See https://healthservice.hse.ie/staff/news/latest-updates-on-regional-health-areas-in-the-hse/
Level of Independence attaching to the Review
Please
Tick
1. Team internal to the ward/department/ NAS Operational Region
2. Team internal to the service/hospital/NAS Operational Area
3. Team external to the service/hospital but internal to the CHO/HG/NAS Corporate
Area/ Regional Health Area
28
4. Team external to the CHO/HG/NAS Directorate/ Regional Health Area
QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 29
Appendix 4. Conducting a Concise Review Guidance
Responsibility to Review
The primary responsibility for commissioning a review is as follows;
1. Category 1 incidents - the Senior Accountable Officer
2. Category 2 incidents – the Local Accountable Officer i.e. the manager of the service in which the
pressure ulcer occurred.
QPS or Tissue Viability staff (or equivalent) may be consulted with in relation to advice on the review
process
Terms of Reference
The terms of reference should have been set out in the Preliminary Assessment to Assist Review Decision
Making Form – Part B – Record of Decision.
Who Should Be Involved?
The review should seek the involvement of relevant staff i.e. those on duty at the time the pressure
ulcer was identified, the line manager in the relevant area and the Service User.
The Service User should be contacted to advise them of the plan for review and to ask them if there are
any specific issues that they would like to see addressed by the review. This engagement also provides
an opportunity to clarify the purpose of the review, the likely timeframe for completion and how they
will be advised of the outcome.
In relation to staff whilst there is no requirement to conduct formal interviews it is important to engage
with staff to understand their involvement and gain their perspective. This can be done on a one to one
basis or by way of a multidisciplinary meeting.
If engaging on a multidisciplinary basis it is important to facilitate this in a way which focuses on
learning. To ensure that the process is open and participative the following ground rules should be set
at the outset: everyone’s perspective is valued (regardless of their grade/profession); it is not about
blame or finger pointing; and the focus is on understanding why the pressure ulcer occurred and what
can be learned in order to prevent any further deterioration of the pressure ulcer identified and to
prevent any further pressure ulcers occurring to this Service User or other Service Users.
The Report
The template for the report is set out below and this should be used in all circumstances and completed
in full. This is important so that services can conduct an aggregate analysis of their concise reports to
identify further learning.
Much of the template reflects information gathered in the completion of the Preliminary Assessment to
Assist Review Decision Making Form Part A earlier in the process. The blank template is 6 pages long
and it is anticipated that a concise report when complete should not exceed 10 pages.

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 30
The review report is divided into the following 14 sections. It is recommended that you print off this
table when drafting the report as it will serve as a guide to completion.
Section
Detail to be included
1. Introduction
This section should include information about the services commitment to
quality and how the learning from this review will inform safety
improvement. It should also contain detail of the approach to review used,
the information considered, and the source of this information e.g.
healthcare record, discussion with key staff etc. Detail of the disclosure of
the pressure ulcer and the apology provided to the Service User should be
included here.
2. Details of Service
User and Pressure
Ulcer
Concise details of the Service User’s background i.e. when and why they
were admitted and brief detail of their medical and social history.
Description of the pressure ulcer i.e. its location, category/stage should be
included and detail of immediate actions taken following its identification.
The section on involvement of the Service User relates to the period
following identification of the pressure ulcer.
3. Issues relating to
the Service User
Service User related issues are listed in this section.
Management of Service User risk factors are a key to pressure ulcer
prevention and particular emphasis should be given to this section.
Having answered the questions, consider any areas identified where
improvement is required and list these. This will assist you when it comes
identifying contributory factors and incidental findings and to making
recommendations.
4. Issues relating to
Environment &
Equipment
Environment & equipment related issues are listed in this section.
The identification and timely supply of equipment identified as required is
key to prevent pressure ulcers. High risk Service Users can develop pressure
ulcers quickly if the correct equipment is not available and utilised
appropriately.
Having answered the questions, consider any areas identified where
improvement is required and list these. This will assist you when it comes
identifying contributory factors and incidental findings and to making
recommendations.
5. Issues relating to
Staffing
Staffing related issues are listed in this section.
Having answered the questions, consider any areas identified where
improvement is required and list these. This will assist you when it comes
identifying contributory factors and incidental findings and to making
recommendations.
6. Issues relating to
Task and Team
Task and team related issues are listed in this section.
The prevention of pressure ulcers is optimal when staff work as a team to
ensure that all tasks required are undertaken in a consistent and complete
manner.
Having answered the questions, consider any areas identified where
improvement is required and list these. This will assist you when it comes

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 31
identifying contributory factors and incidental findings and to making
recommendations.
7. Issues relating to
Policies and
Procedures
Policy and Procedure related issues are listed in this section.
Pressure ulcer prevention must be underpinned by robust policy which is
based on best practice, available, workable and in routine use.
Having answered the questions, consider any areas identified where
improvement is required and list these. This will assist you when it comes to
identifying contributory factors and incidental findings and to making
recommendations.
8. Issues relating to
Staff Training and
Education
Staff training and education related issues are listed in this section.
Though a service may have the relevant policies and procedures in place,
staff training and education is essential if these are to underpin practice.
Having answered the questions, consider any areas identified where
improvement is required and list these. This will assist you when it comes
identifying contributory factors and incidental findings and to making
recommendations.
9. Issues relating to
Communication
Communication related issues are listed in this section.
Communication is vital and it is essential that all those caring for the Service
User are aware of their risk of developing a pressure ulcer. Communication
can be achieved at handovers of care, through signage and other means.
Having answered the questions, consider any areas identified where
improvement is required and list these. This will assist you when it comes
identifying contributory factors and incidental findings and to making
recommendations.
10. Statement of
Findings
Statements which describe the relationships between the contributing
factors and the incident and/or outcome.
In relation to pressure ulcers, the Statement of Findings relates to that
outlined below.
Failure to adequately or consistently apply one or more of the following
interventions increased the likelihood that the service user would develop a
pressure ulcer:
evaluate the Service User’s clinical condition and pressure ulcer risk
factors and/or
plan and implement interventions that are consistent with the
Service User’s needs and goals, and recognised standards of practice
and/or
monitor and evaluate the impact of the interventions or revise the
interventions as appropriate.
Depending on the information gathered so far in the review, amend the
above Statement of Findings as appropriate to the case e.g. if it was that
there was good evidence that the Service User’s clinical condition and
pressure ulcer risk factors were evaluated but the planning, implementation

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 32
and monitoring of interventions were in deficit then you could delete the
first bullet point.
If a Service User has many risk factors and all preventative measures were in
place it may be that there was no Statement of Findings i.e. that the
pressure ulcer was not preventable. That does not mean that learning
cannot take place and improvements made to the care of other Service
Users.
11. Contributory
Factors
These should link to the Statement of Findings. As part of the completion of
the sections relating to issues (3 – 9 above) you will have identified issues
relating to the prevention of pressure ulcers. These may have either been
contributory or incidental to the development of the pressure ulcer.
Contributory factors are defined as a circumstance, action of influence
which it is thought to have played a part in the origin or development of the
pressure ulcer or to increase the risk of development of the pressure ulcer.
List these here starting with the issue e.g.
Task – That the Service User, though having had a nutritional risk assessment,
was not provided with the nutritional supports required.
12. Incidental Findings
These are areas identified in the course of the review, as requiring
improvement but did not cause or contribute to the incident.
13. Notable Practice
The inclusion of notable practice is important in providing balance to the
report as they highlight positive aspects of the service. Points such as how
the service responded to the Service User and managed the pressure ulcer
at the time of identification can be included here. Consider also including
detail of any immediate actions put in place within the service to prevent a
similar event occurring to other Service Users.
14. Other Issues of
Note
These should include detail of the response to any queries raised by the
family/carers at the outset of the review that are not dealt with in the
above report.
15. Review Outcome
Pick one of the following outcomes and enter it in section 11 of the report.
Appropriate care and/or service (Good/Notable Practice)
Well planned and delivered, unpreventable outcome and no Statement
of Findings identified.
Indirect system of care/service issues
No Statement of Findings identified but Incidental Findings were
identified i.e. improvement lessons can be learned but these were
unlikely to have affected the outcome.
Minor system of care/service issues
A different plan and/or delivery of care may have resulted in a different
outcome. For example, systemic factors were identified although there
was uncertainty regarding the degree to which these impacted on the
outcome.
Major system of care/service issues
A different plan and/or delivery of care would, on the balance of
probability, have been expected to result in a more favourable
outcome. For example, systemic factors were considered to have an
adverse and causal influence on the outcome.

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 33
16. Recommendations
Recommendations must be linked to the Statement of Findings and
Contributory Factors as they aim to reduce the risk of pressure ulcers
occurring to this or other Service Users. This is linked to the purpose set out
in the Introduction i.e. improving safety and preventing harm to others.
17. Arrangements for
Shared Learning
Consider how you will share the learning from this review to;
Staff within the ward where the pressure ulcer occurred
Staff within the hospital/residential unit where the pressure ulcer
developed
Within the CHO/HG e.g. through the relevant Quality and Safety
Committee (or equivalent) and have it included in an aggregate
review of pressure ulcer incidents.
18. Sign off
Prior to completion of this section the draft report should be considered in
the context of the Governance Approval Process for Final Draft Reports
(please refer to Section 16 of the HSE Incident Management Framework).
It is the responsibility of the Commissioner of the report to ensure that the
above consideration is carried out.
The draft report is then submitted to the Commissioner.
Based on a satisfactory review of the report and its acceptance by the
Commissioner, the report is then considered final.
Completed reports must be uploaded onto NIMS. Review screens on NIMS
must be completed at this stage as the availability of this summary
information is important to assist with aggregate analysis.

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 34
Appendix 5. Pressure Ulcer Review Report Template
PRESSURE ULCER INCIDENT REVIEW REPORT
29
CONFIDENTIAL
Date of Incident
NIMS Reference Number
Acute Hospital/Community Service
Review Commissioner
Lead Reviewer
Date Report Completed
Date Report uploaded on NIMS
Note: Part 1, Sections 2-9 are identical to the Preliminary Assessment Form and therefore,
these sections from the PAF may be inserted in to this template and updated if further
information has come to light since the SIMT meeting.
To complete the Concise Review of the Pressure Ulcer, Part 2 of this template must be
completed to identify the Findings, Contributory Factors, Recommendations and Shared
Learning.
29
link to template available at https://www.hse.ie/eng/about/who/nqpsd/qps-incident-management/incident-
management/incident-management.html
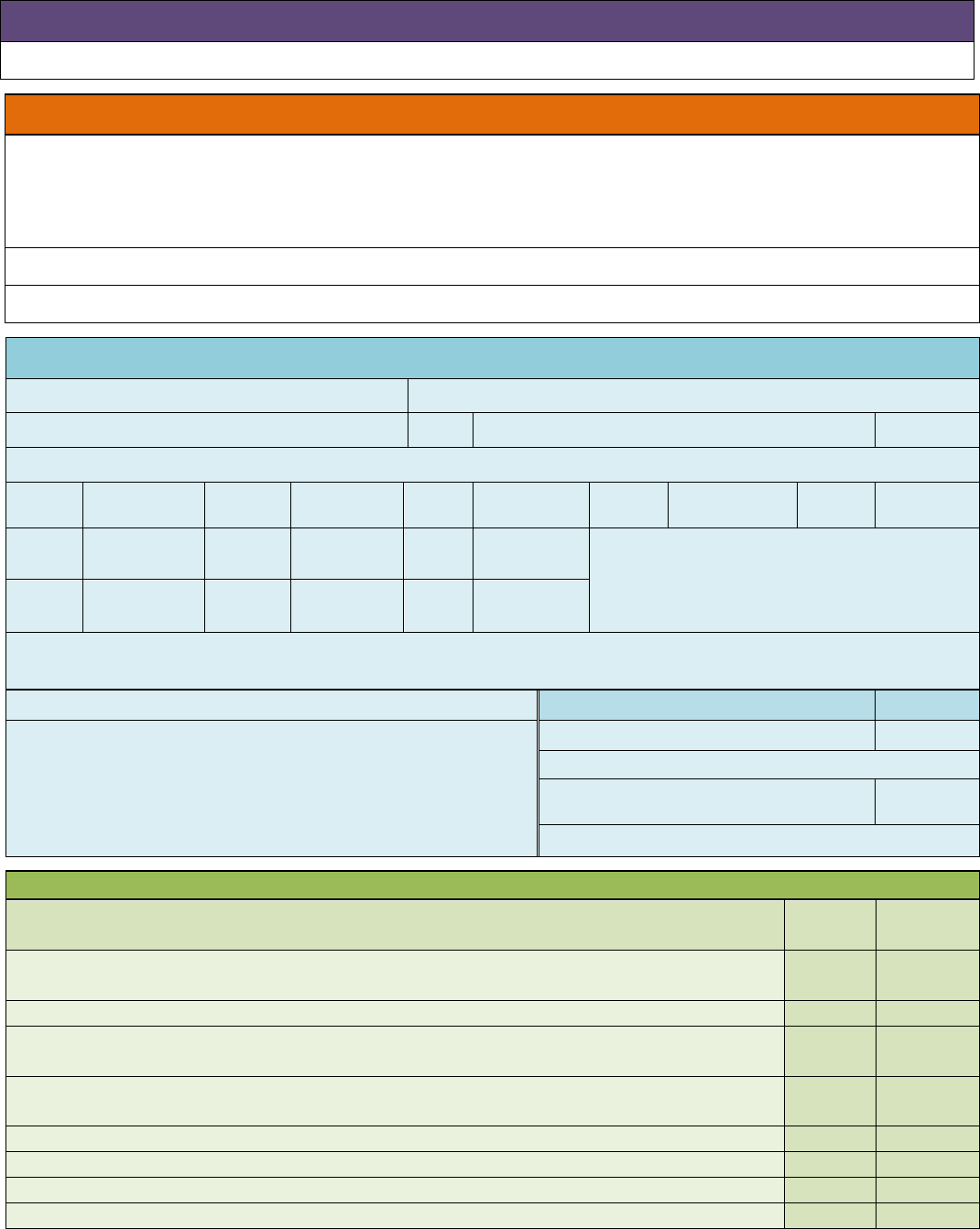
QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 35
Review Report Part 1
INTRODUCTION
Click here to enter text.
SECTION 1: DETAILS OF SERVICE USER
Background
Click here to enter text.
Reason for Admission/Referral:
Date and details of Admission/ First Contact:
SECTION 2: PRESSURE ULCER DETAILS
Date of first observation of Pressure Ulcer(s):
Total number Stage III Pressure Ulcers present:
Total number Stage IV Pressure Ulcers present:
Tick the specific anatomical site(s) AND state category/stage of each pressure ulcer at each site:
Sacrum
Left
Buttock
Left
Hip
Ears
Other
Left
heel
Right
Buttock
Right
Hip
Other (state site):
Right
heel
Scalp
Spine
Actions Taken by the Service since the Pressure Ulcer was identified and prior to this review:
Process
Tick if Yes
Detail engagement with the Service User since the identification of
the Pressure Ulcer and prior to the review:
Open Disclosure?
Date of Open Disclosure
Designated Support Person identified for
Service User?
Name:
SECTION 3: ISSUES RELATING TO THE SERVICE USER
Did the Service User have any of the following risk factors for pressure ulcer development
prior to the initial observation of the pressure ulcer?
Yes
No
Sensory impairment (neurological disease resulting in reduced sensation and insensitivity to
pain)
Reduced level of consciousness
Deterioration in Service User’s condition whereby the Service User may have been
hypotensive, hypothermic, hypoxic, pyrexia, septic etc.
Has the Service User had a period of prolonged collapse / injury / immobilisation prior to
presentation to hospital which may correlate with presentation of tissue damage?
Severe chronic or terminal illness (multi-organ failure, poor perfusion and immobility)
Previous history of a pressure ulcer at site of current pressure ulcer ulceration
Diagnosed or suspected Peripheral Vascular Disease
Sustained pressure from medical related device e.g. from orthopaedic casting, tubing etc.

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 36
Was the Service User a) fully mobile, b) limited movement dependant on others, c) bed
bound d) chair bound?
Enter a, b, c or d
Yes
No
N/a
Has the Service User had a period of prolonged collapse/injury/immobilisation which may
correlate with presentation of tissue damage?
Is the Service User unable to maintain position?
Has the Service User declined repositioning?
Is the Service User unable to be repositioned satisfactorily due to medical condition e.g.
fractures, respiratory disease, spinal precautions, pain etc.?
Was the Service User a) fully continent, b) urinary incontinence only, c) urine and faecal
incontinence or d) catheterised and faecal incontinence?
Enter a, b, c or d
Yes
No
Does the Service User have Moisture Associated Skin Damage?
Has the Service User a body weight BMI <20 or BMI > 35?
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required:
SECTION 4: ISSUES RELATING TO THE ENVIRONMENT & EQUIPMENT
Was all equipment identified as required to prevent pressure ulcer prevention available and in use?
Equipment
Indicated
Type
Date Ordered
Date Available
In use at time PU
identified?
Yes
No
Yes
No
Mattress
Cushion
Heel
Protectors
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required.
SECTION 5: ISSUES RELATING TO STAFFING
What is the approved staffing and skill mix on the
ward/unit? (applicable to hospitals and
residential units only)
Nurse: Enter No.
HCA: Enter No.
Student: Enter No.
If a hospital/residential unit, what is the bed capacity for the ward/unit?
Select
Have there been any issues in relation to staffing/skill mix in the past week that have
impacted on the provision of pressure ulcer prevention interventions required by this
Service User?
Yes
No
If Yes, please detail:
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required:

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 37
SECTION 6: ISSUES RELATING TO TASK & TEAM
A. TASK FACTORS
Yes
No
Is there documented evidence that skin was inspected within 6 hours of presentation to
Emergency Department, admission to the ward or on first community visit?
Was a pressure ulcer risk assessment carried out within 6 hours of presentation to the Emergency
Department, admission to the ward or on first community home visit?
What risk assessment scoring system was used e.g. Waterlow, Braden/Other?
Enter Name
What was the pressure ulcer risk assessment score on admission?
Enter Score
Yes
No
Was there evidence of on-going pressure ulcer risk assessment prior to the development of the
pressure ulcer?
What was the pressure ulcer risk assessment score on the date the pressure
ulcer was identified?
Enter Score
Yes
No
Was there evidence that a pressure ulcer prevention plan was in place (e.g. SSKIN bundle or
specific pressure ulcer care plan?
Is there evidence that the pressure ulcer prevention plan in place (e.g. SSKIN bundle or specific
pressure ulcer care plan) was completed in full as appropriate to the date the Service User was
assessed as ‘at risk’?
Was the frequency of skin inspection stated on the care plan?
Was a wound assessment chart documenting the pressure ulcer assessment and management
plan completed?
What date was the first identification of skin damage documented in the
nursing notes?
Enter date
Yes
No
N/A
Has the Service User been > 2 hours in Theatre up to 6 days prior to identification of the
pressure ulcer?
Was there evidence of on-going pressure ulcer risk assessment prior to the development of
the pressure ulcer?
If the Service User was dependant, was there evidence of a written repositioning schedule
when the Service User was sitting/in bed?
Was the frequency of repositioning appropriate to the risk identified?
If the Service User was incontinent, had the Service User an Elimination Care Plan in place?
If the Service User was incontinent Is there evidence that a skin cleanser and skin barrier
protector were used as part of the skin care regimen?
Did the Service User have a nutritional risk assessment?
Date nutritional risk assessment carried out:
Enter date
Yes
No
N/A
If indicated from the nutritional risk assessment has the Service User been offered nutritional
support (such as fortified diet advice or supplements)?
Was Service User/carer information in relation to pressure ulcer prevention provided?
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required:
B. TEAM FACTORS
Yes
No
N/A
If available, was the TVN involved in the pressure ulcer management plan?

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 38
Is there evidence that the medical team / GP were aware of the Service User’s elevated risk
status for pressure damage/developing skin damage?
If the Service User had reduced mobility were they referred to physiotherapy for additional
advice or mobility rehabilitation?
If the Service User had nutritional or feeding needs identified were they referred to the
Dietician/ Speech & Language Therapist for additional advice / support?
If the Service User was identified as requiring specialist advice for seating/equipment were
they referred to the Occupational Therapist?
Was there evidence that the Service User’s family/carers were involved in the care plan and
agreed with it? (Note: as appropriate and with appropriate Service User’s consent)
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required:
SECTION 7: ISSUES RELATING TO POLICIES AND PROCEDURES
Yes
No
Does the service have local a pressure ulcer prevention policy or equivalent in place?
If yes, is this accessible to all relevant staff?
Is this policy in line with current National Wound Care Guidelines?
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required:
SECTION 8: ISSUES RELATING TO STAFF TRAINING AND EDUCATION
Yes
No
Is there evidence that all staff providing care in the ward/unit/home been trained in the
pressure ulcer prevention polices of the service?
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required:
SECTION 9: ISSUES RELATING TO COMMUNICATION
Yes
No
Is there documented evidence that the Service User’s pressure ulcer risk was communicated
to the Service User?
Is there documented evidence that the Service User’s pressure ulcer risk was communicated
to relevant staff?
Any Additional Information:
Based on the above assessment, identify any areas where improvement is required:

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 39
Review Report Part 2
SECTION 10: STATEMENT OF FINDINGS
This Statement of Finding best explains why this pressure ulcer occurred.
Failure to adequately or consistently apply one or more of the following interventions increased the likelihood that
the service user would develop a pressure ulcer:
evaluate the Service User’s clinical condition and pressure ulcer risk factors and/or
plan and implement interventions that are consistent with the Service User’s needs and goals, and
recognised standards of practice and/or
monitor and evaluate the impact of the interventions or revise the interventions as appropriate.
Note: amend the Statement of Finding as appropriate to the case being reviewed e.g. if it was that there was good
evidence that the Service User’s clinical condition and pressure ulcer risk factors were evaluated but the planning,
implementation and monitoring of interventions were in deficit then you could delete the first bullet point.
SECTION 11: CONTRIBUTORY FACTORS
The Contributory Factors that relate to the Statement of Findings (SOF) identified are as follows.
Enter Contributory Factors that relate to SOF
Enter Contributory Factors that relate to SOF
Enter Contributory Factors that relate to SOF
Enter Contributory Factors that relate to SOF
Add additional rows as required
SECTION 12: INCIDENTAL FINDINGS
These are areas identified as requiring improvement but did not cause or contribute to the incident.
Click here to enter text.
Click here to enter text.
Click here to enter text.
Click here to enter text.
Add additional rows as required
SECTION 13: NOTABLE PRACTICE
The following are points in the incident or review process where care and/or practice had an important positive
impact and may provide valuable learning opportunities
Click here to enter text.
Click here to enter text.
Add additional rows as required
SECTION 14: OTHER ISSUES OF NOTE
Click here to enter text.
SECTION 15: REVIEW OUTCOME
See guidance for detail of possible outcomes

QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 40
SECTION 16: RECOMMENDATIONS
Recommendations for improvement must be linked to the Statement of Findings and Contributory Factors
1
Click here to enter text.
2
Click here to enter text.
3
Click here to enter text.
4
Click here to enter text.
Add additional rows as required
SECTION 18: SIGN OFF
Yes
No
Were the Service User
30
and relevant Staff advised of the plan for review before beginning the
review?
Were the Service User and relevant staff provided with on-going communication and support
throughout the review?
Were Staff who participated in the process provided with the draft report and requested to provide
feedback on factual accuracy and their comments?
Was the Service User given a draft report for review and offered a meeting to discuss?
Comments:
Name SAO/LAO:
Date report accepted:
30
Note: The term Service User is used in this document to include any persons who use health and social care service within
HSE or HSE funded services and who have developed a pressure ulcer. The term Service User also includes their appropriate
Relevant Person who has been legally assigned, or who has been nominated in writing to the health services provider, as a
person to whom clinical information in relation to the patient may be disclosed.
Relevant Persons is defined in the Civil Liability (Amendment) Act 2017 as:
“Relevant person”, in relation to a patient, means a person— (a) who is— (i) a parent, guardian, son or daughter, (ii) a spouse,
or (iii) a civil partner of the patient, (b) who is cohabiting with the patient or (c) whom the patient has nominated in writing to
the health services provider as a person to whom clinical information in relation to the patient may be disclosed.
SECTION 17: ARRANGEMENTS FOR SHARED LEARNING
Learning has been shared in the following manner
1
2
3
4
Add additional rows as required
QPSIM 004, Pressure Ulcers, A Practical Guide for Review, Revision 2, October 2022 41
Appendix 6. Membership of the Pressure Ulcer Review Guide
Development Group (2018)
Cornelia Stuart, Assistant National Director, Quality Risk and Safety, Quality Assurance and
Verification Division (Chair)
Deirdre Carey, Risk & Incident Officer, Acute Hospitals Division
Fiona Concannon, Clinical Nurse Specialist Tissue Viability and Wound Management, CHO 9
Geraldine Craig, Clinical Nurse Specialist Tissue Viability, Our Lady of Lourdes Hospital,
Drogheda
Catherine Hogan, Quality Improvement Division
Pat McCluskey, Advanced Nurse Practitioner Wound Care and Tissue Viability, Cork
University Hospital
Margaret McGarry, Risk Manager, Quality Risk and Safety, Quality Assurance and Verification
Division
Professor Zena Moore, Professor and Head of the School of Nursing and Midwifery, Royal
College of Surgeons in Ireland
Annette Ridley, Risk Advisor, University of Limerick Hospitals Group
Appendix 7. Membership of the Pressure Ulcer Review Guide Review
Group (2022)
Dr. Samantha Hughes, Incident Management Team, QPSD
Professor Zena Moore, Professor and Head of the School of Nursing and Midwifery, Royal
College of Surgeons in Ireland
Fiona Concannon, Clinical Nurse Specialist Tissue Viability and Wound Management, CHO 9
Maureen Nolan, Director of Nursing, ONMSD
Gillian O'Brien, Registered Advanced Nurse Practitioner Tissue Viability, Naas Hospital
Helen Meagher, Registered Advanced Nurse Practitioner Tissue Viability, UL Hospitals Group,
University Hospital Limerick
Thank you also to all those who participated in the consultation process, including the National
Quality and Patient Safety Teams in HSE Acute Operations and HSE Community Healthcare.
Thank you also to the QPSD Team and the QPSD Incident Management Team members who
contributed to reviewing this document.

