
This report is the product of the Allergy and Asthma Task Force
that was convened and supported by Thermo Fisher Scientific.
More information available at
allergyaidiagnostics.com
The Allergy and Asthma Task
Force Recommendations
The Practical Application of Allergic Trigger
Management to Improve Asthma Outcomes
The Need to Improve Outcomes for
People with Asthma in Primary Care and
Health Systems: Beyond Adding More
Pharmacotherapy
Barbara P. Yawn, MD, MSc, FAAFP, for the Allergy and
Asthma Task Force Members
S3
The Practical Application of Allergic Trigger
Management to Improve Asthma Outcomes
Step 1: Identify Patients with Allergic
Components of Asthma
Andrew Liu, MD; Allan Luskin, MD; Randall Brown, MD,
MPH, AE-C; Michael D. Cabana, MD, MPH; Ivor Emanuel,
MD; Len Fromer, MD, FAAFFP; Christine W. Wagner, APRN,
MSN, AE-C; Barbara P. Yawn, MD, MSc, FAAFP
S5
Integrating Allergic Trigger Management
into Primary Care Asthma Management:
Step 3: A Significant Opportunity for Payers
and Health Systems
Randall Brown, MD, MPH, AE-C; Suzanne Madison, PhD;
Len Fromer, MD, FAAFP; Brad Lucas, MD; Steve Clark;
Michael D. Cabana, MD, MPH; Christine W. Wagner, APRN,
MSN, AE-C; Barbara P. Yawn, MD, MSc, FAAFP
S25
The Practical Application of Allergic Trigger
Management to Improve Asthma Outcomes:
Step 2: Identifying and Addressing Allergen
Exposure in Daily Practice
Christine W. Wagner, APRN, MSN, AE-C; Allan Luskin, MD;
Len Fromer, MD, FAAFP; Barbara P. Yawn, MD, MSc, FAAFP;
Randall Brown, MD, MPH; Andrew Liu, MD
S14
Recommendations to Improve Asthma
Outcomes: Work Group Call to Action
Regulatory approval code: 63679.AL.US1.EN.v1.18.
allergyinsider

AUGUST 2018
Randall Brown MD, MPH, AE-C is the Director of Asthma Programs,
Center for Managing Chronic Disease, and a Clinical Assistant Pro-
fessor, Health Behavior and Health Education at the University of
Michigan. He is Co-Director, National Asthma Educator Certication
Board and leader of PACE programs internationally.
Michael D. Cabana, MD, MPH is a Professor of Pediatrics, Epide-
miology and Biostatistics, as well as a member of the core faculty at
the Philip R. Lee Institute for Health Policy Studies at the University
of California, San Francisco (UCSF). Dr. Cabana has maintained an
active presence in clinical medicine, serving as Chief of the UCSF
Division of General Pediatrics since 2005. Dr. Cabana has extensive
experience in practice-based research and has collaborated with
over 120 pediatric practices in several national randomized con-
trolled trials focused on primary care management of asthma.
Steve Clark, Sr. VP, Optum Life Sciences, has 20 years of experience
helping pharmaceutical and medical device companies in market-
ing, clinical, and reimbursement areas. He has worked with numer-
ous early-stage technologies to assess reimbursement issues and
develop strategies for assessment of market differentiation opportu-
nities. The work has included stakeholder analysis for payers, clini-
cians, and health policy analysts, as well as horizon scanning assess-
ments for market opportunity and comparative analysis.
Ivor Emanuel, MD served as a Clinical Assistant Professor in Oto-
laryngology at the University of California, San Francisco, and was
also on the clinical faculty in the Department of Otolaryngology at
Stanford University, Palo Alto, California. Dr Emanuel is a Fellow and
Past President of the AAOA. He is a Fellow of the American Acad-
emy of Otolaryngology/Head and Neck Surgery and a Member of
the ACAAI.
Len Fromer, MD, FAAFP, Executive Medical Director, Group Practice
Forum leads a team engaged in national projects with health systems
and group practices that deliver education, tools, and services to
achieve success in their clinical integration efforts. Dr. Fromer lectures
extensively on the topics of health-system reform, the patient centered
medical home and the accountable care organization. Dr. Fromer is
a Fellow of the AAFP, and a diplomat of both the American Board of
Family Practice and the National Board of Medical Examiners.
Andrew Liu, MD is a Pediatric Allergist, Director, Airway Inam-
mation Research & the Environment (AIRE) Program, Co-Director,
Asthma Clinical Research Center, The Breathing Institute, Section
of Pulmonary Medicine, Children’s Hospital of Colorado, Professor,
Department of Pediatrics, University of Colorado School of Medicine,
Adjunct Professor, Department of Pediatrics, National Jewish Health.
Alan Luskin, MD is Clinical Associate Professor of Medicine at Uni-
versity of Wisconsin and Director of the Center for Respiratory Health
at SSMHealth, President of HealthyAirways, an outcomes manage-
ment consulting group with research focusing on outcomes manage-
ment in airways diseases. He received the NIH Exemplary Service
Award for his work with the NAEPP formulating and disseminating
the National Asthma Guidelines. He is a Past Vice-President and
Distinguished Fellow of the ACAAI and received its Distinguished
Service Award.
Brad Lucas MD, MBA, FACOG is the Senior Medical Director for
Buckeye Health Plan, a subsidiary of Centene Corporation. Centene
manages care for 11 million members across 24 states. Dr. Lucas
has helped build and guide Centene’s award winning programs Start
Smart for Your Baby®, its Addiction in Pregnancy Program and pre-
term birth prevention programs. Similarly, he is responsible for the
development and implementation of programs that improve clinical
outcomes and ensure high quality care across all medical conditions
for Buckeye members. He continues to see patients at AxessPointe
Community Health Center.
Suzanne Madison, PhD holds graduate degrees in public adminis-
tration (MPA) and public health (MPH), a doctorate in public health
(community health track), and a certicate in clinical trials from Har-
vard Medical School. She has been involved in research for the
past nine years, as a participant in a clinical trial, a senior research
associate, and graduate of the Harvard Medical School, Global Clini-
cal Scholars Research Training Program. She currently serves in a
patient advocacy role with the Patient-Centered Outcomes Research
Institute (PCORI) as a member of the Patient Engagement Advisory
Panel (PEAP).
Christine Waldman Wagner APRN, MSN, AE-C has developed and
presented numerous programs for health professionals on multiple
topics including diagnosis and treatment of asthma and allergic dis-
eases, patient education, health literacy, and other related topics.
She is a founding member and rst president of the Association of
Asthma Educators and served on the rst National Asthma Educa-
tor Certication Board of Directors. She is also a trained facilitator
for Problem Based Learning and faculty associate at Texas Woman’s
University.
Barbara P. Yawn, MD, MSc FAAFP, is a family physician researcher
who currently focuses on respiratory diseases, specically COPD
screening/case nding and implementation of new tools to improve
asthma outcomes. She is/was a member of the International Pri-
mary Care Respiratory Group; EPR-3 science panel, editor in chief
of Respiratory Medicine Case Reviews and the COPD Foundation
Research Committee. She is retired from her position as the director
of research at the Olmsted Medical Center, is an Adjunct Professor
of Family and Community Health at the University of Minnesota and
serves as a consultant to multiple NIH and PCORI funded studies of
asthma and COPD.
[
AFFILIATIONS
]
S2
SEPTEMBER 2018
S3
AUGUST 2018
The Need to Improve Outcomes for People
with Asthma in Primary Care and Health
Systems: Beyond Adding More
Pharmacotherapy
Barbara P. Yawn, MD, MSc, FAAFP, for the Allergy and Asthma Task Force Members
DISCLOSURES
Dr. Yawn is a paid consultant and has an ongoing relationship with
Thermo Fisher Scientic.
ACKNOWLEDGEMENT
The Task Force appreciates the editorial support provided
by Sarah Staples, whose work was nancially supported by
Thermo Fisher Scientic. The Task Force also acknowledges and
appreciates the important logistical support provided by Kevin H.
TenBrink and Gabriel Ortiz of Thermo Fisher Scientic.
is supplement is the product of the Allergy and Asthma Task
Force convened and supported by ermo Fisher Scientic.
e Task Force met in person and remotely over a period of
20 months to develop and publish its recommendations to
identify which patients with asthma are of highest priority for
allergy evaluation, how that evaluation could be done, and
how allergy evaluation can be incorporated into primary care.
e expertise in the Task Force includes: primary care
(family medicine and pediatrics); specialists in allergy and
pulmonology, nursing, respiratory therapy, asthma educa-
tion, laboratory medicine, and health systems design; and
LEARNING OBJECTIVES
What this supplement addresses:
• Asthma inammation and the role of aeroallergen sen-
sitization in asthma burden
• The groups of people with asthma who are most likely to
benet from evaluation for allergen sensitization
• A practical approach to identifying and caring for those
subpopulations who shoulder disproportionate allergy
and asthma risk and morbidity
• The 2 readily available methods to assess specic al-
lergen sensitization
• Ways to include allergen evaluation in daily primary care
practice
• Potential solutions for the common barriers to patient
education regarding trigger avoidance and management
• The role of health systems and payers and the busi-
ness case for supporting and integrating allergen evalu-
ation and trigger avoidance education in primary care
practices.
the perspectives of quality experts, medical directors, and
patients. Members’ travel expenses were covered by the spon-
sor, as was the editorial support of Sarah Staples.
Task Force members (in alphabetical order) are: Randall
Brown MD, MPH, AE-C; Michael D. Cabana, MD, MPH; Steve
Clark; Ivor Emanuel, MD; Len Fromer, MD, FAAFP; Andrew
Liu, MD; Brad Lucas, MD; Allan Luskin, MD; Suzanne Madi-
son, PhD; and Christine W. Wagner, APRN, MSN, AE-C. Task
Force Chair is Barbara Yawn, MD, MSc, FAAFP.
A
sthma is a common and increasingly prevalent
chronic respiratory condition that aected 25 mil-
lion Americans in the United States in 2007.
1
Most
people with asthma receive their asthma care within pri-
mary care practices.
2
People with asthma and their families
continue to experience signicant asthma-related disease
burden, with over 10.5 million oce visits a year, most of
which are unscheduled and in primary care oces.
1,2
ese
visits often focus on dealing with acute symptoms or exac-
erbations, with little time and attention available for pre-
vention of the next exacerbation and the daily ongoing bur-
den of asthma symptoms.
Added to unscheduled oce visits, 3 of every 5 children
with asthma
3
and more than half of working adults with
asthma
4
have their life disrupted by the need to seek urgent
or emergency care for their asthma each year.
5
Asthma is
the reason for over 1.8 million emergency department (ED)
visits and more than 400,000 hospitalizations each year.
5
About 10% of people with asthma have severe asthma,
resulting in several urgent care and emergency care visits
and a high risk of asthma-related hospitalization, in addi-
tion to missed school, work and activity days.
6-8
Much of this burden is potentially preventable. How-
ever, several studies have demonstrated that this continu-
ing asthma burden is not simply a need to prescribe more
inhaled corticosteroids and bronchodilators.
9
Other factors
must be considered, including triggers, medication adher-
ence, and comorbid conditions.
10
Most people with asthma
S3
SEPTEMBER 2018

S4
SEPTEMBER 2018
[
INTRODUCTION
]
have hypersensitivity that includes “allergic” reactions to
environmental exposures. Such environmental exposures
are common, with over 90% of homes having at least 3 detect-
able common aeroallergens and 73% having 1 or more at an
elevated level.
11
e presence of an allergen in the home will
not trigger asthma symptoms or exacerbations in a person
without sensitization to that allergen. e study authors con-
rmed that in many sensitized people, the presence of com-
mon allergens at home is associated with increased asthma
burden.
ASTHMA IS NOT WELL-CONTROLLED FOR
MOST PRIMARY CARE PATIENTS
In a recent study of over 1200 family medicine patients with
asthma, 56% of children, 52% of adolescents, and 63% of
adults had uncontrolled asthma, with over 20% making 1 or
more visits to the ED or hospital in the previous 6 months.
12
Several studies conrm that most Americans with asthma
continue to have suboptimal control of symptoms, periodic
asthma exacerbations, or both.
7,13,14
Widely disseminated
asthma-treatment guidelines are available, along with a
variety of generally eective pharmacotherapies.
15,16
ose
guidelines highlight the need to supplement existing phar-
macotherapy with attention to triggers that include irritants
and allergens.
WHAT ARE NEXT STEPS IN DECREASING
ASTHMA BURDEN?
Asthma is a condition of hypersensitivity to common expo-
sures, associated with chronic airway inammation, hyper-
reactivity, congestion, and airow restriction. Whereas
symptoms come and go, inammation and hyperreactivity
of airways are chronic and may be associated with persistent
narrowing of the airways, even when the person “feels well.”
For most people with asthma, that inammation is triggered
or maintained by exposure to allergens to which they are
sensitized. It is the need to address the sensitization to those
allergens that is the basis for this supplement. l
REFERENCES
1. Centers for Disease Control (CDC). https://www.cdc.gov/asthma/most recent data.
htm. Accessed 13 July 2018.
2. Kwong KYC, Eghrari-Sabet JS, Mendoza GR, et al. e benets of specic immuno-
globulin E testing in the primary care setting. Am Manage Care. 2011;17:S447-S459.
3. Federal Interagency Forum on Child and Family Statistics. Indicators of Well-Being.
Washington, DC: Federal Interagency Forum; 2012.
4. Mazurek JM, Syamlal G. Prevalence of Asthma, Asthma Attacks, and Emergency
Department Visits for Asthma Among Working Adults - National Health Interview
Survey, 2011-2016. MMWR. 2018;67(13):377-386.
5. Fuhlbrigge A, Reed ML, Stempel DA, Ortega HO, Fanning K, Stanford RH. e sta-
tus of asthma control in the U.S. adult population. Allergy Asthma Proc. 2009;30(5):
529-533.
6. Rank MA, Wollan P, Li JT, Yawn BP. Trigger recognition and management in poorly
controlled asthmatics. Allergy Asthma Proc. 2010;31(6):99-105.
7. Sullivan SD, Rasouliyan L, Russo PA, Kamath T, Chipps BE. Extent, patterns, and
burden of uncontrolled disease in severe or dicult-to-treat asthma. Allergy.
2007;62(2):126-133.
8. Yawn BP, Wechsler ME. Severe asthma and the primary care provider: identifying
patients and coordinating multidisciplinary care. Am J Med. 2017;130(12):1479.
9. Papadopoulos NG, Arakawa H, Carlsen KH, et al. International consensus on (ICON)
pediatric asthma. Allergy. 2012;67(8):976-997.
10. Lommatzsch M, Virchow JC. Severe asthma: denition, diagnosis and treatment.
Dtsch Arztebl Int. 2014;111(50):847-855.
11. Salo PM, Wilkerson J, Rose KM, et al. Bedroom allergen exposures in US households.
J Allergy Clin Immunol. 2018;141(5):1870-1879.e1814.
12. Yawn BP, Rank MA, Cabana MD, Wollan PC, Juhn YJ. Adherence to asthma guide-
lines in children, tweens, and adults in primary care settings: a practice-based net-
work assessment. Mayo Clinic Proc. 2016;91(4):411-421.
13. Colice GL, Ostrom NK, Geller DE, et al. e CHOICE survey: high rates of persis-
tent and uncontrolled asthma in the United States. Ann Allergy Asthma Immunol.
2012;108(3):157-162.
14. Yawn BP, Wollan PC, Rank MA, Bertram SL, Juhn Y, Pace W. Use of asthma APGAR
tools in primary care practices: a cluster-randomized controlled trial. Ann Fam Med.
2018;16(2):100-110.
15. National Asthma Education and Prevention Program (NAEPP). Guidelines for the
Diagnosis and Management of Asthma (EPR-3). https://www.nhlbi.nih.gov/health-
pro/guidelines/current/asthma-guidelines/full-report. Accessed 31 May 2018.
16. GINA—Global Initiative for Asthma (GINA). Guidelines 2017. http://ginasthma.org.
Accessed 21 May 2018.
Regulatory approval code: 51981.AL.US1.EN.v1.18

S5
AUGUST 2018
The Practical Application of Allergic Trigger
Management to Improve Asthma Outcomes:
Step 1: Identify Patients with Allergic
Components of Asthma
Andrew Liu, MD; Allan Luskin, MD; Randall Brown, MD, MPH, AE-C; Michael D. Cabana, MD, MPH; Ivor
Emanuel, MD; Len Fromer, MD, FAAFP; Christine W. Wagner, APRN, MSN, AE-C; Barbara P. Yawn, MD, MSc,
FAAFP
DISCLOSURES
Dr. Liu discloses that he is a consultant for Thermo Fisher
Scientic.
Dr. Luskin has no conicts to disclose.
Dr. Brown reports that he is on the Board of Directors for Allergy
and Asthma Network; an advisor and speaker for AstraZeneca; a
speaker for Circassia Pharmaceuticals plc; a speaker for Integrity
Continuing Education Inc.; an advisor for Novartis AG; a speaker for
Teva Pharmaceutical Industries Ltd.; and an advisor for Thermo Fisher
Scientic.
Dr. Cabana is on the Merck Speakers Bureau and consults with
Novartis AG, Genentech, Inc. and Thermo Fisher Scientic.
Dr. Emanuel has an ongoing relationship with Thermo Fisher
Scientic.
Dr. Fromer has been a consultant and speaker for Thermo Fisher
Scientic in the recent past.
Christine W. Wagner has an ongoing relationship with Thermo
Fisher Scientic.
Dr. Yawn is a paid consultant and has an ongoing relationship with
Thermo Fisher Scientic.
ACKNOWLEDGEMENT
The Task Force appreciates the editorial support provided
by Sarah Staples, whose work was nancially supported by
Thermo Fisher Scientic. The Task Force also acknowledges and
appreciates the important logistical support provided by Kevin H.
TenBrink and Gabriel Ortiz of Thermo Fisher Scientic.
Kim thought back through her recent asthma visit. She had
mentioned her concern about “hay fever” and wondered if any-
thing else was triggering her asthma attacks. She completed
the intake sheet and circled some things she thought made her
asthma worse—but no one had commented on any of them. Did
she have allergies? And were they making her asthma worse?
Her asthma was certainly causing problems, including missing
sleep and work, and interfering with her ability to care for her
children and family. What should she do next?
K
im’s experience is not unusual. Although widely
disseminated asthma-treatment guidelines are
available, along with a variety of eective pharma-
cotherapies, most patients with asthma continue to have
symptoms. Across all types of practices, almost half of adults
with asthma (47%) report very poorly controlled asthma
and another 24% report not well-controlled asthma.
1
Simi-
larly, the prevalence of uncontrolled asthma in children
with asthma in all practices is 46%.
2
In primary care prac-
tices, 63% of adults, 52% of adolescents, and 56% of children
with asthma have inadequate asthma control.
3
Most people
with asthma receive their care in a primary care setting, and
most continue to have suboptimal control of symptoms and
exacerbations.
3-7
National and international guidelines strongly support
the importance of evaluating and addressing environmental
triggers that can make asthma worse and cause exacerba-
tions.
8,9
e 2007 National Asthma Education and Preven-
tion Program (NAEPP) US guidelines recommend evaluating
the potential role of allergens, particularly indoor inhalant
allergens.
8
is recommendation is considered “Evidence
Category A” (ie, strong evidence from randomized controlled
trials with a rich body of supportive data).
8
Since publication
of these guidelines, additional compelling evidence has been
published on the importance of recognizing and treating the
allergic components of asthma.
10,11
Given the importance of allergens to asthma
morbidity and asthma management, patients
with persistent asthma should be evaluated
for the role of allergens as possible contributing
factors. —NAEPP. GUIDELINES FOR THE DIAGNOSIS AND
MANAGEMENT OF ASTHMA (EPR-3)
8
S5
SEPTEMBER 2018

S6
SEPTEMBER 2018
[STEP 1:
ALLERGIC COMPONENTS OF ASTHMA
]
ASTHMA AND INFLAMMATION
Asthma is a condition of hypersensitivity to common expo-
sures, associated with chronic airway inammation, bron-
chial hyperreactivity with increased mucus, and airway
edema, obstruction, and narrowing. Symptom frequency
and severity are variable, but the underlying inammation
and hyperreactivity of the airways are chronic and present
even when a person “feels well.” Over time, these symptoms
may be associated with persistent narrowing and remodel-
ing of the airways (FIGURE 1
12
).
Sensitization
More than 80% of children and adolescents and 60% of
adults
13,14
with asthma are sensitized to inhaled environ-
mental allergens. Among all ages, 70% of patients with
severe asthma are allergic.
15-17
ere is a direct and causal
relationship between allergic sensitization and asthma
control and exacerbations.
18
For most people with asthma,
hypersensitivity includes reactions to environmental expo-
sures. Liu and colleagues summarized multiple pathways
linked to asthma severity, including allergen sensitization
(FIGURE 2).
19
Long-term implications of inhaled
allergen sensitization and exposure
In children, allergy is also a risk factor for asthma persis-
tence (FIGURE 3
20
). Only 10% of children with nonaller-
gic asthma at age 5 years continue to have asthma by age
12 years. In contrast, approximately 50% of children
with allergic asthma continue to have symptoms at age
12 years.
20
Early sensitization to multiple inhalant aller-
gens
21-23
and sensitization combined with perennial expo-
sure in the home in early life
24
predict asthma persistence,
exacerbation, and lung dysfunction.
FIGURE 1 Airway remodeling caused by asthma-associated inammation
12
Normal Airway Asthmatic Airway
Triggers
Normal,
subclinical
response
Complete
Recovery
(Partial) recovery
Obstruction
Inflammation & Bronchial
Hyperresponsiveness
Remodeling
Hypertrophic smooth muscle
Collagen deposition
Thickened Basement Membrane
Mucus and
Cell debris
Edema
Bronchospasm
Reprinted from Papadopoulus, et al. International consensus on (ICON) pediatric asthma. Allergy. 2012;67(8):976-997. Used with permission.

S7
SEPTEMBER 2018
[STEP 1:
ALLERGIC COMPONENTS OF ASTHMA
]
In sensitized children, adolescents, and adults, expo-
sure to allergic triggers is associated with an increase in
asthma symptoms, decreased lung function, and recur-
ring asthma exacerbations. In addition, those with multiple
inhaled allergen sensitizations are at increased risk of worse
control, often resulting in sick visits to the oce and visits
to urgent care and the emergency department (ED),
25
as
well as hospitalizations (FIGURE 4).
26
e number of asthma
triggers a patient has is associated with the risk of exacer-
bations, more severe exacerbations, and poorer quality
of life.
18
Although viral infection is a common trigger for asthma
exacerbations, especially in younger children, recent data
demonstrate that allergen sensitization results in a signi-
cant increased risk of asthma exacerbation when there is a
combination of allergen sensitization, exposure, and viral
infection (FIGURE 4
26
). e allergic phenotype of asthma
is associated with an impaired innate immune response
FIGURE 2 Pathways by which asthma risk factors contribute to asthma severity
19
Red arrows indicate how allergy acts through multiple pathways (allergen sensitization, allergic inammation, pulmonary physiology, and rhinitis
severity) to affect asthma severity. The negative effect of tobacco smoke exposure is partially mediated by pulmonary physiology (olive arrows).
Vitamin D is inversely associated with inammation (yellow arrow) but its overall effect on asthma severity is insignicant.
Reprinted from Liu et al. Pathways through which asthma risk factors contribute to asthma severity in inner-city children. J Allergy Clin Immunol. 2016;138(4):1042-1050.
® 2016 with permission from Elsevier.

S8
SEPTEMBER 2018
[STEP 1:
ALLERGIC COMPONENTS OF ASTHMA
]
to respiratory viral infection, mediated through immu-
noglobulin E (IgE). e link between viral infections and
allergen sensitization is conrmed by the decreased risk
of asthma exacerbation due to
viral upper respiratory infec-
tion (URI) when IgE-directed
therapy is prescribed for sensi-
tized or “allergic” children and
adolescents.
27,28
The role of serum IgE
Total IgE levels have been
used as an indicator of allergic
asthma. Although higher levels
of total serum IgE have been
associated with poorer asthma
outcomes
29,30
and higher health
care costs,
31
these levels are
variable, aected by genetics,
race, cigarette smoking, and
steroid use, and are, therefore,
not a reliable indicator of aller-
gen sensitization and not a sub-
stitute for specic IgE allergen
testing. Signicant allergy may
exist with low or “normal” total
IgE levels, and higher total IgE
levels may exist without any
signicant specic allergic sen-
sitization. Increasingly, overall
allergen sensitization is being
recognized as a major factor in
asthma across all age groups
and all levels of asthma sever-
ity.
32
Asthma phenotypes
Recent evidence demonstrates
that the common exacerbation-
prone phenotype in US inner
city children with asthma, rep-
resenting 16% of these children,
included sensitization to most
common inhalant allergens for
which they were tested (a mean
of 14 sensitizations from a 22-
allergen panel).
33
is indicates
that exacerbation-prone asth-
matic children are typically
highly allergic to their environ-
ment. In the Epidemiology and Natural History of Asthma:
Outcomes and Treatment Regimens (TENOR) study, there
was a direct relationship between the number of allergens
Risk Factors
Odds Ratios
Sensitization, Exposure,
and Viral Infection
Sensitization and Viral Infection
Viral Infection
Sensitization and Exposure
Sensitization
1.8
2.6
3.2
8.9
19.4
FIGURE 4 Allergen sensitization, exposure, and viral infection greatly
increase the risk for asthma hospital admissions
26
The risk (odds ratio) of severe asthma exacerbations resulting in hospitalization increases across
groups of patients experiencing allergen sensitization, sensitization with exposure to allergen, viral
infection (upper respiratory infection), and combinations of these factors.
FIGURE 3 Children with persistent wheeze and inhalant allergies in
preschool life are more likely to develop persistent asthma
20
Approximately 50% of children with atopic asthma characterized by wheezing continue to have
symptoms at age 12 years. Early sensitization to multiple inhalant allergens and sensitization com-
bined with perennial exposure in the home in early life predict asthma persistence, exacerbation,
and lung dysfunction.
Reprinted from Liu & Martinez. Chapter 2: Natural History of Allergic Diseases and Asthma. In: Leung DYM, et al. (eds.).
Pediatric Allergy: Principles and Practice, 3rd ed. Elsevier, Inc.; 2016. ® 2016 with permission from Elsevier.
Atopy-Associated
Asthma
Transient Early
Wheezers
Wheezing Prevalence
Nonallergic
Wheezers
Asthma in Obese
Females with
Early-Onset Puberty
Age (years)
036912

S9
SEPTEMBER 2018
[STEP 1:
ALLERGIC COMPONENTS OF ASTHMA
]
to which adults, adolescents,
and children were sensitized and
their rates of exacerbations, the
severity of those exacerbations,
and the person’s asthma-related
quality of life.
32
Zoratti and colleagues dis-
tinguished 5 potential asthma
phenotypes (A, B, C, D, and E)
in US inner city children, with
asthma severity burdens ranging
from minimal to high (
FIGURE 5).
33
Children with phenotypes C, D,
and E demonstrate progressively
greater allergen sensitization
and increasingly worse clinical
conditions, likely representing
classic T-helper type 2-driven
allergic asthma. ese allergic
phenotypes also represent 70%
of the study population and
exhibit striking parallel relation-
ships between allergic sensiti-
zation and indicators of asthma
severity. Compatible with
this picture of allergen-driven
asthma, phenotype A represents
the group with low sensitiza-
tion levels and low asthma bur-
den. Only phenotype B appears
to highlight other non-allergic
mechanisms of asthma that may
result in signicant asthma symptom burden.
THE PRIMARY CARE
CHALLENGE
ree-quarters of people with asthma receive care in a pri-
mary care practice.
34
ese people and their families con-
tinue to experience a signicant asthma-related disease
burden, with over 10.5 million oces visits, most of which
are unscheduled and in primary care oces, added to 1.8
million ED visits and more than 400,000 hospitalizations
annually.
12,35,36
ree of every 5 children and more than half
of adults with asthma have had their life disrupted by the
need to seek urgent or emergency care for their asthma
each year.
37
About 10% of people with asthma have severe
asthma, resulting in several urgent and emergency visits
and a high risk of asthma-related hospitalization, in addi-
tion to missed school, work, and activity days.
38,39
Several
studies have demonstrated that this continuing asthma
burden is not simply the basis for prescribing more asthma
medications; further evaluation should be undertaken.
Allergen avoidance and abatement (eg, environmen-
tal control), as well as allergy treatments such as immu-
notherapy (subcutaneous or sublingual), require identi-
cation of allergen sensitization. Particularly in children,
allergy avoidance and immunotherapy have improved
asthma control with decreased symptoms, decreased exac-
erbations, and decreased oral and inhaled corticosteroid(s)
use.
40
Yet allergy evaluation was only discussed in about
33% of primary care oce visits for asthma, and allergy test-
ing was only documented in 2% of cases of asthma over the
course of a year.
3
Several questionnaires to assess asthma
control are available (
FIGURE 6). A newly published study
is the rst to nd that introducing an asthma tool—the
Asthma APGAR Plus—into primary care practices improves
patient and practice outcomes.
7
e Asthma APGAR Plus is
the only tool that includes a brief patient query regarding aller-
FIGURE 5 Children with high asthma burden are highly allergic
to their environment
33
* For a full description of asthma medication steps, refer to pages 46–52 of the EPR–3 Summary Report 2007.
8
The higher the step number (from 1 to 6), the more intense the medication regimen.
Reprinted from Zoratti, et al. Asthma phenotypes in inner-city children. J Allergy Clin Immunol. 2016;138(4):1016-1029.
® 2016 with permission from Elsevier.
Asthma Phenotypes (N=616)
A (15%) B (15%) C (24%) D (30%) E (16%)
Asthma symptoms Minimal High Minimal Minimal Highest
Lung function/
impairment
Normal Mild Minimal Intermediate Most
Allergen
sensitization (no.
of positive tests in
22-allergen panel)
1 2 9 13 14
Step in asthma
medication plan*
1.39 4.2 1.93 3.4 4.7
Rhinitis symptom
severity
Minimal Intermediate Minimal High High

S10
SEPTEMBER 2018
[STEP 1:
ALLERGIC COMPONENTS OF ASTHMA
]
FIGURE 6 Assessment tools for asthma symptom control
APGAR, Activities, Persistent, triGGers, Asthma medications, Response to therapy.
1. Nathan RA, et al. J Allergy Clin Immunol. 2004;113(1):59-65.
2. Juniper EF, et al. Eur Respir J. 1999;14(4):902-907.
3. Vollmer WM, et al. Am J Respir Crit Care Med. 1999;160(5 Pt 1):1647-1652.
4. Yawn BP, et al. J Asthma Allergy. 2008;31(1):1-10.
Available Assessment Tools to
Evaluate Asthma Symptom Control
Asthma Control Test
(ACT)
1
Asthma Therapy
Assessment
Questionaire (ATAQ)
3
Asthma Control
Questionaire (ACQ)
2
Asthma APGAR Plus
4
gies and triggers, designed to facilitate discussion of allergens
and need for further allergy evaluation with patients. Using
a tool to assess potential “allergies” is the rst step in allergy
evaluation, which often requires investigation and care over
a number of visits, an important hallmark of the continuity of
primary care.
WHO SHOULD BE TESTED FOR INHALANT
ALLERGEN SENSITIZATION?
All patients who have been given a diagnosis of persis-
tent asthma should be evaluated to identify their allergic
triggers. But this recommendation is not typically imple-
mented in the primary care setting, where there are con-
cerns about limited time, cost, and patient burden. A more
practical approach is to identify the specic patient groups
most likely to benet from evaluation of the potential
allergic contribution to asthma burden (FIGURE 7).
1. Patients of any age who continue to have high
asthma burden or high risk despite treatment.
a. A severe exacerbation requiring hospitalization
b. Two or more ED asthma visits a year resulting in
treatment with systemic corticosteroids, such as
prednisone and dexamethasone
c. Prescribed step-4 or step-5 asthma treatment, which
includes high-dose ICS
d. ose whose primary care clinician may con-
sider them a potential candidate for biologic
therapy but who have not yet had an allergy
evaluation.
In this high-burden/high-risk asthma group, diag-
nostic testing for inhalant allergen sensitization can help
identify people with high-risk asthma who are highly aller-
gic; identify specic allergen exposures that can underlie
their high asthma burden; and identify those who may
benet from specic asthma therapies to reduce their
asthma burden, lower the risk of future exacerbation, limit
the risk of side eects from high-dose ICS, and limit the
morbidity and mortality of future exacerbations and the
side-eects of“bursts” of oral corticosteroids (OCS) used
to treat them.

S11
SEPTEMBER 2018
[STEP 1:
ALLERGIC COMPONENTS OF ASTHMA
]
2. Young children with recurrent cough/wheeze
symptoms to help predict their likelihood of
persistence of “asthma” beyond age 6 years.
Inhalant allergen sensitization, atopic dermatitis, aller-
gic rhinitis, and parental asthma are key risk factors to
predict which preschoolers with recurrent respiratory
symptoms, such as cough and wheeze, are most likely to
develop persistent asthma. Allergen sensitization can-
not be adequately assessed by history and physical exam
alone. Diagnosing specic inhalant allergen sensitizations
in at-risk children identies those who are most likely to
develop persistent asthma and allows opportunities for
designing allergen-avoidance strategies that may improve
outcomes.
3. Patients of any age meeting any of the asthma Rules
of Two
®
* criteria while on daily controller or
maintenance therapy.
a. Having >2 days/week of asthma symptoms or quick
relief inhaler use
b. Having >2 nights/month of nighttime asthma
symptoms
c. Having ≥2 asthma exacerbations/year resulting in a
burst of OCS
d. Requiring >2 rescue albuterol inhaler lls/rells a
year not when used just to cover dierent sites such
as home/school/daycare/oce.
*Registered trademark of Baylor Health Care System. Adapted
from: Millard et al. Proc (Bayl Univ Med Cent). 2014;27(2):79-82.
e presence of daytime and/or nighttime symptoms and/
or the need for additional medication prompts the need
for additional management. Diagnostic testing for inhalant
allergen sensitization can identify specic allergen expo-
sures that, when treated, may allow a step-down in high-
dosage ICS therapy and may identify patients with asthma
who may benet from specic asthma therapies to reduce
their asthma burden and risk of future exacerbations.
CHANGING PRACTICE
When exacerbations or out-of-control symptoms are recog-
nized, a common approach is to simply add more medica-
tions, which is often expensive and ineective.
4
Before con-
sidering any additional therapy, it is important that patients
are receiving the prescribed therapy at the target site. High
asthma burden is not necessarily a deciency of prescribed
pharmacotherapy. Two issues should always be addressed
before adding more inhalers:
• Is the patient taking the medications?
• Are the medications getting into the lungs?
Rules of Two
®
is a registered trademark ofBaylorHealth Care System. Adapted from: Millard et al. Proc (Bayl Univ Med Cent). 2014;27(2):79-82.
FIGURE 7 Patients in need of an allergy evaluation
Patients of any age experiencing a high asthma burden or
high risk despite treatment
• An asthma-related hospitalization or 2 or more emergency department visits
• Step 4 or higher medication regimen
• Potential candidate for biologics
Young children with recurrent cough/wheeze symptoms to help
predict the likelihood of asthma persistence beyond 6 years.
Patients of any age meeting the asthma "Rules of 2" criteria
while on therapy
• >2 days/week of symptoms or quick relief inhaler use
• >2 nights/month of nighttime asthma symptoms
• ≥2 asthma exacerbations/year (episodes resulting in a burst of oral steroids) or >2 rescue
albuterol inhaler lls/rells per year
S12
SEPTEMBER 2018
[STEP 1:
ALLERGIC COMPONENTS OF ASTHMA
]
Nonadherence is a common problem that we discuss
in the next article. Inadequate inhaler technique is also
common and must be addressed by selecting inhaler or
drug delivery devices tailored to the patient’s age and capa-
bilities.
3,41
After selecting the appropriate device, teaching,
observing, and reassessing proper inhaler technique regu-
larly can enhance drug delivery and improve unintentional
nonadherence, decreasing symptom and exacerbation
burden.
For many people with asthma, addressing adher-
ence and inhaler technique fails to mitigate the underly-
ing cause of bronchial hyperreactivity: the inammatory
response to allergic triggers. Identication of allergens to
which the patient is sensitized and attempts to decrease
allergen impact are also needed.
3
NAEPP guidelines
8
and
the NAEPP Guideline Implementation Panel
42
recommend
determining the patient’s exposure to allergens, assessing
sensitization from the medical history and skin or in vitro
testing, and interpreting positive results in the context of the
patient’s medical history.
8
Accordingly, incorporating aller-
gen identication into routine asthma management is the
main goal of this supplement.
CONCLUSIONS
Assessing and dealing with asthma-related allergies can
help prevent airway remodeling, reduce children’s and
adolescents’ days of wheezing and asthma-related hospi-
talizations, and, in adults, reduce the necessity for quick-
relief medications and nighttime awakenings. Although all
people with asthma may be an appropriate candidate for
aeroallergen sensitization assessment, the groups with the
highest likelihood of benet are those with high asthma
burden, an uncertain asthma future, and uncontrolled
symptoms.
Kim came into the ofce after another visit to the ED last month,
where she was again given a diagnosis of “bronchitis,” given
oral corticosteroids plus antibiotics, and told to take her asthma
medications regularly. The pharmacy lled the prescriptions
from the ED, but told her that the usual asthma prescriptions
were too old to rell and her children’s prescriptions could not
be relled either, so she had no source of medication and is
wheezing and short of breath again.
Today, Kim’s Asthma APGAR score is 4—conrming her
out-of-control asthma. She circled several triggers, includ-
ing tobacco smoke, pets, and seasonal issues. She noted
her incomplete adherence, due primarily to cost and lack of a
current prescription for the asthma medications, and further
reported that her asthma medications were only “somewhat
helpful” even when used. Your diagnosis is difcult-to-control
asthma, due to issues of adherence and unidentied triggers
that have not been addressed. She asks you about allergies.
Kim and you agree to her continued use of daily moderate-
strength ICS, combined with a long-acting beta-agonist bron-
chodilator. Upon review of inhaler technique, the medical assis-
tant noted some errors that were corrected; nal observation
demonstrated adequate inhaler technique. Following discus-
sion of Kim’s suspected allergies and your expressed concerns
about the potential impact of allergies on her asthma symptoms
and exacerbations, she agrees to have the blood test for pos-
sible allergen sensitization but declines to visit an allergist at this
time, due to concerns about getting time off work and visiting
yet another physician. As Kim makes an appointment to return
to review the allergy test results, she comments to your recep-
tionist, “She is the rst doctor who has bothered to listen to me
about my asthma and allergies. I will give her another try.” l
REFERENCES
1. Murphy KR, Meltzer EO, Blaiss MS, Nathan RA, Stolo SW, Doherty DE. Asthma
management and control in the United States: results of the 2009 Asthma Insight
and Management survey. Allergy Asthma Proc. 2012;33(1):54-64.
2. Stanford RH, Gilsenan AW, Ziemiecki R, Zhou X, Lincourt WR, Ortega H. Predic-
tors of uncontrolled asthma in adult and pediatric patients: analysis of the Asth-
ma Control Characteristics and Prevalence Survey Studies (ACCESS). J Asthma.
2010;47(3):257-262.
3. Yawn BP, Rank MA, Cabana MD, Wollan PC, Juhn YJ. Adherence to asthma guide-
lines in children, tweens, and adults in primary care settings: a practice-based net-
work assessment. Mayo Clinic Proc. 2016;91(4):411-421.
4. Sullivan SD, Rasouliyan L, Russo PA, Kamath T, Chipps BE; TENOR Study Group.
Extent, patterns, and burden of uncontrolled disease in severe or dicult-to-treat
asthma. Allergy. 2007;62(2):126-133.
5. Fuhlbrigge A, Reed ML, Stempel DA, Ortega HO, Fanning K, Stanford RH. e
status of asthma control in the U.S. adult population. Allergy Asthma Proc.
2009;30(5):529-533.
6. Colice GL, Ostrom NK, Geller DE, et al. e CHOICE survey: high rates of persis-
tent and uncontrolled asthma in the United States. Ann Allergy Asthma Immunol.
2012;108(3):157-162.
7. Yawn BP, Wollan PC, Rank MA, Bertram SL, Juhn Y, Pace W. Use of asthma APGAR
tools in primary care practices: a cluster-randomized controlled trial. Ann Fam
Med. 2018;16(2):100-110.
8. National Asthma Education and Prevention Program (NAEPP). Guidelines for the
diagnosis and management of asthma (EPR-3). www.nhlbi.nih.gov/health-pro/
guidelines/current/asthma-guidelines/full-report. Accessed June 28, 2018.
9. Global Initiative for Asthma. Pocket guide for asthma management and preven-
tion. https://ginasthma.org/wp-content/uploads/2017/02/wms-Main-pocket-
guide_2017.pdf
10. Agency for Healthcare Research and Quality (AHRQ). Topic: Asthma. www.ahrq.
gov/topics/asthma.html. Accessed June 28, 2018.
11. European Academy of Allergy and Clinical Immunology. AIT guidelines. www.eaa-
ci.org/resources/guidelines/ait-guidelines-part-2.html. Accessed June 28, 2018.
12. Papadopoulos NG, Arakawa H, Carlsen KH, et al. International consensus on
(ICON) pediatric asthma. Allergy. 2012;67(8):976-997.
13. Busse PJ, Cohn RD, Salo PM, Zeldin DC. Characteristics of allergic sensitization
among asthmatic adults older than 55 years: results from the National Health
and Nutrition Examination Survey, 2005-2006. Ann Allergy Asthma Immunol.
2013;110(4):247-252.
14. Høst A, Halken S. e role of allergy in childhood asthma. Allergy. 2000;55(7):
600-608.
15. Wenzel SE. Asthma phenotypes: the evolution from clinical to molecular ap-
proaches. Nat Med. 2012;18(5):716-725.
16. Arbes SJ Jr., Gergen PJ, Vaughn B, Zeldin DC. Asthma cases attributable to atopy:
results from the ird National Health and Nutrition Examination Survey. J Allergy
Clin Immunol. 2007;120(5):1139-1145.
17. Moore WC, Bleecker ER, Curran-Everett D, et al; National Heart, Lung, and Blood
Institute’s Severe Asthma Research Program. Characterization of the severe asth-
ma phenotype by the National Heart, Lung, and Blood Institute’s Severe Asthma
Research Program. J Allergy Clin Immunol. 2007;119(2):405-413.

S13
SEPTEMBER 2018
[STEP 1:
ALLERGIC COMPONENTS OF ASTHMA
]
18. Luskin AT, Chipps BE, Rasouliyan L, Miller DP, Haselkorn T, Dorenbaum A. Im-
pact of asthma exacerbations and asthma triggers on asthma-related quality of life
in patients with severe or dicult-to-treat asthma. J Allergy Clin Immunol Pract.
2014;2(5):544-552.e1-e2.
19. Liu AH, Babineau DC, Krouse RZ, et al. Pathways through which asthma risk fac-
tors contribute to asthma severity in inner-city children. J Allergy Clin Immunol.
2016;138(4):1042-1050.
20. Liu AH, Martinez FD. Chapter 2: Natural history of allergic diseases and asthma.
In: Leung DYM, ed. Pediatric Allergy: Principles and Practice. 3rd ed. Atlanta, GA:
Elsevier, Inc.; 2016:
21. Simpson A, Tan VY, Winn J, et al. Beyond atopy: multiple patterns of sensitiza-
tion in relation to asthma in a birth cohort study. Am J Respir Crit Care Med.
2010;181(11):1200-1206.
22. Belgrave DC, Buchan I, Bishop C, Lowe L, Simpson A, Custovic A. Trajecto-
ries of lung function during childhood. Am J Respir Crit Care Med. 2014;189(9):
1101-1109.
23. Havstad S, Johnson CC, Kim H, et al. Atopic phenotypes identied with latent class
analyses at age 2 years. J Allergy Clin Immunol. 2014;134(3):722-727.e2.
24. Illi S, von Mutius E, Lau S, Niggemann B, Gruber C, Wahn U; Multicentre Allergy
Study (MAS) group. Perennial allergen sensitisation early in life and chronic asth-
ma in children: a birth cohort study. Lancet. 2006;368(9537):763-770.
25. Butz A, Morphew T, Lewis-Land C, et al. Factors associated with poor controller
medication use in children with high asthma emergency department use. Ann Al-
lergy Asthma Immunol. 2017;118(4):419-426.
26. Murray CS, Poletti G, Kebadze T, et al. Study of modiable risk factors for asthma
exacerbations: virus infection and allergen exposure increase the risk of asthma
hospital admissions in children. orax. 2006;61(5):376-382.
27. Teach SJ, Gill MA, Togias A, et al. Preseasonal treatment with either omalizumab or
an inhaled corticosteroid boost to prevent fall asthma exacerbations. J Allergy Clin
Immunol. 2015;136(6):1476-1485.
28. Gill MA, Liu AH, Calatroni A, et al. Enhanced plasmacytoid dendritic cell antiviral
responses after omalizumab. J Allergy Clin Immunol. 2018;141(5):1735-1743.e9.
29. Burrows B, Martinez FD, Halonen M, Barbee RA, Cline MG. Association of
asthma with serum IgE levels and skin-test reactivity to allergens. N Engl J Med.
1989;320:271-277.
30. Borish L, Chipps B, Deniz Y, Gujrathi S, Zheng B, Dolan CM; TENOR Study Group.
Total serum IgE levels in a large cohort of patients with severe or dicult-to-treat
asthma. Ann Allergy Asthma Immunol. 2005;95(3):247-253.
31. Luskin AT, Antonova E, Broder M, Chang E, Omachi TA. Higher immunoglobulin E
(IgE) levels are associated with greater emergency care and other healthcare utili-
zation among asthma patients in a real-world data setting. J Allergy Clin Immunol.
2016;137(2 Suppl):AB9.
32. Chipps BE, Zeiger RS, Borish O, et al; TENOR Study Group. Key ndings and clini-
cal implications from e Epidemiology and Natural History of Asthma: Outcomes
and Treatment Regimens (TENOR) study. J Allergy Clin Immunol. 2012;130(2):
332-342.e10.
33. Zoratti EM, Krouse RZ, Babineau DC, et al. Asthma phenotypes in inner-city chil-
dren. J Allergy Clin Immunol. 2016;138(4):1016-1029.
34. Kwong KYC, Eghrari-Sabet JS, Mendoza GR, et al. e benets of specic im-
munoglobulin E testing in the primary care setting. Am Manage Care. 2011;17:
S447-S459.
35. Asthma. Centers for Disease Control and Prevention; March 31, 2017. www.cdc.
gov/nchs/fastats/asthma.htm. Accessed June 28, 2018.
36. Federal Interagency Forum on Child and Family Statistics. America’s children in
brief: Key national indicators of well-being, 2012. Washington, DC: US Govern-
ment Printing Oce. www.childstats.gov/pdf/ac2012/ac_12.pdf. Accessed June
28, 2018.
37. Most recent asthma data. Centers for Disease Control and Prevention; May 15,
2018. www.cdc.gov/asthma/most_recent_data.htm. Accessed June 28, 2018.
38. Zeiger RS, Schatz M, Dalal AA, et al. Utilization and costs of severe uncon-
trolled asthma in a managed-care setting. J Allergy Clin Immunol. 2016;4(1):
120-129.e3.
39. Chipps BE, Haselkorn T, Rosén K, Mink DR, Trzaskoma BL, Luskin AT. Asthma ex-
acerbations and triggers in children in TENOR: impact on quality of life. J Allergy
Clin Immunol. 2018;6(1):169-176.e2.
40. Lin SY, Azar A, Suarez-Cuervo C, et al. e Role of Immunotherapy in the Treat-
ment of Asthma. Comparative Eectiveness Review No. 196 (Prepared by the Johns
Hopkins University Evidence-based Practice Center under Contract No.290-2015-
00006-I). AHRQ Publication No. 17(18)-EHC029-EF. Rockville, MD: Agency for
Healthcare Research and Quality; March 2018. https://eectivehealthcare.ahrq.
gov/sites/default/les/pdf/cer-196-full-immunotherapy-asthma.pdf. Accessed
June 28, 2018.
41. Price DB, Roman-Rodriguez M, McQueen RB, et al. Inhaler errors in the CRITIKAL
study: type, frequency, and association with asthma outcomes. J Allergy Clin Im-
munol. 2017;5(4):1071-1081.e9.
42. National Institutes of Health, National Heart Lung and Blood Institute. Guidelines
implementation panel report for: Expert Panel Report 3—guidelines for the diagnosis and
management of asthma: Partners putting guidelines into action. Bethesda, MD: US De-
partment of Health and Human Services ; 2008 Dec. NIH Publication Number 09-6147.
www.nhlbi.nih.gov/guidelines/asthma/gip_rpt.pdf. Accessed June 28, 2018.
Regulatory approval code: 52044.AL.US1.EN.v1.18

AUGUST 2018
The Practical Application of Allergic Trigger
Management to Improve Asthma Outcomes:
Step 2: Identifying and Addressing Allergen
Exposure in Daily Practice
Christine W. Wagner, APRN, MSN, AE-C; Allan Luskin, MD; Len Fromer, MD, FAAFP;
Barbara P. Yawn, MD, MSc, FAAFP; Randall Brown, MD, MPH; Andrew Liu, MD
DISCLOSURES
Christine W. Wagner has an ongoing relationship with Thermo
Fisher Scientic.
Dr. Luskin has no conicts to disclose.
Dr. Fromer has been a consultant and speaker for Thermo Fisher
Scientic in the recent past.
Dr. Yawn is a paid consultant and has an ongoing relationship with
Thermo Fisher Scientic.
Dr. Brown reports that he is on the Board of Directors for Allergy
and Asthma Network; an advisor and speaker for AstraZeneca; a
speaker for Circassia Pharmaceuticals plc; a speaker for Integrity
Continuing Education Inc.; an advisor for Novartis AG; a speaker
for Teva Pharmaceutical Industries Ltd.; and an advisor for Thermo
Fisher Scientic.
Dr. Liu discloses that he is a consultant for Thermo Fisher
Scientic.
ACKNOWLEDGEMENT
The Task Force appreciates the editorial support provided
by Sarah Staples, whose work was nancially supported by
Thermo Fisher Scientic. The Task Force also acknowledges and
appreciates the important logistical support provided by Kevin H.
TenBrink and Gabriel Ortiz of Thermo Fisher Scientic.
I
n the previous article, we presented the rationale for
allergy testing as part of asthma care and made recom-
mendations for identifying patients with the greatest
need for allergy assessment, testing, and interventions. Next,
we present suggestions for prioritizing the allergens to be
assessed, tests that identify allergen sensitization, and treat-
ments, including avoidance, environmental control, phar-
macotherapy, and immunotherapy.
Maristela Nabong-Nillas, MD, Chief of Pediatrics at Little
River Medical Center, SC, speaks about asthma and allergy
evaluation from rsthand experience:
“When I moved here, I noticed that many patients—per-
haps one-third—had atopic problems, including allergy and
asthma. During my career, asthma care has unfolded, from
simply treating acute exacerbations that required hospital-
ization to allowing management for most asthma on an out-
patient basis.
“Improving outcomes for patients with asthma requires
a multicomponent coordinated effort. We were fortunate
to be a part of The QTIP project (Quality Through Technol-
ogy and Innovations in Pediatrics), a Federal CHIPRA (Chil-
dren’s Health Insurance Program Reauthorization Act) Qual-
ity Improvement grant in 2011 to address quality measures,
including asthma management. We developed system-wide
methods to identify people with persistent asthma using daily
controller medication to see if they had asthma action plans,
and had received evaluation for environmental triggers.
“Initially, we asked parents about suspected triggers and
used their responses. At the time, trigger testing required
referral to an allergist. Many of our patients did not want
to or could not take this step. Now, we identify triggers
based on blood work (specic immunoglobulin E [sIgE]
testing). Parents are interested in knowing about trig-
gers and like not having skin testing. Patients return after
2 weeks to discuss results. Positive results are followed up
with face-to-face education and handouts explaining how
to reduce exposure.
“If parents learn that environmental measures will help avoid
triggers, they are open to testing. They’re the ones who are
up at night and they’re appreciative if they know what to
avoid. Negative results let us focus on nonallergic causes for
symptoms. I have not had to admit any patients with asthma
for the past 3 years because their asthma symptoms are
being controlled.”
COMMON TRIGGERS/ALLERGENS AND
EFFECTIVE CONTROL MEASURES
ere is strong evidence that exposing patients with asthma
S14
SEPTEMBER 2018

S15
SEPTEMBER 2018
[
STEP 2: ALLERGEN EXPOSURE IN DAILY PRACTICE
]
who are sensitized to certain indoor and outdoor aeroaller-
gens increases symptoms in those with high asthma burden,
resulting in frequent exacerbations.
1,2
Identifying sensitiza-
tion to specic aeroallergens is required to guide appropri-
ate targeted exposure control. e plan for environmental
control is often complicated by the frequent presence of
multi-sensitization, requiring multiple control measures.
e National Asthma Education and Prevention Program
(NAEPP) guidelines recommend using allergy testing to
educate patients about the role of allergens in their disease
and to delineate specic environmental control measures for
sensitized patients experiencing symptoms.
3
Relevance of identifying common allergens
Of all the relevant indoor antigens, house dust mite is the
most common. ere are very few locations in the United
States in which house dust mites are not of concern. Only
high altitude (>3,000 feet above sea level) protects against
dust mites. Exposure to cockroaches and rodents is also
common in certain areas of the United States—such as the
Southeast, where cockroaches survive and breed indoors
and outdoors. Rodent exposure may be more common in
inner-city and rural areas. Strong evidence links indoor
mouse allergen exposure in homes and schools to wors-
ened asthma symptoms in sensitized children.
4-6
Sensitiza-
tion to these indoor allergens is associated with increasing
asthma severity and more frequent and severe exacerba-
tions (FIGURE 1
7-9
). For school-age children in the Childhood
Asthma Management Program (CAMP) study, sensitization
and exposure to multiple allergens (mite, cat, dog, Alter-
naria fungi, and cockroach) made asthma worse. For US
inner-city children in the National Cooperative Inner-City
Asthma Study population, the most important indoor aller-
gens were cockroach and rat, and probably mice. Half of the
bedrooms of inner-city children had a high level of cock-
roach allergen.
7
Indoor allergen sensitization is known to be greater
among minority populations living in urban environments,
compared to non-Latino whites.
10,11
In particular, black and
Puerto Rican populations carry the highest risk of sensitiza-
tion to those allergens that are most associated with asthma
morbidity. African-American youth are more likely to have a
mouse and/or cockroach sensitization prole independently
associated with asthma exacerbations, acute care visits, and
hospitalizations, compared to non-Latino white youth. So
too, Puerto Rican and other Latino ethnic minorities are at
higher risk of mouse sensitization and attributable asthma
hospitalization compared to those of Mexican heritage.
10,11
is evidence highlights how a simple clinical risk strati-
cation and personalized approach may impact critical out-
comes among patients who shoulder disproportionate dis-
ease burden.
Although indoor allergens are of prime importance,
assessing sensitization to seasonal outdoor allergens can also
lead to improved outcomes. Associations exist between peak
seasonal pollen and fungi levels and emergency department
(ED) visits for asthma exacerbations.
12
Additionally, asthma
exacerbations can increase dramatically after thunderstorms
that expose sensitized patients to electrostatically fractured
pollen and fungi.
13
How will knowing sensitization affect my practice?
Is effective therapy available?
When a person has conrmed sensitization, a history
of symptoms, and a reaction compatible with exposure,
2 approaches can be considered:
• Trigger allergen reduction, which has demonstrated
ecacy, especially in children
FIGURE 1 Aeroallergen sensitization and exposure to common allergens and
asthma severity and exacerbations
7-9
Cat Dog Mold Alternaria Mice/Rat Cockroach
Prednisone
Bursts
8 8 8
Urgent Care
Visits
8 8 7,9 7,9
Hospitalizations 8 8 8 8 7,9 7,9
Blue arrows show that, for school-age children, sensitization and exposure to multiple allergens, such as mite, cat, dog, Alternaria, and
cockroach, made asthma worse when they occurred together. Green arrows show that, for US inner-city children, the most important
indoor allergens were cockroach and rat, and probably mice.

S16
SEPTEMBER 2018
[
STEP 2: ALLERGEN EXPOSURE IN DAILY PRACTICE
]
• Targeted immunotherapy, which is not available
for all allergens but is eective in both children and
adults.
Effective exposure control measures
ere is evidence that multifaceted environmental control
measures are eective in reducing the burden of asthma,
but no specic combination of interventions has proved
more eective than others
14
(TABLE 1
15-20
). is evidence
strengthens the imperative to correctly and accurately
identify individual allergic sensitization so that appropriate
allergen control measures can be initiated.
Patients with asthma who have allergy testing are signi-
cantly more likely to employ preventive strategies (an asthma
plan, trigger avoidance, and medication adherence) and had
fewer days with allergy symptoms than patients who had not
been tested.
21
ese outcomes were supported by a study of
adults with moderately severe asthma,
22
who had an individ-
ualized plan, including environmental control based on the
results of allergy testing (FIGURE 2
22
).
What therapies are available?
e immunoglobulin E (IgE)-directed therapies include envi-
ronmental control, immunotherapy, and anti-IgE therapy
(omalizumab). Environmental control is the initial therapy;
particularly in children, simple changes have demonstrated
eectiveness.
A recent meta-analysis funded by the Agency for Health
Research and Quality (AHRQ) supports the value of identify-
ing allergen sensitization to guide potential immunotherapy,
23
which may play an increasing role in allergy and asthma man-
agement with the availability of US Food and Drug Adminis-
tration-approved sublingual immunotherapy (SLIT) for pol-
len and dust mite allergy. SLIT therapy is easy to administer,
has few potential risks, and can be done within primary care
practice. SLIT improves asthma symptoms, quality of life
(QoL), and FEV
1
, and reduces the use of long-term control
medications. It may also reduce the use of quick-relief medi-
cations. Local reactions to SLIT are common but only infre-
quently require a change in therapy. Systemic reactions are
so uncommon that home administration is recommended,
making this therapy convenient.
Subcutaneous immunotherapy (SCIT) reduces use of
long-term control medications and may also improve QoL
and lung function (eg, FEV
1
) and reduce the use of short-
acting bronchodilators and systemic corticosteroids. SCIT
oers more antigens but its use is limited by the need for
oce administration with monitoring, due to the potential
for systemic,potentially severe, reactions.
23
IDENTIFICATION OF
ALLERGIC SENSITIZATION
e diagnosis of clinically signicant sensitization requires
both history and testing conrmation.
24
e gold standard
for allergy diagnosis is the rarely used allergen exposure
challenge. While allergy evaluation begins with a history,
even with a structured history, allergy can be dicult to
diagnose accurately. A structured allergy history alone can
result in false-positives for perennial and seasonal allergens,
as outlined in FIGURE 3.
25
Combining history with diagnostic
Study Results
Parikh (2018)
15
For children with asthma hospital admissions, post-discharge referral for environmental mitigation
programs, as part of comprehensive discharge education, helped reduce the hospital readmission rate.
Murray (2017)
16
In children with asthma, a year-long study of dust mite-impermeable bed covers found a signicant
reduction in severe exacerbations requiring hospitalization, but no difference in exacerbations.
Rabito (2017)
17
In homes of children with asthma, a simple cockroach-specic intervention with insecticide bait
reduced asthma severity (eg, symptom burden), and modestly affected exacerbations.
Kercsmar (2006)
18
In children with asthma, home remediation of dampness and mold demonstrated a signicant reduction
in exacerbations.
Shirai (2005)
19
For people of all ages, a small (N=20) study of pet removal from homes of pet-allergic people with
asthma demonstrated signicant improvement, largely attributable to reduction in pet rodent or ferret
exposure, not exposure to cats or dogs.
Morgan (2004)
20
In inner-city children with asthma who were cockroach-sensitized, a multifaceted intervention, including
establishing an environmentally safe sleeping zone, signicantly reduced cockroach, dust mite, and
cat allergen exposures; signicantly reduced asthma symptom days and nights; and decreased missed
school days, emergency department visits, and unscheduled ofce visits. Signicantly reduced asthma
symptoms continued during the year after the study ended.
TABLE 1 Studies supporting environmental control measures
15-20
S17
SEPTEMBER 2018
[
STEP 2: ALLERGEN EXPOSURE IN DAILY PRACTICE
]
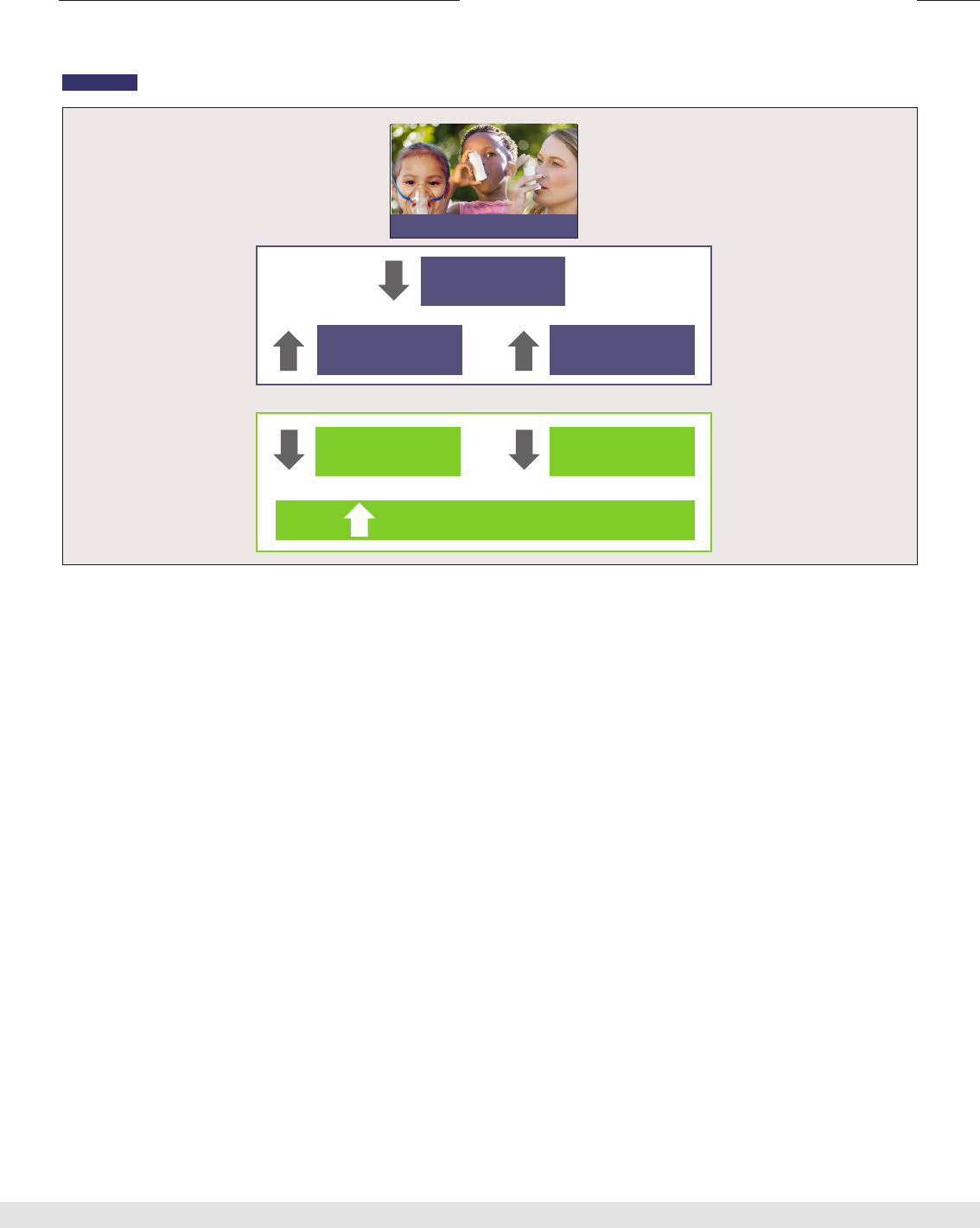
FIGURE 2 An individualized plan, including environmental control, improves asthma symptoms
22
An individualized self-management plan decreased rescue inhaler use and nighttime awakenings and increased quality of life (QoL) among
adults with asthma.
Adapted from: Janson et al. J Allergy Clin Immunol. 2009;123(4);840-846.
Indoor and
Outdoor Allergens
Inhaler
Technique
Medication
Adherence
Rescue Inhaler
Use
Nighttime
Awakenings
Increased Quality of Life
ACTIONS
RESULTS
testing “improves the accuracy of an assessment of allergic
status based on patient opinion or a structured allergy his-
tory alone.”
25
Carefully performed skin testing and modern
standardized in vitro testing have excellent specicity and
sensitivity in the setting of a clinical history suggestive of
allergic disease. ese tests are not meant to be screening
tests for large populations but rather to conrm or exclude
the diagnosis of allergic triggers in the setting of clinically
relevant symptoms.
How do I obtain the clinical history to suggest a
need for testing?
Several questionnaires are available to facilitate the assess-
ment of allergy history and to assist parents and patients,
with the highest priority for those with high asthma bur-
den as identied in the previous article: frequent exacer-
bations, high symptom burden, step-4 or step-5 asthma
therapy, and for preschool children when parents want
to better understand the risk of continuing asthma. e
Asthma APGAR
26
tool combines an asthma “control score,”
a review of asthma medication adherence, patients’ per-
ception of their response to current therapy, and a short
list of common triggers (FIGURE 4). Question 4 of the
Asthma APGAR system is designed to begin a conversation
with patients and families regarding potential aeroallergen
sensitization. NAEPP guidelines also list questions that cli-
nicians can use to elicit a history.
3
Even without a specic asthma tool, 2 questions may
help initiate this important conversation:
• Do you know what is triggering your asthma, like
smoke, allergies, or cold air?
• Have you had any type of allergy testing in the past?
When the history is suggestive, it is appropriate to proceed
to allergen-specic testing.
What testing is available?
Skin testing, either skin prick or intradermal testing, is typi-
cally performed by an allergy specialist. Another method of
assessing sIgE sensitization is with in vitro diagnostic test-
ing. NAEPP guidelines present the advantages of the 2 types
of testing (TABLE 2).
3
Opinions on the comparative specic-
ity and sensitivity of skin testing and in vitro testing vary. In
general, they are comparable.
Patient

S18
SEPTEMBER 2018
[
STEP 2: ALLERGEN EXPOSURE IN DAILY PRACTICE
]
FIGURE 3 History plus diagnostic testing improves diagnostic accuracy
25
Diagnoses based on history alone (purple bars) tended to overestimate the occurrence of allergen sensitization. The history conrmed by
diagnostic IgE testing (blue bars) improved the accuracy of allergic status assessment.
Smith, el al. Is structured allergy history sufcient. J Allergy Clin Immunol 2009. 123 646-50.
!"#$%&#'()'*&+$,&$+"-'./#&(+0'1#'./#&(+0'23-'4/253(#&/,'6"#&/35
80
60
40
100
20
0
87%
53%
76%
54%
70%
40%
46%
37%
37%
15%
Dust
Mite
Grass
Pollen
Tree
Pollen
Cat
Dog
Results of Structured History vs History and Diagnostic Testing
History
History & Allergy Test Results
% of Patients
Which test do I order?
e American College of Allergy, Asthma & Immunology/
American Academy of Allergy, Asthma and Immunology
Specic IgE Test Task Force provides guidance regarding the
use of allergy testing.
ACAAI/AAAAI Joint Task Force Recommendation
Because most allergic patients are sensitized to multiple
allergens, the task of determining which ones are of major
importance is not a simple task. Because exposure to mul-
tiple allergens to which a patient is sensitized is likely to cre-
ate a synergistic effect, optimal management may require
identication and management for each of the relevant
allergens. Panels of tests designed for specic seasons and
geographical locations are available for this purpose.
27
e availability of preselected allergen proles greatly
simplies the task of choosing allergens for testing. For skin
testing, the allergist performing the testing is likely to use a
battery of common allergen substrates. For in vitro testing,
regional respiratory proles are available that include aller-
gens typical of the geographic region or those known to be
associated with allergic asthma. Including key regional aller-
gens maximizes test eciency without compromising the
utility of test results.
27
How do I interpret test results?
Skin-testing results are interpreted by the clinician supervis-
ing the testing. e referring physician or clinician should
receive a report outlining the allergens tested and the results
(positive or negative), based on the response to the allergen
in millimeters and compared to positive and negative con-
trols. Results can be used to guide avoidance or exposure
reduction, consideration of immunotherapy, and reassur-
ance when testing is negative.
In vitro testing is also used to conrm the history and to
guide therapy, which includes environmental control, aller-
gen avoidance and, if neither is possible or sucient, to con-
sider pharmacotherapy or immunotherapy. erefore, the
interpretation is based on evidence of sensitization (yes or
no). Sharing test results with patients can help them under-
stand the nature of their sensitization and target allergen-
control eorts. Similarly, sIgE test results are useful for rul-
ing out sensitization, sparing patients the eort and cost of
avoiding allergens that are not causing their symptoms.

S19
SEPTEMBER 2018
[
STEP 2: ALLERGEN EXPOSURE IN DAILY PRACTICE
]
FIGURE 4 Asthma APGAR questionnaire
26
Please circle your answers:
1. In the past 2 weeks, how many times did any breathing problems (such as asthma) interfere with your
ACTIVITIES or activities you wanted to do?
Never ( 0 ) 1 – 2 times ( 1 ) 3 or more times ( 2 )
2. How many DAYS in the past 2 weeks did you have shortness of breath, wheezing, chest tightness,
cough or felt you should use your rescue inhaler?
None ( 0 ) 1 – 2 DAYS ( 1 ) 3 or more DAYS ( 2 )
3. How many NIGHTS in the past 2 weeks did you wake up or have trouble sleeping due to coughing,
shortness of breath, wheezing, chest tightness or get up to use your rescue medication?
Never ( 0 ) 1 – 2 NIGHTS ( 1 ) 3 or more NIGHTS ( 2 )
4. Do you know what makes your breathing problems or asthma worse?
Yes No Unsure
• Please circle things that make your breathing problems or asthma worse
Cigarettes Smoke Cold Air Colds Exercise Dust Dust Mites
Trees Flowers Cats Dogs Mold Other:______________
• Can you avoid the things that make your breathing problems or asthma worse?
Seldom Sometimes Most of the times
5. List or describe medications you’ve taken for breathing problems or asthma in the past 2 weeks:
Remember you may use Nasal, Oral, or Inhaler medications.
Breathing or Allergy
Medication
When Taken? Reasons for taking
medication:
Reasons for not taking
medication:
Daily As needed
Daily As needed
Daily As needed
Daily As needed
6. When I use my breathing or asthma medication I feel?
Worse No Different A Little Better A Lot Better
A = Activities
P = Persistent
G = triGGers
A = Asthma medications
R = Response to therapy
P = Asthma Plan
L = Lung fuction
U = Use of inhaler
S = Steroids
Asthma APGAR
A
P
G
A
R

S20
SEPTEMBER 2018
[
STEP 2: ALLERGEN EXPOSURE IN DAILY PRACTICE
]
FIGURE 5 illustrates how sIgE results may be reported.
Specic IgE values >0.10 kU
A
/L indicate sensitization;
increasing values have been correlated with increased prob-
ability of symptoms. Ranking positive results from high to low
specic IgE values helps prioritize targets for environmental
control. In the sample report, the 3 highest sIgE values were
for ragweed, Alternaria, and dog dander. It may be appropri-
ate to focus on mold abatement and keeping the dog out of
the bedroom (creating a reduced-allergen sleeping environ-
ment) as reasonable rst steps in environmental control,
in this example. A nonsedating antihistamine could be pre-
scribed to control symptoms during seasons when outdoor
allergens are present. A double-blind, randomized controlled
trial found that cetirizine delayed or prevented development
of asthma in infants who were sensitized to grass pollen.
28
INCORPORATING ALLERGEN
TESTING INTO DAILY PRACTICE—MORE THAN
ORDERING THE TEST
Even when allergy testing is ordered, environmental con-
trol recommendations to address the results are often
overlooked. is may be a particular problem for primary
care health teams in which time and expertise on allergen
avoidance and control are limited. A study by Cabana and
colleagues evaluated barriers that pediatricians identied
as interfering with their ability to implement NAEPP guide-
lines.
29
Although broad environmental counseling was not
assessed, smoking cessation, 1 component of environmental
counseling, was assessed. Lack of time was the barrier most
often cited (by approximately 50% of respondents), followed
by lack of educational materials, lack of support sta, and
lack of reimbursement, all reported by more than 40% of the
pediatricians. It is likely that primary care practices experi-
ence similar barriers to addressing allergies in people and
families aected by asthma and allergies.
The time barrier
Time is a constant issue for enhancing care in clinical prac-
tice. For every activity added, some existing activity will have
Skin Testing In Vitro Testing
• Less expensive than in vitro testing
• Results are available within 30 min
• Equally sensitive as in vitro tests
• Results are visible to the patient; this may encourage
compliance with environmental control measures
• Does not require knowledge of skin testing technique
• Does not require availability of allergen extracts
• Can be performed on patients who are taking medications that
suppress the immediate skin test (antihistamines, antidepressants)
• No risk of systemic reaction
• Can be done for patients who have extensive eczema
TABLE 2 Advantages of skin testing and of in vitro testing
3
to be dropped or at least shortened. To minimize additional
time commitments related to trigger identication, allergy
assessment, and testing and teaching avoidance strategies,
primary care physicians and practices have tried several
methods with varying success. For patients with poorly con-
trolled asthma or disruptive exacerbations, referral to an
asthma specialist is possible. In other countries, respiratory
practice nurses help educate patients and families suering
the greatest asthma burden. Some large health care systems
in the United States have adopted similar systems staed
by registered nurses or nurse practitioners. Regrettably, not
FIGURE 5 Specic IgE test results
For this patient, Alternaria and dog dander should be the targets of
environmental control. A nonsedating antihistamine along with ex-
posure reduction methods for pollens, especially during ragweed
season, should also be considered.
Sample Report
Results kU
A
/L Reference Range
Ragweed IgE 23.55 <0.10 kU
A
/L
Alternaria alternata IgE 20.01 <0.10 kU
A
/L
Dog Dander IgE 6.87 <0.10 kU
A
/L
Orchard Grass IgE 1.23 <0.10 kU
A
/L
Bermuda Grass IgE 1.22 <0.10 kU
A
/L
Elm Tree IgE 0.94 <0.10 kU
A
/L
June/Kentucky Blue IgE <0.10 <0.10 kU
A
/L
Maple Tree IgE <0.10 <0.10 kU
A
/L
Oak Tree IgE <0.10 <0.10 kU
A
/L
Ash Tree IgE <0.10 <0.10 kU
A
/L
Birch Tree IgE <0.10 <0.10 kU
A
/L
Timothy Grass IgE <0.10 <0.10 kU
A
/L
Cockroach IgE <0.10 <0.10 kU
A
/L
D. farinae IgE <0.10 <0.10 kU
A
/L
D. pteronyssinus IgE <0.10 <0.10 kU
A
/L
Mouse Urine IgE <0.10 <0.10 kU
A
/L
Total IgE 76 <100 kU
A
/L

S21
SEPTEMBER 2018
[
STEP 2: ALLERGEN EXPOSURE IN DAILY PRACTICE
]
all of these programs include trigger and allergy assessment.
e Asthma APGAR system, which does include allergy
assessment, is linked to a care algorithm that suggests next
steps; practices using the system reported that “it saves time”
and improves both patient and practice asthma outcomes.
26
Staff support
In outpatient settings, few primary care clinics include a cer-
tied asthma educator who might have expertise in environ-
mental control. However, it may be possible (for example,
through www.naecb.com
30
) to nd a certied asthma educa-
tor in your area to support these activities and educate your
sta. Clinic sta usually includes only 1, if any, nurse and
several medical assistants, who likely have had no education
or training in environmental trigger avoidance. In some prac-
tices, lack of support may be managed by timely referral to an
allergist; however, most patients with asthma will never see
an asthma specialist. erefore, primary care practices need
support to become better-versed not only in allergy evalua-
tions but also in dealing with evaluation results through trig-
ger management. is requires sta education and access to
appropriate educational materials to share with the patient
and family.
A comprehensive systematic review of delivery of allergy
services noted that primary care physicians do not receive
structured instruction in allergy during their training, and
few may be familiar with treatment guidelines, yet it con-
cluded that many patients referred to specialists could be
FIGURE 6 Asthma disease-management pathways
34
Initial Evaluation
• History and physical (asthma severity assessed)
• Spirometry
• Allergy testing (for persistent asthma)
- In vitro sIgE testing or skin testing
• Medications prescribed
• Environmental control education (if applicable)
6-8 weeks
3 visits with not
well-controlled
or very poorly
controlled asthma
Missed
appointment
and asthma
uncontrolled
or very poorly
controlled at
last visit
Well-controlled
asthma or fewer
than 3 visits with
not well- or very
poorly controlled
asthma
Missed
appointment last
visit with well-
controlled asthma
and/
or
and/
or
Early follow-up
2-4 weeks
Regular follow-up
6-8 weeks
Allergy testing
and allergen
avoidance may
be performed
at the second or
third visit
Initial Evaluation
• History and physical (asthma control assessed)
• Spirometry
• Allergy testing (for persistent asthma)
- In vitro sIgE testing or skin testing
• Medications prescribed and adjusted
• Environmental control education (if applicable)
Republished with permission of American Journal of Managed Care from Kwong et al. Adaptation of an asthma management program to a small clinic. Am J Manag Care
2017;23(7):e231-e237. Permission conveyed through Copyright Clearance Center, Inc.

S22
SEPTEMBER 2018
[
STEP 2: ALLERGEN EXPOSURE IN DAILY PRACTICE
]
easily managed in primary care if clinicians were appropri-
ately trained.
31
e Physician Asthma Care Education (PACE)
program demonstrated that interactive training for primary
care physicians improved their patients’ outcomes—spe-
cically, asthma care plans, frequency of days with asthma
symptoms, and ED utilization.
32
Access to the PACE program
is available for primary care clinicians and practices, and
group PACE programs may be available in your area.
33
A simple plan for asthma ofce visits
Health-care professionals value clinically meaningful, patient-
centered outcomes (frequency and severity of asthma symp-
toms, level of asthma control, QoL), as well as prudent resource
utilization (fewer ED visits for asthma, fewer hospitalizations,
fewer exacerbations). Instituting a simple plan for an initial
asthma evaluation and follow-up visits, such as shown in
FIGURE 6, may help sta manage patients more eciently.
34
e pathways are adaptable to small and large practices and
achieved good asthma outcomes on a sustainable basis. Repeat
or follow-up visits are usually necessary to review key asthma
education points and rene an asthma management plan.
Referring patients to allergy specialists
A percentage of patients require referral for subspecialty
care. Further work is needed to understand better meth-
ods for expediting referral and ensuring that primary care–
specialty care communication is timely and bidirectional.
35,36
According to a survey of pediatricians, they consider refer-
ral if a child has severe persistent asthma or a single life-
threatening asthma event.
36
e top 2 reasons for referral
were poor asthma control and unclear diagnosis. ere has
been increasing use of electronic consultation (eConsult)
services to improve communication and access to subspe-
cialists.
37
Initial evaluations also point to improved primary
care satisfaction with this approach.
38
ere is limited work in
assessing the potential eectiveness of eConsults in improv-
ing allergen screening, counseling, management, and patient
outcomes.
PATIENT ENGAGEMENT
Self-assessment
Given the limited time for patient clinic visits in primary
care settings, there is a need to develop more ecient ways
for health care providers to interact with patients
39
and
counsel patients about how to avoid allergen exposure.
Using a simple form that the patient completes prior to the
clinician encounter can provide important information
when considering allergy testing and making avoidance
recommendations. e Asthma APGAR was developed by
and within primary care practices and, in a large study,
improved patients’ asthma outcomes and the practice’s
guideline-concordant care.
26
Available materials
Many of the written asthma trigger management materials
that are readily available are not culturally appropriate or at
the recommended reading level (at or below the 5
th
-grade
level for the general US population).
40,41
Beyond general liter-
acy concerns, materials may also require high health-literacy
levels to read and understand. Of the trigger-management
materials, many include multiple pages, cannot be tailored
to the individual patient’s needs, and are often written at a
10th- to 12th-grade reading level. Consequently, patients
may never read or understand the materials they receive.
Considering the importance of patient literacy levels for
written materials, it may be useful to assess literacy using a
simple and validated tool called Quick Assessment of Literacy
in Primary Care: e Newest Vital Sign,
42
* Practices that care
for non-English-speaking patients must also consider assess-
ment of materials in other required languages.
*Available at www.ncbi.nlm.nih.gov/pmc/articles/PMC1466931.
Patient education
Patient education will be dicult and likely unsuccessful if
primary health care team members are not well versed and
comfortable providing evidence-based recommendations for
trigger avoidance. Straightforward, concise educational mod-
ules on avoidance counseling should be available, includ-
ing “user-friendly, systematic and step-wise techniques and
tools for evaluation of a patient’s environmental exposures.”
43
FIGURE 7 presents a sample of environmental control rec-
ommendations for dust mites that can be reviewed with the
patient and taken home. is and other examples of patient
education materials for allergen environmental control and
avoidance can be found in the supplementary material.
New technology: apps and video
e ubiquity of smart phones and apps has provided mobile
health with platforms to access patients and monitor patient
data in real-time. ese platforms might also be useful for
asthma education, and to help patients identify triggers or be
aware of real-time environmental changes (eg, with air qual-
ity or air pollution). Regrettably, a review of over 100 asthma
apps noted that none “combined reliable, comprehensive
information about the condition with supportive tools for
self-management.”
44
In addition, another review noted that
“apps for asthma lack clinical evaluation and are often not
based on medical guidelines.”
45
Further work is needed to
understand how these technologies could improve allergen
control and asthma outcomes.

S23
SEPTEMBER 2018
[
STEP 2: ALLERGEN EXPOSURE IN DAILY PRACTICE
]
Video applications that are tailored to a specic prac-
tice or group of practices allow physicians or nursing sta to
pre-record short messages for patients on a variety of top-
ics, such as use of daily and quick-relief inhalers, inhaler
instructions for each of the inhaler types, and messages
about triggers. Messages are recorded once and made avail-
able to patients via several online formats. is system has
several advantages:
• Messages come from the patient’s care team
• Messages can be used over and over by patients
• Messages are available in the clinic and at home.
CONCLUSIONS
Asthma continues to be a signicant burden for patients,
families, health care systems, schools, employers, and
health-care insurers and payers. To date, implementation of
existing guidelines has been modest and focused on medi-
cations, with limited emphasis on identifying triggers or
allergens that impede eorts to control asthma symptoms
and to decrease the burden for everyone. More than 90%
of US households harbor potential asthma triggers.
46
Sim-
plifying the process for clinicians to identify patients who
would benet from allergy testing, using an environmental
questionnaire, will increase the number of patients receiv-
ing allergy testing. Providing patient-friendly educational
materials using only the individual patient’s recommenda-
tions at an appropriate literacy level will increase the likeli-
hood of the patient taking steps to improve the environment
as related to asthma triggers.
Implementation of trigger testing and environmental con-
trols has been successful at Little River Medical Center
in South Carolina for several reasons. First, aeroallergen
blood testing is simple and can be ordered during routine
appointments. Whereas spirometry and trigger testing once
required specialist referrals, both can now be done in the
primary care setting.
Second, it’s a team effort with nursing staff supporting
the physicians. Nurses document symptoms, explain and
monitor inhaler technique, and educate about positive trig-
gers. Peer chart reviews also track the use of controller
medications and asthma action plans.
Third, there is continuity of care. Regular follow-up visits
allow therapy to be individualized and adjusted based on
current symptoms and asthma control. Rather than seeing
patients only during acute crises, the medical team uses
regular appointments to educate patients and families so
that they can avoid asthma exacerbations. This fosters con-
tinued patient engagement and reinforces the recommenda-
tions in the asthma action plan. l
FIGURE 7 Sample of practical environmental control measures*
Your child [___________________________________________________________] is allergic to the checked items. Taking the
recommended steps listed below will help reduce his/her allergy and asthma symptoms.
Date tested:__________________________ Date reviewed____________________________ by__________________________________
o Dust Mites—Present All Year
• Dust mites are sensitive to light and can pull their water out of humid air. They like to burrow down into upholstered furniture,
carpeting, mattresses, pillows, and stuffed animals.
• Your child’s bedroom should be addressed rst, then the rest of the house.
—Put dust-proof casings on pillows and mattresses where your child sleeps.
—Wash bedding weekly, in hot (130°F) water, if possible.
—Avoid heavy drapery and use vinyl blinds or washable curtains.
—Reduce dust catchers, especially in the bedroom (books, stuffed animals, etc.).
— Vacuum and dust thoroughly when your child is not present. This can be done once a week unless there is a reason to vacuum
more often.
—Use a vacuum with a HEPA lter or double-layered bag if possible.
—If possible, remove carpeting, at least from the bedroom. Floors that can be swept or mopped are best.
*Developed and used in practice by Christine W. Wagner, APRN, MSN, AE-C. Only the dust mite section of the complete handout is shown here.

S24
SEPTEMBER 2018
[
STEP 2: ALLERGEN EXPOSURE IN DAILY PRACTICE
]
REFERENCES
1. Institute of Medicine Committee on the Assessment of Asthma and Indoor Air. Di-
vision of Health Promotion and Disease Prevention. Clearing the Air: Asthma and
Indoor Air Exposures. Washington, DC: e National Academies Press; 2000.
2. Kanchongkittiphon W, Mendell MJ, Gan JM, Wang G, Phipatanakul W. Indoor en-
vironmental exposures and exacerbation of asthma: an update to the 2000 review by
the Institute of Medicine. Environ Health Perspect. 2015;123(1):6-20.
3. National Asthma Education and Prevention Program (NAEPP). Guidelines for the di-
agnosis and management of asthma (EPR-3). www.nhlbi.nih.gov/health-pro/guide-
lines/current/asthma-guidelines/full-report. Accessed June 28, 2018: [see pages 169,
187, and 188].
4. Matsui EC, Eggleston PA, Buckley TJ, et al. Household mouse allergen exposure and
asthma morbidity in inner-city preschool children. Ann Allergy Asthma Immunol.
2006;97(4):514-520.
5. Ahluwalia SK, Peng RD, Breysse PN, et al. Mouse allergen is the major allergen of
public health relevance in Baltimore City. J Allergy Clin Immunol. 2013;132(4):830-
835.e1-e2.
6. Sheehan WJ, Permaul P, Petty CR, et al. Association between allergen exposure
in inner-city schools and asthma morbidity among students. JAMA Pediatr.
2017;171(1):31-38.
7. Rosenstreich DL, Eggleston P, Kattan M, et al. e role of cockroach allergy and ex-
posure to cockroach allergen in causing morbidity among inner-city children with
asthma. New Engl J Med. 1997;336(19):1356-1363.
8. Nelson HS, Szeer SJ, Jacobs J, Huss K, Shapiro G, Sternberg AL. e relationships
among environmental allergen sensitization, allergen exposure, pulmonary func-
tion, and bronchial hyperresponsiveness in the Childhood Asthma Management
Program. J Allergy Clin Immunol. 1999;104(4 Pt 1):775-785.
9. Perry T, Matsui E, Merriman B, Duong T, Eggleston P. e prevalence of rat allergen in
inner-city homes and its relationship to sensitization and asthma morbidity. J Allergy
Clin Immunol. 2003;112(2):346-352.
10. Yang JJ,BurchardEG, Choudhry S, et al. Dierences in allergic sensitization by self-
reported race and genetic ancestry. J Allergy Clin Immunol. 2008;122(4):820-827.
11. Fishbein AB, Lee TA, Cai M, et al. Sensitization to mouse and cockroach allergens
and asthma morbidity in urban minority youth: Genes-environments and admixture
in Latino American (GALA-II) and Study of African-Americans, Asthma, Genes, and
Environments (SAGE-II). Ann Allergy Asthma Immunol. 2016;117(1):43-49.e41.
12. Reid MJ, Moss RB, Hsu YP, Kwasnicki JM, Commerford TM, Nelson BL. Seasonal
asthma in northern California: allergic causes and ecacy of immunotherapy. J Al-
lergy Clin Immunol. 1986;78(4 Pt 1):590-600.
13. Wark PA, Simpson J, Hensley MJ, Gibson PG. Airway inammation in thunderstorm
asthma. Clin Exp Allergy. 2002;32(12):1750-1756.
14. Leas BF, D’Anci KE, Apter AJ, et al. Eectiveness of indoor allergen reduction in man-
agement of asthma. Comparative Eectiveness Review No. 201. (Prepared by the
ECRI Institute–Penn Medicine Evidence-based Practice Center under Contract No.
290-2015-0005-I.) AHRQ Publication No. 18-EHC002-EF. Rockville, MD: Agency for
Healthcare Research and Quality; February 2018. https://eectivehealthcare.ahrq.
gov/topics/asthma-nonpharmacologic-treatment/final-report-indoor-allergen-
reduction. Accessed June 29, 2018.
15. Parikh K, Hall M, Kenyon CC, et al. Impact of discharge components on readmission
rates for children hospitalized with asthma. J Pediatr. 2018;195:175-182.e2.
16. Murray CS, Foden P, Sumner H, Shepley E, Custovic A, Simpson A. Preventing severe
asthma exacerbations in children: a randomized trial of mite-impermeable bedcov-
ers. Am J Respir Crit Care Med. 2017;196(20:150-158.
17. Rabito FA, Carlson JC, He H, Werthmann D, Schal C. A single intervention for cock-
roach control reduces cockroach exposure and asthma morbidity in children. J Al-
lergy Clin Immunol. 2017;140(2):565-570.
18. Kercsmar CM, Dearborn DG, Schluchter M, et al. Reduction in asthma morbidity in
children as a result of home remediation aimed at moisture sources. Environ Health
Perspect. 2006;114(10):1574-1580.
19. Shirai T, Matsui T, Suzuki K, Chida K. Eect of pet removal on pet allergic asthma.
Chest. 2005;127(5):1565-1571.
20. Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental
intervention among urban children with asthma. N Engl J Med. 2004;351(11):1068-
1080.
21. Stingone JA, Claudio L. Disparities in allergy testing and health outcomes among ur-
ban children with asthma. J Allergy Clin Immunol. 2008;122(4):748-753.
22. Janson SL, McGrath KW, Covington JK, Cheng SC, Boushey HA. Individualized
asthma self-management improves medication adherence and markers of asthma
control. J Allergy Clin Immunol. 2009;123(4):840-846.
23. Lin SY, Azar A, Suarez-Cuervo C, Diette GB, et al. Role of immunotherapy in the
treatment of asthma. Comparative Eectiveness Review No. 196 (Prepared by the
Johns Hopkins University Evidence-based Practice Center under Contract No.290-
2015-00006-I). AHRQ Publication No. 17(18)-EHC029-EF. Rockville, MD: Agency for
Healthcare Research and Quality. March 2018. https://eectivehealthcare.ahrq.gov/
topics/asthma-immunotherapy/research. Accessed June 29, 2018.
24. Williams PB, Ahlstedt S, Barnes JH, Söderstrom L, Portnoy J. Are our impressions of
allergy test performances correct? Ann Allergy Asthma Immunol. 2003;91(1):26-33.
25. Smith HE, Hogger C, Lallemant C, Crook D, Frew AJ. Is structured allergy history suf-
cient when assessing patients with asthma and rhinitis in general practice? J Allergy
Clin Immunol. 2009;123(3):646-650.
26. Yawn BP, Wollan PC, Rank MA, Bertram SL, Juhn Y, Pace W. Use of Asthma APGAR
tools in primary care practices: a cluster-randomized controlled trial. Ann Fam Med.
2018;16(2):100-110.
27. Cox L, Williams B, Sicherer S, et al; American College of Allergy, Asthma and Im-
munology Test Task Force; American Academy of Allergy, Asthma and Immunology
Specic IgE Test Task Force. Pearls and pitfalls of allergy diagnostic testing: report
from the American College of Allergy, Asthma and Immunology/American Academy
of Allergy, Asthma and Immunology Specic IgE Test Task Force. Ann Allergy Asthma
Immunol. 2008;101(6):580-592.
28. Warner JO; ETAC Study Group. Early Treatment of the Atopic Child. A double-
blinded, randomized, placebo-controlled trial of cetirizine in preventing the onset
of asthma in children with atopic dermatitis: 18 months’ treatment and 18 months’
posttreatment follow-up. J Allergy Clin Immunol. 2001;108(6):929-937.
29. Cabana MD, Rand CS, Becher OJ, Rubin HR. Reasons for pediatrician nonadherence
to asthma guidelines. Arch Pediatr Adolesc Med. 2001;155(9):1057-1062.
30. National Asthma Educator Certication Board. Find a certied asthma educator.
www.naecb.com. Accessed 18 June 2018.
31. Diwakar L, Cummins , Lilford R, Roberts T. Systematic review of pathways for the de-
livery of allergy services. BMJ Open. 2017;7(2):e012647.
32. Cabana MD, Slish KK, Evans D, et al. Impact of physician asthma care education on
patient outcomes. Pediatrics. 2006;117(6):2149-2157.
33. National Institutes of Health. National Heart, Lung, and Blood Institute. e PACE
curriculum. www.nhlbi.nih.gov/health-pro/resources/lung/physician-asthma-care-
education/curriculum.htm. Accessed June 29, 2018.
34. Kwong KY, Redjal N, Scott L, Li M, obani S, Yang B. Adaptation of an asthma man-
agement program to a small clinic. Am J Manag Care. 2017;23(7):e231-e237.
35. Ryan D, Gerth van Wijk R, Angier E, et al. Challenges in the implementation of the
EAACI AIT guidelines: A situational analysis of current provision of allergen immu-
notherapy. Allergy. 2018;73(4):827-836.
36. Poowuttikul P, Kamat D, omas R, Pansare M. Asthma consultations with special-
ists: what do the pediatricians seek? Allergy Asthma Proc. 2011;32(4):307-312.
37. Keely EJ, Archibald D, Tuot DS, Lochnan H, Liddy C. Unique educational opportuni-
ties for PCPs and specialists arising from electronic consultation services. Acad Med.
2017;92(1):45-51.
38. Liddy C, Afkham A, Drosinis P, Joschko J, Keely E. Impact of and satisfaction with a
new eConsult service: a mixed methods study of primary care providers. J Am Board
Fam Med. 2015;28:394-403.
39. Smith H, Horney D, Goubet S, et al. Pragmatic randomized controlled trial of a struc-
tured allergy intervention for adults with asthma and rhinitis in general practice. Al-
lergy. 2015;70(2):203-211.
40. e Joint Commission. Advancing Eective Communication, Cultural Competence,
and Patient- and Family-Centered Care: A Roadmap for Hospitals. www.jointcom-
mission.org/assets/1/6/ARoadmapforHospitalsnalversion727.pdf. Oakbrook Ter-
race, IL: e Joint Commission; 2010. Accessed June 29, 2018.
41. Centers for Disease Control and Prevention. Healthy People 2010. Objective 11-2
data. htpp://wonder.cdc.gov/data2010/focus.htm. Accessed June 29, 2018.
42. Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the
newest vital sign. Ann Fam Med. 2005;3(6):514-522.
43. National Institutes of Health. National Heart, Lung. and Blood Institute. Guidelines
Implementation Panel Report for: Expert Panel Report 3—Guidelines for the diagno-
sis and management of asthma. Washington, DC: U.S. Dept. of Health and Human
Services; December 2008:32.
44. Huckvale K, Car M, Morrison C, Car J. Apps for asthma self-management: a system-
atic assessment of content and tools. BMC Med. 2012;10:144.
45. Tinschert P, Jakob R, Barata F, Kramer JN, Kowatsch T. e potential of mobile apps
for improving asthma self-management: a review of publicly available and well-ad-
opted asthma apps. JMIR Mhealth Uhealth. 2017;5(8):e113.
46. Salo PM, Wilkerson J, Rose KM, et al. Bedroom allergen exposures in US households.
J Allergy Clin Immunol. 2018;141(5):1870-1879.e14.
Regulatory approval code: 52115.AL.US1.EN.v1.18

S25
AUGUST 2018
Integrating Allergic Trigger Management into
Primary Care Asthma Management:
Step 3: A Signicant Opportunity for Payers
and Health Systems
Randall Brown, MD, MPH, AE-C; Suzanne Madison, PhD; Len Fromer, MD, FAAFP;
Brad Lucas, MD; Steve Clark; Michael D. Cabana, MD, MPH; Christine W. Wagner, APRN, MSN, AE-C;
Barbara P. Yawn, MD, MSc, FAAFP.
DISCLOSURES
Dr. Brown reports that he is on the Board of Directors for Allergy
and Asthma Network; an advisor and speaker for AstraZeneca; a
speaker for Circassia Pharmaceuticals plc; a speaker for Integrity
Continuing Education Inc.; an advisor for Novartis AG; a speaker
for Teva Pharmaceutical Industries Ltd.; and an advisor for Thermo
Fisher Scientific.
Dr. Madison has no conicts to disclose.
Dr. Fromer has been a consultant and speaker for Thermo Fisher
Scientic in the recent past.
Dr. Lucas has no conflict to disclose.
Steve Clark has no conflict to disclose.
Dr. Cabana is on the Merck Speakers' Bureau and consults with
Novartis AG, Genentech, Inc., and Thermo Fisher Scientic.
Christine W. Wagner has an ongoing relationship with Thermo
Fisher Scientic.
Dr. Yawn is a paid consultant and has an ongoing relationship with
Thermo Fisher Scientic.
ACKNOWLEDGEMENT
The Task Force appreciates the editorial support provided
by Sarah Staples, whose work was nancially supported by
Thermo Fisher Scientic. The Task Force also acknowledges and
appreciates the important logistical support provided by Kevin H.
TenBrink and Gabriel Ortiz of Thermo Fisher Scientic.
I
n the rst 2 articles, we presented the evidence for aero-
allergen impact on asthma and the need to identify the
people most likely to benet from allergic trigger evalu-
ation (TABLE 1). Next, we outlined the available methods to
evaluate and conrm aeroallergen sensitization, as well as
appropriate evidence-driven prevention and treatment strat-
egies. Despite this knowledge and the available tools, most
people with asthma do not receive an allergy assessment as
part of their asthma management.
1
Integrating aeroallergen
evaluation and trigger management into practice is often
met with barriers. is article focuses on innovative ways of
overcoming the system-wide barriers to delivering excellent
asthma care.
Kim is an African-American woman who has self-identied
several possible “allergies” that she admittedly self-treats.
On her previous visit, she agreed to conrm her aeroaller-
gen sensitivities and you ordered a panel of “allergy blood
tests.” You are aware that she is a member of a racial group
historically known for being at higher risk of asthma-related
morbidity and mortality than non-Hispanic Caucasian adults.
Today, you begin by reviewing Kim’s Asthma APGAR
score, which has fallen from 6 to 4 with fewer episodes of
missed or modied activities that she thinks are a result of
using her current medications more regularly. But she still
reports both days and nights with asthma symptoms. She is
taking her “regular” inhaler and shows you the inhaled corti-
costeroid/long-acting beta agonist (ICS/LABA) combination,
TABLE 1 Patients in need of an allergy evaluation
Patients of any age experiencing a high asthma burden or
high risk despite treatment.
• An asthma-related hospitalization or 2 or more emergency
department visits
• Step 4 or higher medication regimen
• Potential candidate for biologics
Young children with recurrent cough/wheeze symptoms to
help predict the likelihood of asthma persistence beyond
6 years.
Patients of any age meeting the asthma “Rules of 2”*criteria
while on therapy.
• >2 days/week of asthma symptoms or quick relief inhaler use
• >2 nights/month of nighttime asthma symptoms
• ≥2 asthma exacerbations/year (episodes resulting in a burst of
oral steroids) or >2 albuterol rescue inhaler lls/rells per year
*Rules of Two
®
is a registered trademark of Baylor Health Care System. Adapted
from: Millard et al. Proc (Bayl Univ Med Cent). 2014;27(2):79-82.
S25
SEPTEMBER 2018

S26
SEPTEMBER 2018
[
STEP 3: OPPORTUNITY FOR PAYERS AND HEALTH SYSTEMS
]
FIGURE 1 Data can drive both transparency and performance
but says she still needs to use the quick-relief medication (a
short-acting beta agonist) several times a week. You also see
that the medical assistant reports that Kim’s inhaler tech-
nique for the dry-powder inhaler ICS/LABA combination is
much better—adequate, today.
You and Kim discuss her allergic sensitization results,
noting that she has signicant levels on at least 4 of the aller-
gens that were tested, including dust mites, cockroaches,
grass pollen, and mold. You discuss how exposure to these
triggers may be affecting her asthma and, at least in part,
may explain her problems with frequent symptoms and
“asthma attacks.”
Health systems and payers serve large patient popu-
lations and patients are generating information that can
improve their outcomes and reduce costs. Health care is
moving toward an integrated system, in which data are avail-
able across stakeholders, including multiple health care sys-
tems, patients, pharmacies, and other health care resources,
to drive both transparency and performance (FIGURE 1).
Patient-oriented data can answer key questions: What are the
best treatments? What facilitates improved care? How can
quality and cost be balanced and managed? Where are there
gaps that require innovation? In fact, this publication arose
from a gap in asthma care identied by the National Heart
Lung and Blood Institute Guideline Implementation Panel:
Allergen and irritant exposure control was 1 of 6 priority mes-
sages designed to “close the disparity gap for quality asthma
care and to promote the principles of patient-centered care.”
2
OPPORTUNITIES FOR IMPROVING
POPULATION HEALTH
Learning from improved outcomes in other chronic dis-
eases, the use of “big data” or electronic population health
data to identify individual patients most likely to benet
from enhanced asthma care and allergy evaluation is war-
ranted. Population asthma outcomes and health-related
data can be produced for most health care clinics or sys-
tems. ese data may be used to initiate allergy assessment
and evaluation in response to the continuing large clinical,
family, and cost burden of asthma in the United States. Data
Real-time
Integrated
Patient-level
De-identied
Clinical &
Laboratory
Data
Integrated
Sub-population
Analytics
Physical
& Mental
Status
Cost &
Risk
Data
Consumer
Preference
Connected
Payers Care Providers Policy Setters Manufacturers Consumers

S27
SEPTEMBER 2018
[
STEP 3: OPPORTUNITY FOR PAYERS AND HEALTH SYSTEMS
]
or postviral cough. e prescription order
system can then be used to identify people
with asthma who have been prescribed 3
or more months of daily maintenance ther-
apy with an ICS/LABA combination or, for
younger children, a prescription for an ICS
at a moderate-to-high dosage or an ICS plus
montelukast. ese are patients with step-4
and step-5 asthma therapy, according to the
2007 asthma guidelines.
3
In the example in
FIGURE 2, of the 2.2 million people identied
with asthma, 819,000 meet the criteria for
high asthma burden and an allergy evalu-
ation. Of that group, 215,000 (26.3%) have
already had the evaluation. Using this type
of big data allows a focus on the high-risk
group (ie, 819,000 – 215,000 = 609,000) who
have not had the evaluation, rather than the
entire population of 2.2 million people with
asthma.
To make asthma care more ecient and
eective, some large health care organiza-
tions have embedded asthma assessment
tools into their electronic health records,
making them easily accessible during any
asthma visit. is has been done with the
Asthma Action Plan
4
and the Asthma APGAR
tool.
5
Making these tools available at point
of care has the potential to increase their
completion, even when the visit may be for
another problem, ensuring that asthma care
does not get lost in the rush of acute prob-
lems or other chronic diseases. Incorporation of the Asthma
APGAR tool, including its brief allergy/trigger assessment,
into the electronic health record resulted in increased use of
control and assessment for people of all ages with asthma.
5
Appropriate standardized queries and data reporting for-
mats, based on control assessments or billing codes for ED
or urgent-care visits, can be developed to alert clinicians of
at-risk patients as they are seen in the clinic. Care algorithms
and, possibly, even standing orders can be considered for
assessing, testing, or referring patients with potential allergy-
related asthma symptoms.
Using large clinical and population health data
6
and
basing identication on adverse outcomes is of interest to
health-care professionals and systems and to payers who
want to improve compliance with the triple aims of reduc-
ing utilization and cost burden, improving outcomes, and
enhancing patient and provider satisfaction—focused, in
this case, on the greatest use of expensive asthma-related
searching does not rely solely on individual clinicians’ skills,
interest, or available time to determine which patients are
candidates for further allergy assessment.
For example, patients with poorly controlled asthma
could be selected for allergy evaluation or more intensive
management (FIGURE 2). Because asthma control scores are
not yet widely used, other health care data can be used to
identify patients with asthma who have frequent exacerba-
tions, especially those resulting in costly, burdensome, and
disruptive visits to the emergency department (ED) or hos-
pitalizations—proxies for poor asthma control. Using billing
and ICD-10 (10th Revision of the International Classica-
tion of Diseases) codes, everyone with asthma can be iden-
tied. Dening those with “asthma” as patients with at least
2 visits in the past 18 months with an asthma code can help
limit the group to people most likely to have asthma, and not
those who may have had a “rule out” diagnosis or an asthma
code to justify short-term inhaler use for a respiratory event
FIGURE 2 Identifying patients in specic populations
A database search of patients with asthma can ag those who might benet from
allergy evaluation or more intensive management. The numbers here are based on
an exploratory review of data from a large health care system. The 2.2 million people
had 2 or more ICD-9 or ICD-10 asthma codes in an 18-month period. The 819,000
had either 2 or more asthma-related ED visits in a year, or an asthma hospitaliza-
tion, or were on step-4 or step-5 asthma therapy (eg, including a high-dosage ICS in
combination with other maintenance drugs).
Using Big Data to Identify Candidates
for Allergy Evaluation
2.2 Million people with asthma
819K with
indication of
poorly controlled
asthma
(candidates for
allergy evaluation)
215K with an
allergy visit
(already had
an allergy
evaluation)

S28
SEPTEMBER 2018
[
STEP 3: OPPORTUNITY FOR PAYERS AND HEALTH SYSTEMS
]
services.
Services such as ED visits and hospitalization are
coded within the billing and clinical data in almost all health
care facilities (FIGURE 3). erefore, the data can be used
to identify a group of patients appropriate for enhanced
asthma management, which, in many cases, should include
allergy assessment or evaluation. Pharmacy records can
also be searched to monitor step-4 and step-5 prescrib-
ing, as well as adherence to prescription lling and overall
costs.
Over time, information from large databases can also
be used to measure progress toward the triple-aim goals. In
FIGURE 3, the red graph lines represent an at-risk population
compared to a reference group (blue line). Using standard
search algorithms, these 2 populations can be compared
after various interventions to evaluate the eect the interven-
tions had on modifying risk and outcomes.
MAKING ASTHMA PART OF
IMPROVED HEALTH CARE
Delivering value
Asthma is a major driver of health care costs and is the most
common chronic disease of children and adolescents. e
prevalence of asthma has risen steadily over the past 20
years and is projected to continue rising, along with a rise in
asthma exacerbations, which may be triggered by aeroaller-
gens.
7,8
e US health care system is rapidly moving toward
a value-based structure related to 3 questions—the triple
aims:
• How do we improve outcomes?
• What is the patient experience in the care process?
• What is the population cost for a dened segment of
patients?
Delivering excellence in value-based asthma care is a
function of improving quality while containing cost. is is
a continuous process fed by real-world data, which lends
insight and helps to shape new, more successful approaches,
the results of which can then be measured.
Allergy-trigger testing for people with asthma uses
resources, but poorly controlled asthma is expensive in
terms of ED visits, hospitalizations (inpatient and inten-
sive care), and extended stays. A single case of uncontrolled
asthma can cost $5963 a year—double the cost for a patient
whose asthma symptoms are being controlled.
9
e invest-
ment in patient education about trigger avoidance is com-
pelling when viewed in light of the savings that could be
FIGURE 3 Database searching for care improvement opportunities
The red graph line represents utilization and cost for a group of at-risk patients compared to a reference population (blue line). The bright
red squares below identify groups of patients who are not meeting target clinical or utilization goals. Over time, as new management prac-
tices are introduced, the impact of those practices can be seen by comparing the 2 groups again.

S29
SEPTEMBER 2018
[
STEP 3: OPPORTUNITY FOR PAYERS AND HEALTH SYSTEMS
]
achieved. To date, there has not been sucient belief that
asthma exacerbations are not only costly but also a sign of
health-system failure. Improved outcomes for patients and
populations will come when there is fuller buy-in from pay-
ers, accountable-care organizations, and health care sys-
tems that allergy evaluation and trigger management oer
an opportunity to dramatically improve clinical care and
lower costs.
Developing quality metrics
Care systems based on value rely on metrics, transparent and
valid measures designed to be used in performance score-
cards and compared to benchmarks of excellence. ere are
2 types of metrics in assessing asthma care: process and out-
comes. Each type is vitally important but must be shown to be
clinically important, have evidence of improving outcomes
and be easily measured. If signicant extra work is needed or
care ow is disrupted in collecting the metrics, their use will
not be sustained over time.
Currently, the only asthma quality metrics in wide-
spread use are the Healthcare Eectiveness Data and Infor-
mation Set (HEDIS) measures focused on medication use.
10
One measure is the percentage of patients with persistent
asthma who remained on their controller medications for
at least 75% of their treatment period. Another measure is
the ratio of controller medications to total asthma medica-
tions during the measurement year. Although measures of
medication use are important, there are other components
to asthma care that are important.
Allergy testing in asthma management of high-risk
individuals is a good example of a process metric that can be
derived from claims data (Current Procedural Terminology
codes for skin testing or specic immunoglobulin E) and
correlated with outcomes. Aeroallergen assessment in high-
risk patients (TABLE 1) should be considered for an updated
HEDIS or other quality metric to help guide this important
but often overlooked aspect of asthma management.
Regular clinician and team feedback can change prac-
tice behavior, especially when care teams are empowered
to deploy a workow model that incorporates tools and
resources to support the team, utilizing testing results to
teach the patient trigger avoidance. Ultimately, when pro-
cess metrics, such as appropriate trigger-testing rates, are
coupled to improvements in outcomes, such as decreased
urgent and emergent asthma interventions, and then
aligned with payment methodology for improved results,
signicant quality improvement in practice team care pat-
terns will be sustainable.
Quality metrics could help the clinicians and medical
directors who participate in value-based contracting under-
stand how to better align decision-making in clinical prac-
tice with the delivery of value to the patient, which emerges
clearly in the analysis of when and why to do allergy trigger
testing. e cost saving is going to be highest in groups with
high utilization of ED and hospital services for asthma, and
those with chronically poorly controlled asthma.
Addressing disparities
As with most chronic diseases, insurance coverage for basic
components, including allergy testing, is excellent. How-
ever, disparity in allergy and asthma care is plentiful in the
United States. Allergy and asthma disproportionately aect
children, adult women, the poor, African Americans, and
Americans of Puerto Rican descent.
11-18
Beyond what dis-
ease prevalence would predict, severe asthma morbidity
and asthma death are most striking among black and Puerto
Rican ethnic populations, in particular.
14,19,20
Given the com-
plexity of disparity sources and the admixture of American
society, health care professionals profess incomplete con-
dence in identifying and tackling these important issues
with diering populations in clinical care.
21
However, clini-
cians can address disparity through awareness and practi-
cal clinical approaches to allergen evaluation and asthma
management.
Understanding disparity
Disparity is multifactorial. Genetics may dene subpopula-
tion susceptibility as well as prevalence of disease, yet most
experts agree that, with standard-of-care clinical interven-
tion, allergies and asthma can be eectively diagnosed,
managed, and controlled in all patients.
13,22-24
Allergy-
associated asthma death rates that are considerably higher
among African Americans, Americans of Puerto Rican
descent, and other Latino ethnicities and economically dis-
advantaged populations, therefore, raise considerable dis-
parity concerns.
24-28
Researchers have described more than 30 evidence-
based causes for disparity in asthma and allergy man-
agement
25
(TABLE 2). Many factors may explain such dis-
parities, including environmental and genetic inuences.
Urban areas, which often have a predominance of African
American patients, are heavily concentrated with asthma
risk factors, such as air pollution, mice, cockroaches, dust
mites, poor diet, poverty, stress, and violence.
13,15,22,24
African
Americans are also less likely to receive National Institutes
of Health (NIH) guideline-directed care.
21,29
For example,
compared to whites, African Americans visit an asthma spe-
cialist less often, and use an ICS for persistent asthma less
frequently.
24,26
Clinicians can gain considerable disease-
management leverage by understanding the determinants

S30
SEPTEMBER 2018
[
STEP 3: OPPORTUNITY FOR PAYERS AND HEALTH SYSTEMS
]
of disparity and critically reviewing their own care delivery
model.
Working to minimize disparity in the clinical setting
So, how does one approach disparity in the clinical set-
ting? Clearly, change starts with clinical recognition that
such disparities exist, an obvious fact that is often missed.
Recent data suggest that African-American and some
Latino asthma patients who perceive health care discrimi-
nation are—independent of other asthma risk and socio-
economic status—at greater jeopardy for poor asthma con-
trol.
28
Promising patient strategies are on the horizon
30
and,
reassuringly, when clinicians are trained in cultural compe-
tence in addition to asthma care, their condence in using
better counseling and more eective patient-centered
approaches to asthma care are signicantly enhanced,
compared to standard asthma care training alone.
21
TABLE 3 summarizes practical approaches to removing dis-
parity when interacting with patients who have allergy or
asthma, or both.
THE NEED TO CLOSE THE CARE GAP
At its core, clinical care is about the clinician–patient relation-
ship and the provision of care that will lead to reduced symp-
toms and costs. Data collected on the delivery of the non-
medication elements of asthma care dene a signicant care
gap (TABLE 4).
1
Among 1176 patients with persistent asthma,
asthma triggers—specically, allergens—were assessed and
documented in only 32.5% of all patients.
1
Only 2% of patients
with persistent asthma had documented allergy test results.
The value of closing the care gap
A large integrated health network in southern California with
250,000 patients realized their asthma results (exacerbations,
hospitalizations, ED visits) were fair at best. e network
wanted to advance their performance beyond the HEDIS
metric of increasing the percentage of patients on a daily
controller medication to manage symptoms. e network
focused on 3 metrics. eir goal was to have the percentage
of patients who had a diagnosis of mild, moderate, or severe
persistent asthma, and who received the following care com-
ponents, exceed 90%:
• a controller medication;
• a written asthma plan;
• allergy testing.
e objective was to improve asthma care and realize
better patient outcomes as well as recover shared savings
bonuses from their value-based payer agreement. e net-
work acted on the evidence that engaging patients is eec-
tive when an asthma treatment plan, with a personalized
approach to medication use and allergic-trigger avoid-
ance, is used. e Asthma Action Plan from the American
Lung Association
4
is one such plan (see supplemental
materials).
e network achieved the goal of >90% compliance for
all 3 metrics within 6 months. e resulting decrease in ED
visits, hospitalizations, and urgent care and walk-in visits
resulted in a shared savings bonus that was signicantly
higher than the cost of trigger testing. is alignment of clin-
ical and nancial outcomes was very important because the
TABLE 2 Evidence-based determinants of asthma management disparities
25
Individual and Family Health Care Community Sociocultural and Political
• Cultural beliefs
• Depression
• Family dysfunction
• Genetic polymorphisms
• Health literacy
• Management of indoor
environments
• Medication adherence
• Nutrition and obesity
• Respiratory infections
• Social support
• Self-management skills
• Stress
• Cultural competence
• Health care access
• Health care nancing
• Quality of care
• Process of care
• Provider bias
• Provider-client communication
• Community stress
• Crowded living conditions
• Inadequate housing
• Neighborhood disadvantage
• Outdoor air pollution
• Social capital
• Social isolation
• Violence/crime
• Discrimination
• Employment
• Environmental justice
• Poverty
• Race
• Segregation
• Socioeconomic position
From Evans-Agnew RA. Health Promot Pract. 2018;19(2):213-221. © 2018 SAGE Publications, Inc. Reprinted by permission of SAGE Publications, Inc.

S31
SEPTEMBER 2018
[
STEP 3: OPPORTUNITY FOR PAYERS AND HEALTH SYSTEMS
]
predominant network reimbursement was a global capita-
tion rate.
ere is growing evidence that the use of acute care
resources can be reduced when patients are assessed for
specic IgE antibodies to aeroallergens. A recent study dem-
onstrated that IgE testing cut the hazard of another emer-
gency visit and corticosteroid treatment by half in patients
with mild persistent asthma (P<0.05).
31
Discharge referrals
for environmental mitigation have also reduced hospi-
tal readmissions.
32
ese interventions delivered value to
patients through improved quality of life and to health care
systems through decreased cost.
CONCLUSIONS
Overall, improved eciency in allergy testing and manage-
ment addresses an identied gap in asthma care intended
to improve quality of care, patient satisfaction, and value
for the health care system, as well as resource utilization.
Improved allergen evaluation, appropriateness for test-
ing referral, and follow-up education require system-wide
• Clearly communicate allergy and asthma risk to your patients and family; prudently screen, diagnose, and monitor for disease,
especially among high-risk groups
• Seek to understand how patient experience, environment, family, and culture may inuence allergy and asthma diagnosis and
management
• Plan a strategy with your patients that includes their opinions and concerns about disease, therapy, side effects, activity, and cost
• Regularly aim to improve cultural competence for your practice
• Regularly review samples of your practice’s cases of allergy and asthma diagnosis, management and control—especially from
populations that face disparity.
• Entertain multidisciplinary approaches to disparity reduction; consider aggressive patient education and supplemental assessment
and intervention (including at home, school, and work)
TABLE 3 A clinician’s allergy/asthma disparities to-do list
TABLE 4 Adherence to nonmedication elements of the asthma guidelines
1
Adherence, No. (%)
Elements of the
guidelines assessed
and documented
All
(N=1176)
Children
(5-11 years old)
(n=285)
Tweens
(12-18 years old)
(n=211)
Adults
(19-65 years old)
(n=680)
P value for
difference
across age
groups
P value for difference
across age groups,
adjusting for site using
random-effects model
Asthma control
Validated tool used
176 (15)
88 (7.50)
63 (22.1)
32 (11.2)
34 (16.1)
15 (7.1)
79 (11.6)
41 (6)
<.001 .03
Asthma medication
adherence discussed 390 (33.2) 90 (31.6) 68 (32.2) 232 (34.1) .71 .18
Inhaler technique
Taught
Observed
89 (7.6)
15 (1.3)
40 (14)
8 (2.8)
16 (7.6)
2 (0.9)
33 (2.8)
5 (0.7)
<.001
.20
>.002
<.001
Trigger/Irritants
Allergies discussed
Allergy testing
Patient smoking
status
Others smoking in
home
382 (32.5)
24 (2.0)
681 (76.3)
221 (18.8)
123 (43.2)
9 (2.8)
NA
97 (34)
69 (32.7)
6 (2.8)
115 (54.5)
47 (22.3)
190 (27.9)
9 (1.2)
566 (83.1)
77 (11.3)
<.001
.12
<.001
<.001
>.002
.19
<.001
<.001
Asthma action plan 37 (3.1) 25 (8.9) 5 (2.4) <.001 <.001
Reprinted from Yawn et al. Adherence to asthma guidelines in children, tweens, and adults in primary care settings: a practice-based network assessment. Mayo Clin Proc
2016;91(4):411-421. Used with permission.

S32
SEPTEMBER 2018
[
STEP 3: OPPORTUNITY FOR PAYERS AND HEALTH SYSTEMS
]
support. Gathering relevant patient information, quickly
assessing environmental issues, and providing counseling
are crucial in improving asthma outcomes.
After talking with Kim about her allergy test results, you
provide her with written materials that highlight practical
methods to avoid dust mite, mold, and cockroach triggers.
The materials are brief, have culturally appropriate word-
ing and illustrations, and can be shared with family and
friends. You also give her telephone numbers for advocacy
groups whose information you know is evidence-based,
as well as your ofce number. Being involved in personal-
izing the asthma management plan to her life experiences
is important to Kim, and plays a critical role in her desire
and ability to address the challenges of trigger avoidance
necessary to improve the health outcomes that are impor-
tant to her. l
REFERENCES
1. Yawn BP, Rank MA, Cabana MD, Wollan PC, Juhn YJ. Adherence to asthma guide-
lines in children, tweens, and adults in primary care settings: a practice-based
network assessment. Mayo Clin Proc. 2016;91(4):411-421.
2. National Institutes of Health, National Heart Lung and Blood Institute. Guide-
lines implementation panel report for: Expert Panel Report 3—guidelines for the
diagnosis and management of asthma: Partners putting guidelines into action.
Bethesda, MD: US Department of Health and Human Services; 2008 Dec. NIH
Publication Number 09-6147. www.nhlbi.nih.gov/guidelines/asthma/gip_rpt.
pdf. Accessed June 28, 2018.
3. National Asthma Education and Prevention Program (NAEPP). Guidelines for
the diagnosis and management of asthma (EPR-3). www.nhlbi.nih.gov/health-
pro/guidelines/current/asthma-guidelines/full-report. Accessed June 28, 2018.
4. American Lung Association. Asthma action plan. www.lung.org/assets/docu-
ments/asthma/asthma-action-plan.pdf. Accessed June 29, 2018.
5. Yawn BP, Wollan PC, Rank MA, Bertram SL, Juhn Y, Pace W. Use of Asthma AP-
GAR tools in primary care practices: a cluster-randomized controlled trial. Ann
Fam Med. 2018;16(2):100-110.
6. Accordini S, Corsico A, Cerveri I, et al. e socio-economic burden of asthma is
substantial in Europe. Allergy. 2008;63(1):116-124.
7. Loftus PA, Wise SK. Epidemiology of asthma. Curr Opin Otolaryngol Head Neck
Surg. 2016;24(3):245-249.
8. Hoch H, Liu A. Predicting and preventing asthma exacerbations. In: Personaliz-
ing Asthma Management for the Clinician, 1st ed. Szeer SJ, Holguin F, Wechsler
ME, eds. Atlanta, GA: Elsevier, Inc.; 2017:129-141.
9. Sullivan SD, Rasouliyan L, Russo PA, Kamath T, Chipps BE; TENOR Study Group.
Extent, patterns, and burden of uncontrolled disease in severe or dicult-to-
treat asthma. Allergy. 2007;62(2):126-133.
10. National Committee for Quality Assurance. Healthcare Eectiveness Data
and Information Set (HEDIS): Use of appropriate medications for people with
asthma and medication management for people with asthma. www.ncqa.org/
report-cards/health-plans/state-of-health-care-quality/2017-table-of-contents/
asthma. Accessed June 29, 2018.
11. Akinbami LJ,Moorman JE,Simon AE,Schoendorf KC. Trends in racial disparities
for asthma outcomes among children 0 to 17 years, 2001-2010. J Allergy Clin Im-
munol.2014;134(3):547-553.e5.
12. Centers for Disease Control and Prevention. 2016 National Health Interview Sur-
vey (NHIS) data: 2016 Lifetime asthma, current asthma, asthma attacks among
those with current asthmas. www.cdc.gov/asthma/nhis/2016/data.htm. Accessed
June 29, 2018.
13. Global Initiative for Asthma. 2018 GINA report, global strategy for asthma pre-
vention and management. https://ginasthma.org/2018-gina-report-global-strat-
egy-for-asthma-management-and-prevention/ Accessed June 29, 2018.
14. Zahran HS, Bailey CM, Damon SA, Garbe PL, Breysse PN. Vital signs: asth-
ma in children - United States, 2001-2016. MMWR Morb Mortal Wkly Rep.
2018;67(5):149-155.
15. Cardet JC, Louisias M, King TS, et al. Income is an independent risk factor for
worse asthma outcomes. J Allergy Clin Immunol. 2018;141(2):754-760.e3.
16. CooganPF, Yu J, O’ConnorGT,Brown TA, Cozier YC,Palmer JR,Rosenberg L.
Experiences of racism and the incidence of adult-onset asthma in the Black
Women’s Health Study. Chest.2014;145(3):480-485.
17. Clark NM, Gong ZM, Wang SJ, Lin X, Bria WF, Johnson TR. A randomized trial
of a self-regulation intervention for women with asthma. Chest. 2007;132(1):
88-97.
18. Centers for Disease Control and Prevention. 2015 National Health Interview
Survey (NHIS) data: Table 4-1. Current Asthma Prevalence Percents by Age,
United States: National Health Interview Survey, 2015. www.cdc.gov/asthma/
nhis/2015/table4-1.htm. Accessed June 29, 2018.
19. Mushtaq A. Asthma in the USA: the good, the bad, and the disparity. Lancet
Respir Med.2018;6(5):335-336.
20. Dwyer-Lindgren L,Bertozzi-Villa A,Stubbs RW,et al. Trends and patterns of dif-
ferences in chronic respiratory disease mortality among US counties, 1980-2014.
JAMA. 2017;318(12):1136-1149.
21. Patel MR, Song PXK, Bruzzese JM, et al. Does cross-cultural communication
training for physicians improve pediatric asthma outcomes? A randomized trial.
J Asthma. 2018:1-12.
22. Brown RW, Cappelletti CS. Reaching beyond disparity: safely improv-
ingasthmacontrol in the at-risk African-American population. J Natl Med As-
soc.2013;105(2):138-149.
23. Bryant-Stephens T. Asthma disparities in urban environments. J Allergy Clin Im-
munol. 2009;123(6):1199-1206.
24. Forno E, Celedón JC. Health disparities in asthma. Am J Respir Crit Care
Med.2012;185(10):1033-1035.
25. Evans-Agnew RA. Asthma disparity photovoice: e discourses of black ado-
lescent and public health policymakers. Health Promot Pract. 2018;19(2):
213-221.
26. WilliamsLK,Joseph CL,Peterson EL,et al. Patients withasthmawho do not ll
their inhaled corticosteroids: a study of primary nonadherence. J Allergy Clin Im-
munol.2007;120(5):1153-1159.
27. Yang JJ,BurchardEG, Choudhry S, et al. Dierences in allergic sensitization by
self-reported race and genetic ancestry. J Allergy Clin Immunol. 2008;122(4):
820-827.
28. akur N, Barcelo NE, Borrell LN, et al. Perceived discrimination associated with
asthma and related outcomes in minority youth: the GALA II and SAGE II stud-
ies. Chest. 2017;151(4):804-812.
29. Mitchell SJ, Bilderback AL, Okelo SO. Racial disparities in asthma morbid-
ity among pediatric patients seeking asthma specialist care. Acad Pedi-
atr.2016;16(1):64-67.
30. Baptist AP, Islam N, Joseph CL. Technology-based interventions for asthma-can
they help decrease health disparities? J Allergy Clin Immunol. 2016;4(6):1135-
1142.
31. Brock J. Acute Blood Allergy Testing Associated with Fewer Pediatric Asthma
Hospitalizations. P957. Presented at: the American oracic Society; May 18-23,
2018; San Diego, CA.
32. Parikh K, Hall M, Kenyon CC, et al. Impact of Discharge Components on Re-
admission Rates for Children Hospitalized with Asthma. J Pediatr. 2018 DOI:
https://doi.org/10.1016/j.jpeds.2017.11.062 [Epub ahead of print]
Regulatory approval code: 52195.AL.US1.EN.v1.18
